

Background: Antiphospholipid syndrome (APS) is a systemic autoimmune disease characterised by increased risk of thrombosis and pregnancy morbidity with persistently elevated antiphospholipid antibodies (aPL). Childhood APS is usually diagnosed before age 18. Historically, APS has been classified using the Sapporo criteria, revised in 2006. The American College of Rheumatology (ACR) and European Alliance of Rheumatology Associations (EULAR) developed new classification criteria for APS in 2023 for research.
Objectives: Here we characterised a single-centre cohort of adolescents and young adults (AYA) with childhood-onset APS, diagnosed by expert opinion. We compared the performance of the new 2023 ACR/EULAR criteria, which have not yet been tested in childhood APS vs. the revised Sapporo criteria.
Methods: We screened our childhood-onset connective tissue disease database comprising 215 cases to identify AYA diagnosed with childhood-onset APS based on expert opinion. We collected retrospective data to assess their demographics, disease duration, clinical manifestations, serological markers, treatment, and compared the two classification criteria.
Results: We identified 12 AYA diagnosed with childhood-onset APS (see Table 1 below), 91% of which had another associated autoimmune disease, including childhood-onset systemic lupus erythematosus (cSLE)/Sjogren and juvenile dermatomyositis (JDM). For APS manifestations, 8/12 cases were treated with aspirin and warfarin and 2/12 with direct oral anticoagulants (DOACs). One young person had previously received plasma exchange for catastrophic APS. 5/215 cases of AYA had persistently elevated aPL (four with cSLE and one with JDM) without clinical APS manifestations (fulfilling neither the Sapporo nor the 2023 ACR/EULAR criteria for APS).
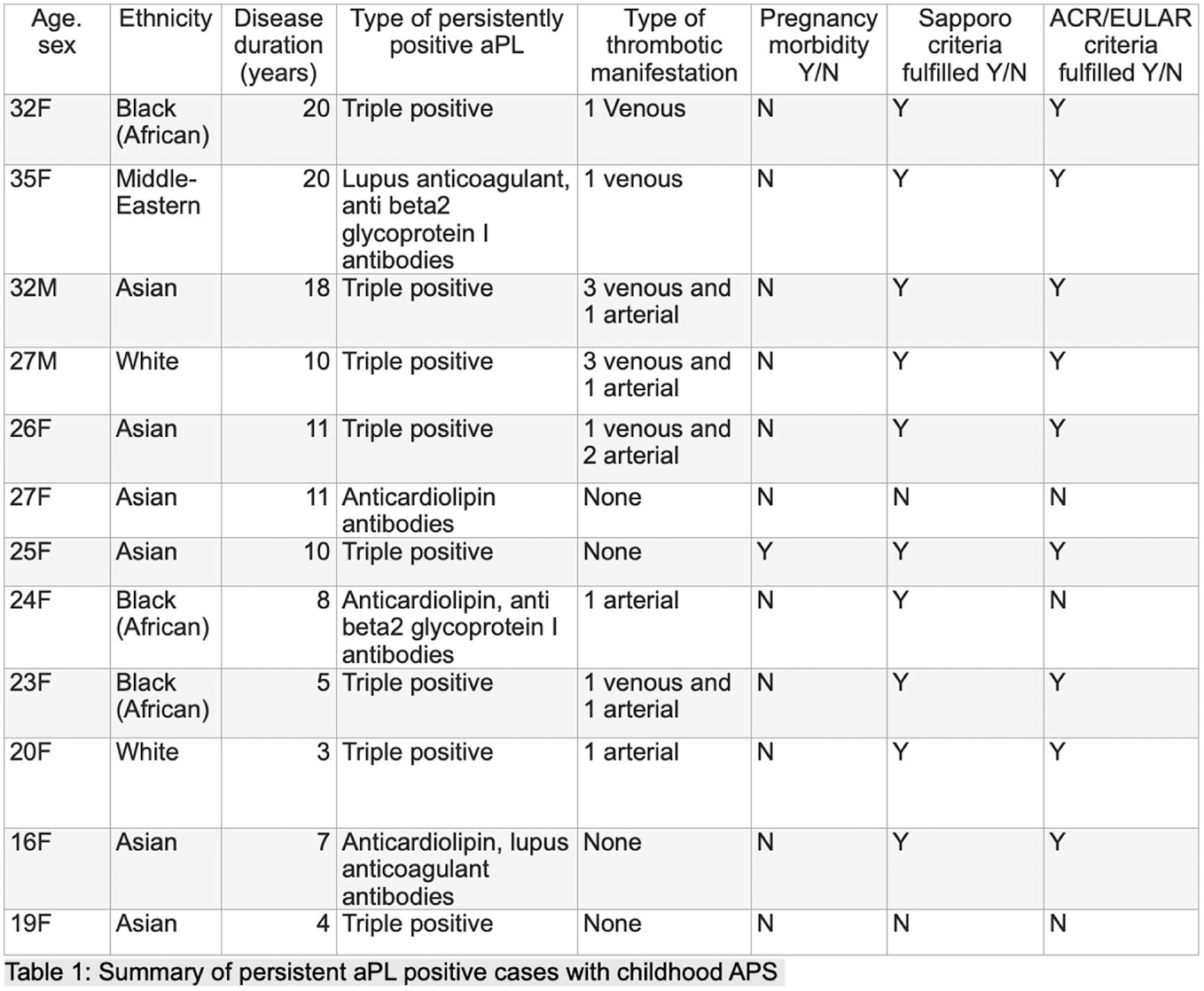
Conclusion: The 2023 ACR/EULAR classified 75%, while the revised Sapporo criteria classified 66% of AYA with APS diagnosed by expert opinion, suggesting that childhood-specific criteria may be warranted. In this small cohort, macrovascular thrombosis affected 66% of AYA diagnosed with APS, and 33% had more than one major thrombotic event. Overall, 47% (8/17) of AYA with persistently elevated aPL had thrombosis, despite previous publications suggesting low thrombosis risk in childhood APS. This cohort was followed up for 3-20 years, allowing us to assess the disease clinical course better over time. Future large cohort studies are needed to define the natural course and long-term complications of childhood APS.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (