

Background: Hyperuricemia is the main risk factor of gout, which has classically been linked to an increased risk of multiple comorbidities, such as chronic kidney disease or development of cardiovascular events (CVE), among others. However, the influence of asymptomatic hyperuricemia on the development of CVE is not yet fully understood, and the last clinical guidelines does not recommend its treatment to prevent them.
Objectives: To assess the association between hyperuricemia, serum uric acid levels (UA) and the development of atheroma plaque formation, CVE and death in patients with rheumatic diseases from the health department of Hospital Universitari Doctor Peset in Valencia, Spain.
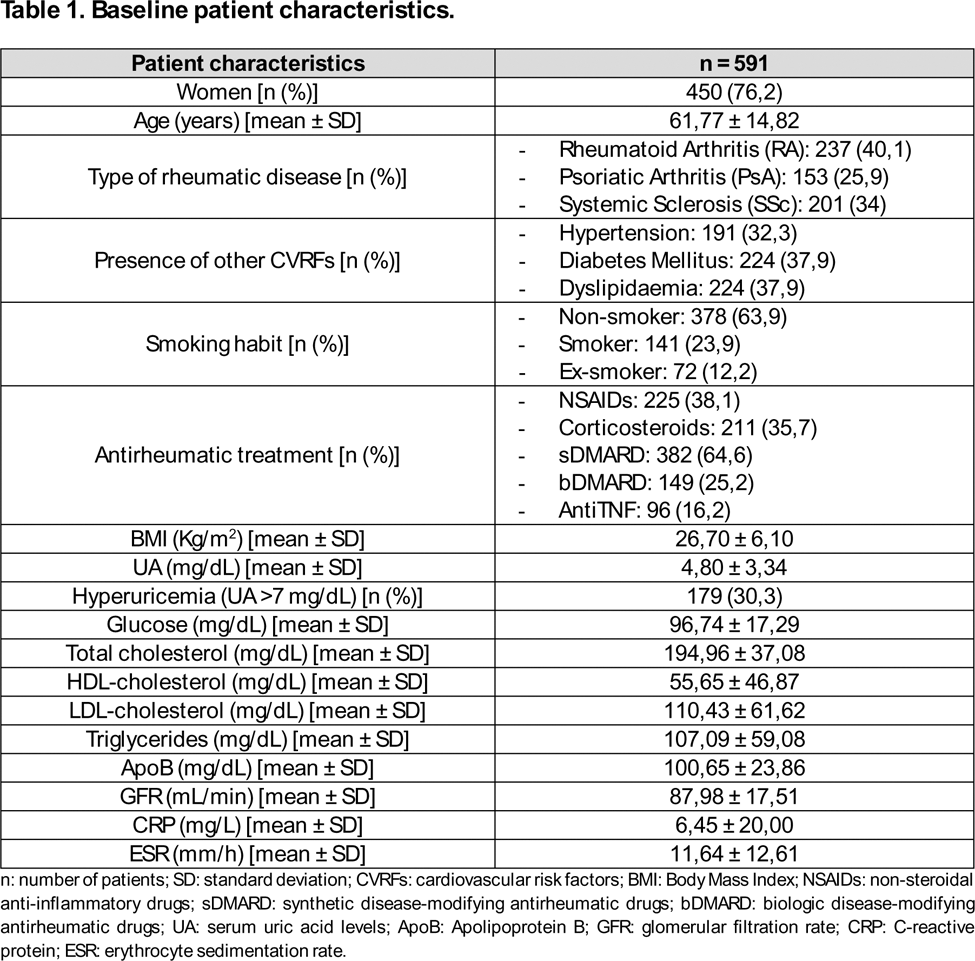
Methods: This retrospective study analysed patients diagnosed with Rheumatoid Arthritis (RA), Psoriatic Arthritis (PsA) and Systemic Sclerosis (SSc) who were followed up in our Rheumatology department until December 2024. Demographic, clinical and baseline laboratory data (glucose, total cholesterol, HDL-cholesterol, LDL-cholesterol, UA, triglycerides, apolipoprotein B [ApoB], acute phase reactants, renal filtration rate) were collected. Hyperuricemia was defined as UA > 7 mg/dL. Presence of other cardiovascular risk factors (CVRFs) as hypertension, diabetes mellitus, dyslipidaemia, smoking habit or BMI; presence of atheroma plaque (measured by carotid ultrasonography), CVE (myocardial infarction [MI], stroke, peripheral arterial disease) and deaths since diagnosis were also recorded. Statistical analysis was performed using SPSS v27.0.1.0 statistical software.
Results: 591 patients were included. Baseline patient characteristics are shown in Table 1. We found an association between hyperuricemia, atheroma plaque (p=0.001) and CVE (p=0.001). This association was also confirmed in UA (p=0.001 and p=0.01, respectively). Only UA was significatively related with MI (p=0.019). We did not observed association between hyperuricemia, UA and deaths (p=0.276). When analysed by subgroups, men had a significative association between hyperuricemia (p=0.007), UA (p=0.002) and CVE. Women had a significative association between hyperuricemia, UA, atheroma plaque (p=0.001) and CVE (p=0.001 and p=0.003). RA patients showed significant association between hyperuricemia and atheroma plaque (p=0.029); PsA patients showed significative moderate association between hyperuricemia and CVE (p=0.005); and SSc patients had a significative association between UA and atheroma plaque (p=0.001), and between hyperuricemia and CVE (p=0.003). However, when multivariate logistic regression model was performed, only the association between UA and CVE in the total population, and between hyperuricemia and CVE in PsA patients were found significant.
Conclusion: In our study, hyperuricemia and UA are associated to the development of CVE in RA, PsA and SSc patients, but with moderate to low effect. Hyperuricemia was only found significatively associated with CVE in PsA patients.
REFERENCES: [1] Asghari KM, Zahmatyar M, Seyedi F, Motamedi A, Zolfi M, Alamdary SJ, et al. Gout: global epidemiology, risk factors, comorbidities and complications: a narrative review. BMC Musculoskelet Disord. 2024 Dec 19;25(1):1047.
[2] Maloberti A, Colombo V, Daus F, De Censi L, Abrignani MG, Temporelli PL, et al. Two still unanswered questions about uric acid and cardiovascular prevention: Is a specific uric acid cut-off needed? Is hypouricemic treatment able to reduce cardiovascular risk? Nutrition, Metabolism and Cardiovascular Diseases. 2024 Nov;103792.
[3] Richette P, Doherty M, Pascual E, Barskova V, Becce F, Castañeda-Sanabria J, et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Annals of the Rheumatic Diseases. 2017 Jan;76(1):29–42.
[4] Timsans J, Kerola AM, Rantalaiho VM, Hakkarainen KN, Kautiainen HJ, Kauppi MJ. “Metabolic” Type of Hyperuricemia Increases Mortality Mainly by Leading to Premature Death From Cardiovascular Disease. Mayo Clinic Proceedings. 2024 Nov;99(11):1835–7.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (