

Background: Psoriatic arthritis (PsA) is a chronic inflammatory joint disease frequently associated with psoriasis, leading to a significant reduction in patients’ quality of life (QoL). In addition to the direct impact of the disease, PsA patients often experience higher rates of comorbidities, including obesity, depression, and metabolic syndrome, which further exacerbate disease activity and impair QoL. Addressing challenges such as pain relief, functional capacity, social participation, fatigue, and psychological distress is critical for improving patient outcomes. The Psoriatic Arthritis Impact of Disease 12-item (PsAID-12) questionnaire, developed by the European Alliance of Associations for Rheumatology (EULAR), serves as a validated tool to assess the multifaceted impact of PsA on QoL. This study explores the relationship between the disease burden, as measured by PsAID-12, and the prevalence of carotid plaque (CP). Understanding this association may provide valuable insights to enhance health outcomes and guide treatment strategies.
Objectives: Evaluate the association between disease activity impact on QoL, as measured by the PsAID12 questionnaire, and the prevalence of CP in patients with PsA.
Methods: Cross-sectional and comparative study that included PsA patients aged 30 to 75 who fulfilled the 2006 CASPAR Classification Criteria. Patients with previous CV disease, overlap syndrome, or pregnancy were excluded. Carotid ultrasound was performed on all study participants. The presence of CP was defined as diffuse carotid intima-media thickness (cIMT) ≥1.2 mm or focal thickness ≥0.5 mm. Subclinical atherosclerosis was defined as the presence of CP or an increased cIMT (≥0.8mm). Quality of life was evaluated using the psAID12 questionnaire. Patients were categorized into two groups based on their PsAID12 score, with a score of ≥ 4 indicating high disease impact. The Kolmogorov–Smirnov test was employed to determine normality. Comparisons with Chi-square and T- or Mann Whitney’s U-test, accordingly. A p-value of ≤0.05 was considered statistically significant.
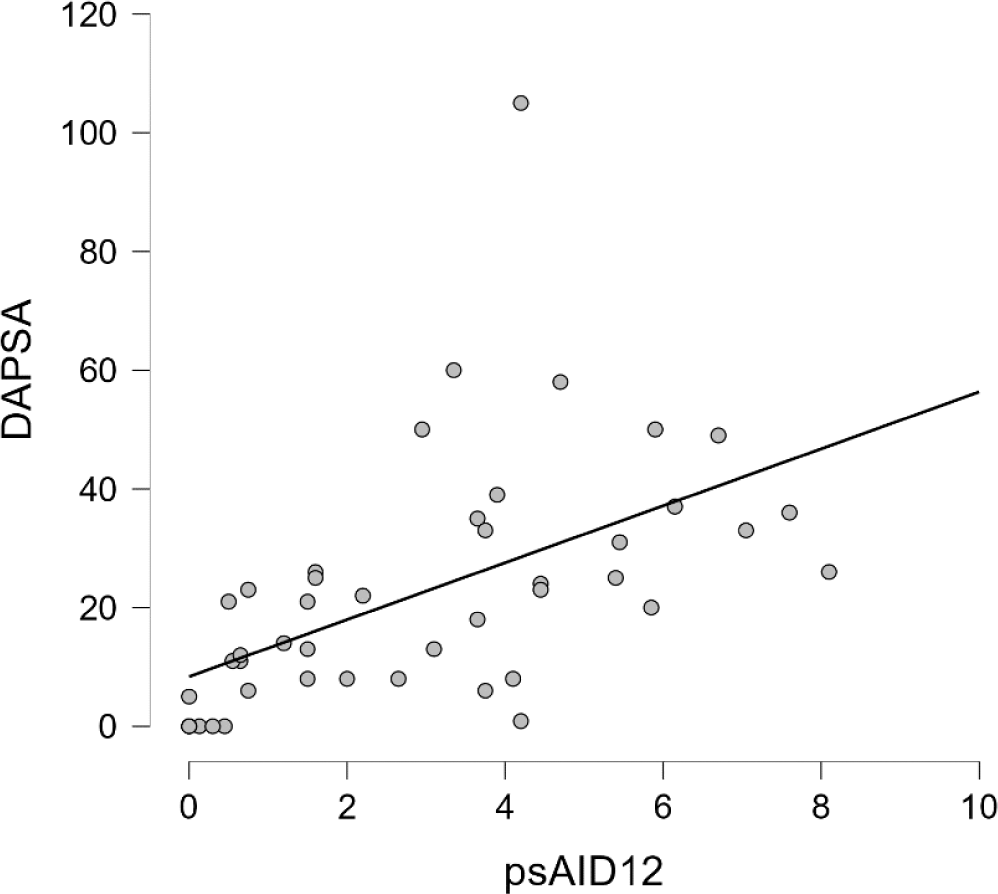
Results: A total of 45 PsA patients were included, with a mean age of 51.9 ± 12.6 years and a mean disease duration of 12.5 years. The average PsAID12 score for all patients was 2.95 ± 2.31. Dyslipidemia was the most prevalent CV risk factor, affecting 46.6% of patients (n = 21). No significant differences were observed in other CV risk factors between groups. Patients with PsAID12 ≥ 4 showed significantly higher DAPSA scores compared to those with PsAID12 <4 (35 vs. 16.2, p = 0.003), as well as a notably greater prevalence of CP (73.3% vs. 23.3%, p= < 0.002). Correlation analysis demonstrated a significant positive relationship between DAPSA and PsAID12 scores (Pearson’s r = 0.54, p < 0.001), indicating that higher disease activity is strongly associated with a greater impact on QoL, as measured by the PsAID12 questionnaire.
Conclusion: Our study demonstrates a significant association between disease activity and its impact on QoL in patients with PsA, as assessed by the PsAID12 questionnaire. Higher disease activity linked to elevated PsAID12 scores, reflecting a greater impact on QoL, is associated with an increased prevalence of CP in PsA patients. Therefore, incorporating routine CV assessments, such as carotid ultrasound, into the management of PsA patients—especially those with significant disease impact—is crucial for effectively addressing CV risk. These findings highlight the importance of controlling disease activity to improve patient-reported outcomes in PsA.
REFERENCES: [1] So H, Tam L-S. Cardiovascular disease and depression in psoriatic arthritis: Multidimensional comorbidities requiring multidisciplinary management. Best Pract Res Clin Rheumatol [Internet]. 2021;35(2):101689. Available from:
[2] Palominos PE, Coates L, Kohem CL, Orbai A-M, Smolen J, de Wit M, et al. Determinants of sleep impairment in psoriatic arthritis: An observational study with 396 patients from 14 countries. Joint Bone Spine [Internet]. 2020;87(5):449–54. Available from:
Comparison of demographic and disease characteristics.
| Variables | PsA patients with psAID12 <4
| PsA patients with psAID12 ≥4
| p-value |
|---|---|---|---|
| Age, years, ± SD | 50.1 ± 13.8 | 55.6 ± 9.2 | 0.17 |
| Women, n (%) | 20 (66.6) | 10 (66.6) | 1.00 |
| Diabetes, n (%) | 5 (16.6) | 3 (20) | 0.78 |
| Hypertension, n (%) | 6 (20) | 4 (26.6) | 0.61 |
| Dyslipidemia, n (%) | 11 (36.6) | 10 (66.6) | 0.05 |
| BMI, mean ± SD | 29.1 ± 5.0 | 30.2 ± 3.5 | 0.45 |
| Active smoking, n (%) | 9 (30) | 2 (13.3) | 0.44 |
| Time of evolution, years, mean ± SD | 10.6 ± 13.0 | 16.33 ± 13.1 | 0.17 |
| DAPSA, mean ± SD | 16.2 ± 15.2 | 35.0 ± 24.5 | 0.003 |
| PASI, median (IQR) | 0.0 (0.0-1.2) | 0.80 (0.28-1.9) | 0.08 |
| NAPSI, median (IQR) | 0.00 (0.0-2.7) | 1.0 (0.0-4.0) | 0.35 |
| Carotid plaque, n (%) | 7 (23.3) | 11 (73.3) | 0.002 |
PsA, psoriatic arthritis; psAID12, Psoriatic Arthritis Impact of Disease 12-item questionnaire; SD, standard deviation; IQR, interquartile range; BMI, body mass index; DAPSA, Disease Activity Psoriatic Arthritis; PASI, Psoriasis Area Severity Index; NAPSI, Nail Psoriasis Severity Index.
Positive correlation between DAPSA and psAID12 scores.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (