

Background: Psoriatic arthritis (PsA) is a multisystem inflammatory disease associated with accelerated atherosclerosis and increased cardiovascular (CV) risk. Research indicates that patients with PsA, particularly those with moderate to severe skin involvement, are at an even greater risk of adverse CV events. To assess the extent of skin involvement, the Psoriasis Area and Severity Index (PASI), a widely recognized method, is utilized. This involvement reflects underlying systemic inflammation, which contributes to immune cell activation and the secretion of pro-inflammatory cytokines. These processes may potentially alter ventricular geometry and be associated with both diastolic and systolic dysfunction.
Objectives: Evaluate the relationship between active skin involvement and carotid plaque (CP) as well as alterations in the left ventricle’s geometry, diastolic function, and systolic function in patients with PsA.
Methods: We conducted a cross-sectional and comparative study that included PsA patients aged 35 to 75 years who met the 2006 CASPAR criteria. Patients with prior CV disease, pregnancy, and overlap syndrome were excluded. Patients were classified based on their skin involvement as active (PASI > 1) or inactive (PASI ≤ 1). Ultrasound measurements were performed using B-mode ultrasonography; the presence of CP was defined as diffuse carotid intima-media thickness (cIMT) ≥1.2 mm or focal thickness ≥0.5 mm and carotid hyperplasia was determined by an increased cIMT (≥0.8mm). Echocardiographic measurements were made using B-mode, M-mode, Spectral Doppler, Color Doppler, and Tissue Doppler Imaging; cardiac geometry, diastolic function, and systolic function were classified according to the 2016 ASE/EACVI criteria. The normality was assessed with the Kolmogorov-Smirnov test. Comparisons were performed using the Student’s T-test, Chi-square test, and Mann-Whitney U test, accordingly. A p-value of ≤0.05 was considered statistically significant.
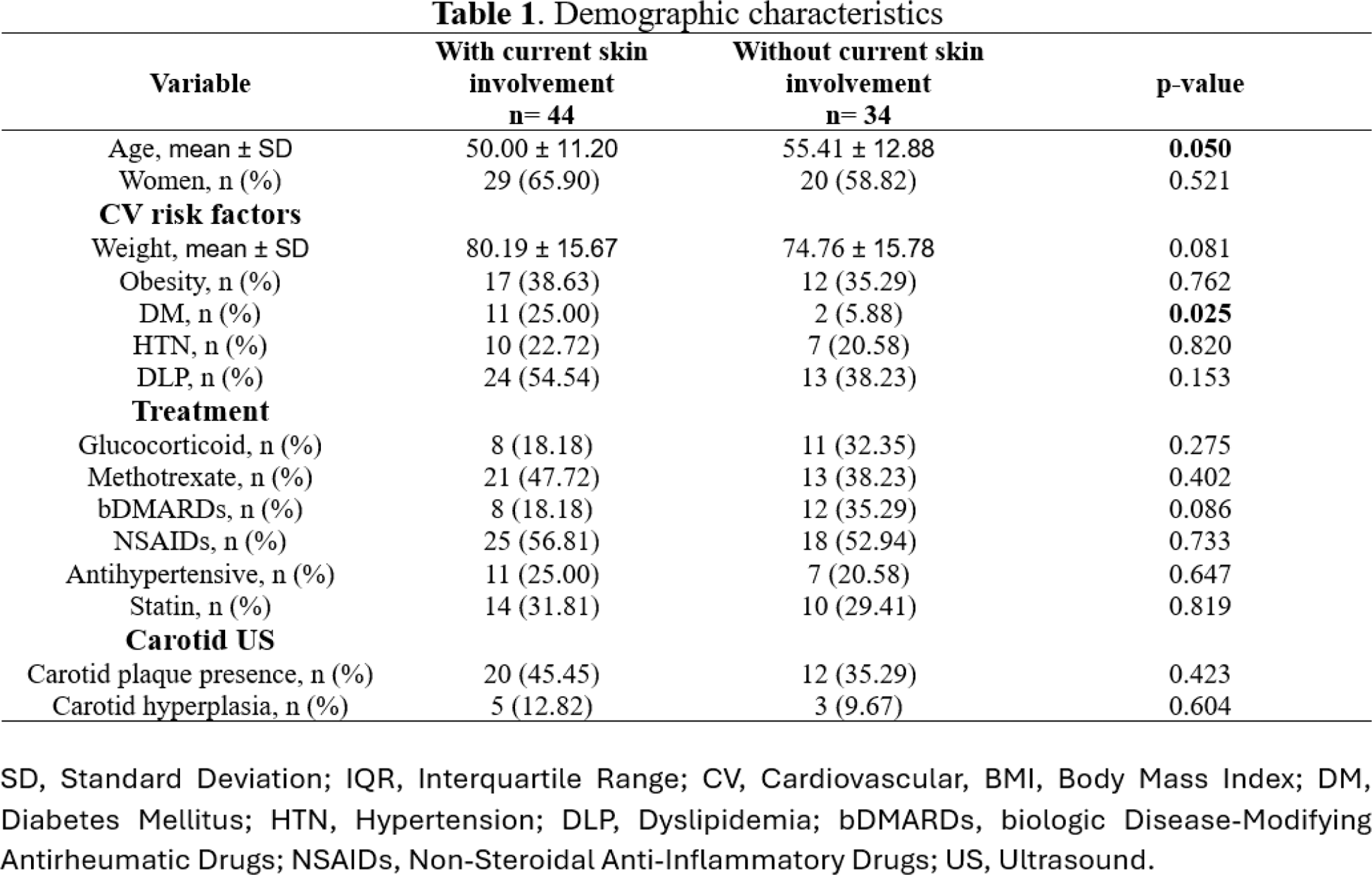
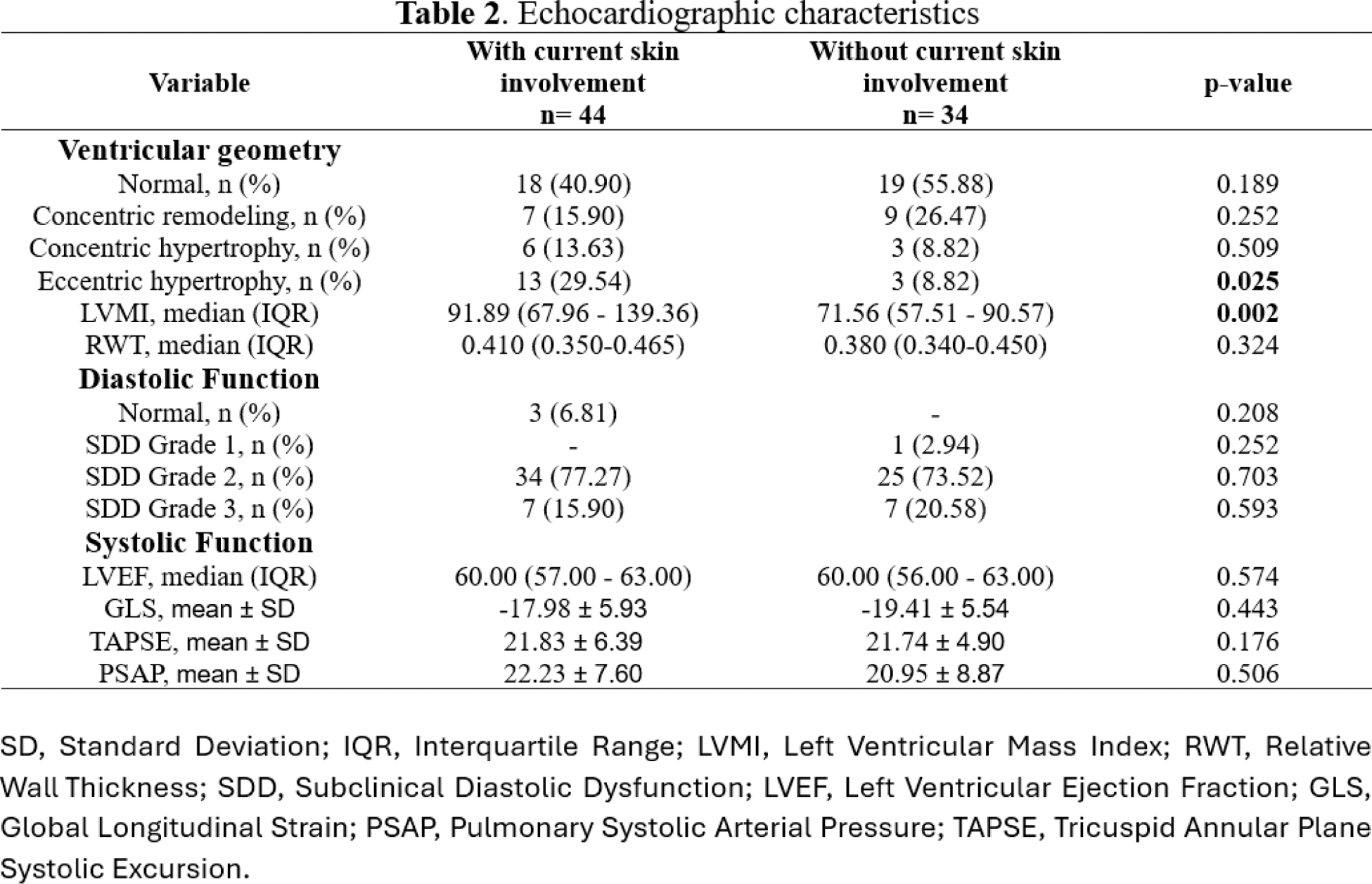
Results: 78 patients were included, divided into groups with and without current skin involvement. Patients with skin involvement tended to be younger than those without (50.00 vs. 55.41 years, p = 0.050). Both groups had a similar distribution of women (65.90% vs. 58.82%, p = 0.521). Cardiovascular (CV) risk factors were comparable between groups, except for diabetes mellitus (DM), which was more frequent in patients with skin involvement (25.00% vs. 5.88%, p = 0.025). There were no significant differences in obesity, hypertension (HTN), dyslipidemia (DLP), or treatments. Regarding carotid ultrasound findings, carotid plaque presence and carotid hyperplasia were observed in similar proportions between groups (45.45% vs. 35.29%, p = 0.423; 12.82% vs. 9.67%, p = 0.604, respectively). Eccentric hypertrophy was more frequent in patients with skin involvement (29.54% vs. 8.82%, p = 0.025), with a higher median left ventricular mass index (LVMI) (91.89 vs. 71.56 g/m², p = 0.002). No significant differences were found in relative wall thickness (RWT) or systolic and diastolic function parameters, including left ventricular ejection fraction (LVEF), global longitudinal strain (GLS), and pulmonary systolic arterial pressure (PSAP).
Conclusion: Patients with current skin involvement in PsA showed a higher prevalence of eccentric hypertrophy and a significantly higher left ventricular mass index compared to those without skin involvement. However, no differences were observed in other cardiovascular risk factors, carotid ultrasound findings, or systolic and diastolic function parameters. These findings suggest that skin involvement in PsA may be associated with subtle alterations in cardiac geometry, emphasizing the implementation of echocardiography as part of a complete cardiovascular evaluation in these patients.
REFERENCES: [1] Svedbom A, Ståhle M. The psoriasis area and severity index is an independent risk factor for cardiovascular events: A prospective register study. J Eur Acad Dermatol Venereol. 2023; 37:1841–7.
[2] Garshick M, Ward N, Krueger J, et al. Cardiovascular Risk in Patients With Psoriasis: JACC Review Topic of the Week. J Am Coll Cardiol. 2021;77(13):1670–80.
[3] Ramonda R, Nigro AL, Modesti V, Nalotto L, Musacchio E, Iaccarino L, et al. Atherosclerosis in psoriatic arthritis. Autoimmun Rev. 2011;10(12):773–8.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (