

Background: Rheumatoid arthritis (RA) is a chronic autoimmune disease with frequent extra-articular manifestations, including interstitial lung disease (ILD). ILD affects up to 60% of RA patients, with 10% developing clinically significant symptoms. Joint damage, dyspnoea, and fatigue often limit physical activity, exacerbating functional impairments. Sedentary behaviour (SB), defined as low-energy activity (<1.5 MET) while awake and sitting/reclining, is associated with cardiovascular risk, metabolic dysfunction, and reduced functional capacity. Even with sufficient physical activity, prolonged SB remains detrimental. Patients with RA-ILD face challenges achieving activity guidelines due to dyspnoea, joint pain, and fatigue. Understanding the extent and consequences of SB in RA-ILD patients versus those without lung involvement is essential to guide tailored interventions.
To measure the extent of SB in RA-ILD patients compared with RA patients without ILD (RA-Control).
To delineate the effect of SB on physical and psychological health in RA-ILD patients.
Methods: In this cross-sectional study, RA-ILD patients, fulfilling EULAR/ ACR criteria, were recruited from a joint Rheumatology/Respiratory clinic. Demographic data and BMI (kg/m²) were recorded. Sedentary behaviour (SB) was objectively measured using ActivPal monitors worn for 7 days. Functional capacity, pain, sleep, and psychological wellbeing were assessed using validated questionnaires, while RA disease activity was evaluated using Clinical Disease Activity Index (CDAI); pulmonary function was assessed by standard Pulmonary Function testing. Data from the RA-ILD cohort were compared to a cohort of RA patients without ILD with statistical comparisons and correlation analyses performed to identify differences and associations between groups.
Results: 16 RA-ILD patients were recruited for the study, with 72 patients in the RA control group. The RA-ILD cohort demonstrated moderately impaired quality of life, as reflected by a mean K-BILD score of 62.5 ± 13, alongside moderate impairments in pulmonary function with FVC (77.7 ± 14.1%) and DLCO (70 ± 9.1%). The RA-ILD patients were older (mean age 69.3 ± 5.1 years), had a higher percentage of male patients and had a higher BMI (30.2 ± 4.3 kg/m²) compared to the RA-Control group (mean age 60.8 ± 12.7 years, BMI 28.9 ± 4.5 kg/m²). While daily sedentary time was comparable between groups (~530 minutes/day), the RA-ILD cohort exhibited distinct sedentary behaviour patterns, including more prolonged sedentary bouts (>30 minutes: 7.6 ± 1.9 vs. 6.7 ± 1.7; >60 minutes: 4 ± 1.1 vs. 3.4 ± 1.3), fewer interruptions in sedentary time (49.9 ± 17 vs. 52.3 ± 17.9 interruptions/day), and reduced total standing time (200.9 ± 77.9 vs. 271.8 ± 86.1 minutes/day). In addition, psychological assessments highlighted significant differences between groups. RA-ILD patients reported higher depression scores (HADS: 7 ± 2.9 vs. 5.4 ± 3.7), reflecting the substantial burden of comorbid ILD on overall health and well-being (Table 1a and 1b). Correlation analyses (Table 2) revealed significant associations between SB metrics and clinical outcomes. In RA-ILD patients, daily sedentary time was strongly correlated with pain intensity (r = 0.64, p < 0.01) and widespread pain score (r = 0.59, p < 0.05), while RA Controls showed modest correlations with pain (r = 0.29, p<0.05) and anxiety (r = 0.3, p < 0.05). Among RA-ILD patients, a higher percentage of sedentary time was positively correlated with pain (r = 0.61, p < 0.05) and widespread pain (r = 0.57, p < 0.05). Prolonged sedentary bouts had limited significant correlations, but trends suggested negative associations with clinical outcomes in RA-ILD. Interruptions in sedentary time were negatively associated with pain (r = -0.37) and fatigue (r = -0.42) in RA-ILD patients. Total standing time was negatively correlated with pain (RA Control: r = -0.43, p < 0.01) and CDAI (RA Control: r = -0.34, p < 0.01; RA-ILD: r = -0.33). Additionally, daily steps were significantly negatively correlated with CDAI in RA-ILD (r = -0.53, p < 0.05).
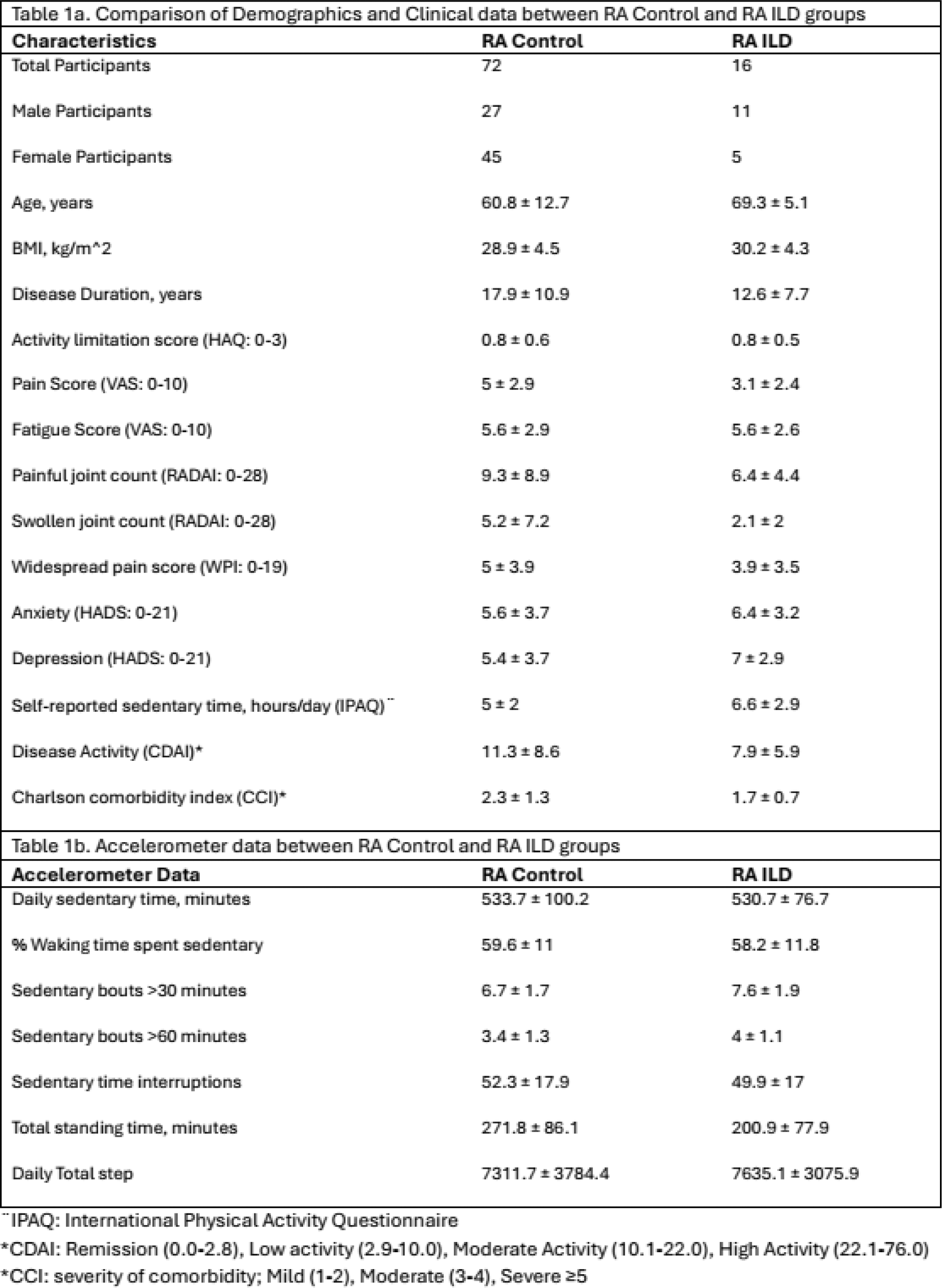
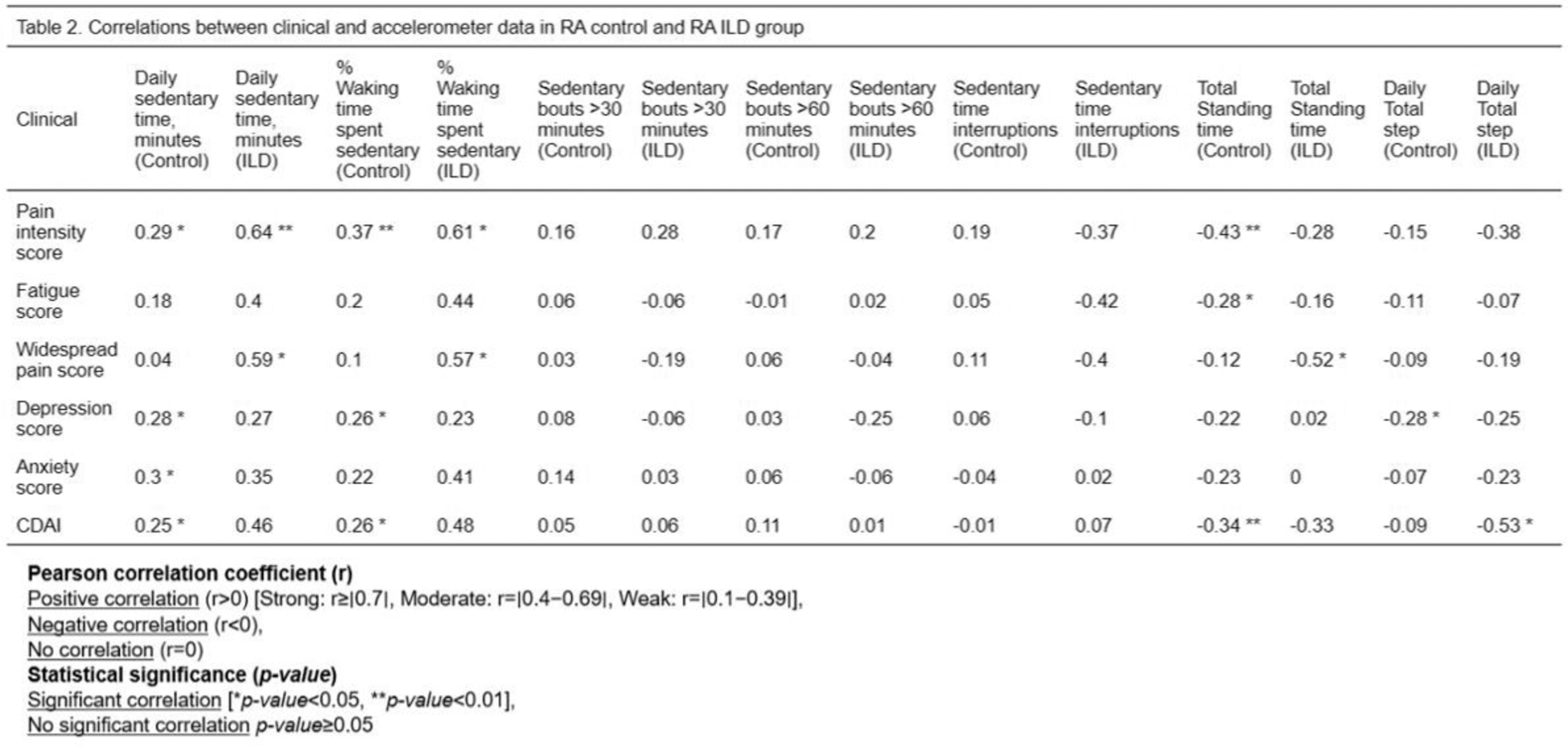
Conclusion: The RA-ILD cohort exhibited distinct SB patterns characterized by prolonged sedentary bouts, reduced standing time, and poorer physical and psychological health outcomes compared to RA Controls. These findings underscore the need for targeted interventions to minimize SB and promote light-intensity activities, potentially improving quality of life in this vulnerable group. The small RA-ILD cohort size (n=16) limits the generalizability of findings and calls for further research with larger sample sizes to validate these results.
REFERENCES: NIL.
Acknowledgements: Rheumatology Department, Cork University Hospital, Ireland. Respiratory Department, Cork University Hospital, Ireland. Physiotherapy Department, Cork University Hospital, Ireland. Rheumatology Patients.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (