

Background: Comorbid anxiety (ANX), depression (DEP), and fibromyalgia (FM) are reported in patients with many rheumatic diagnoses and may elevate indices such as DAS28 and CDAI designed to assess inflammatory activity in rheumatoid arthritis (RA). Nonetheless, formal recognition of ANX, DEP, and/or FM is largely limited to research studies, as feasible screening in routine care is limited by a need for multiple patient questionnaires. A multidimensional health assessment questionnaire (MDHAQ), completed by most patients in 5-10 minutes and scored by a professional in less than 30 seconds in paper formats and instantly in electronic versions, contains 4 validated indices based on individual scores within the MDHAQ: RAPID3 - routine assessment of patient index data, to assess overall patient status, MAS 2 - MDHAQ anxiety screen, MDS2 - MDHAQ depression screen, and FAST4 - fibromyalgia assessment screening tool. MDHAQ is informative in all rheumatic diseases and available for any clinical setting prior to seeing a health professional.
Objectives: To study the prevalence of positive MDHAQ screening for comorbid ANX, DEP, and/or FM on MDHAQ indices in unselected routine care patients with any rheumatic diagnosis seen at an academic medical center.
Methods: All patients with all diagnoses are asked to complete an MDHAQ at each rheumatology visit prior to seeing a health professional, scanned into the electronic medical record (EMR), and entered into a longitudinal database. The prevalence of positive screening on the MDHAQ indices for ANX, DEP, and FM was computed according to ICD-10 diagnoses in the EMR. Diagnoses with fewer than 20 patients were grouped as “other inflammatory” (other inflam) or “other noninflammatory” (other non-inflam).
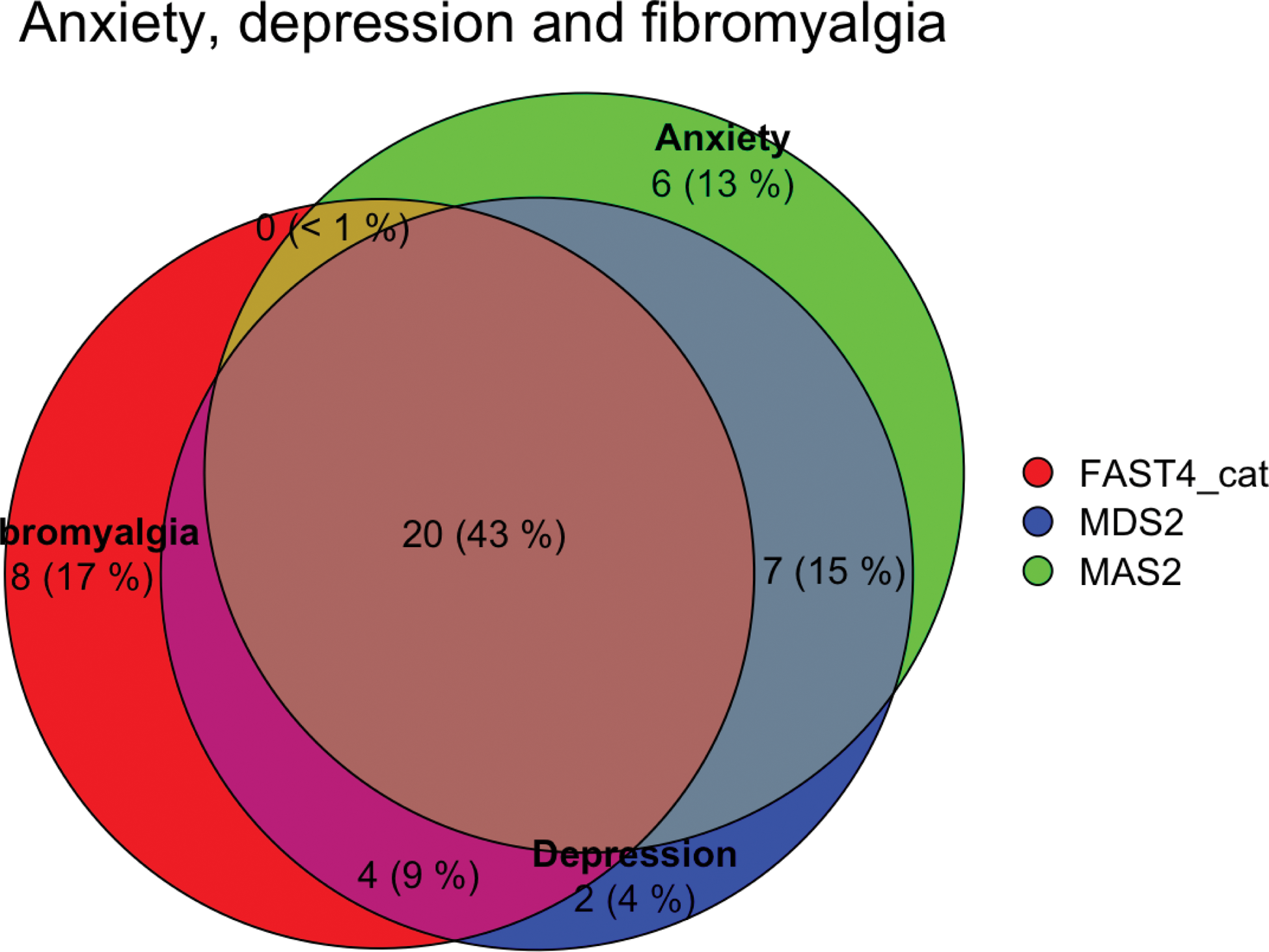
Results: In 1337 patients, excluding 60 with primary FM, positive screening for any of the 3 MDHAQ screening indices was seen in 587 (44%), including 399 (30%) for MAS2 anxiety, 321 (24%) for MDS2 depression, 328 (25%) for FAST4 FM; 750 (56%) screened negative for all the 3 indices (Figure 1 and Table 1, listing diagnoses with 20 or more patients according to inflammatory, noninflammatory, and FM diagnosis in increasing order of any positive screen). Among diagnoses categories, positive screening for any of the 3 indices ranged from 30% in crystal arthritis and vasculitis to 52% in patients with other noninflammatory diagnoses, for ANX from 17% in “other inflammatory” to 39% in “other non-inflammatory” diagnoses, for DEP from 9% in systemic sclerosis to 33% in myositis, and for FM from 7% in vasculitis to 31% in OA (Table 1). The totals were raised by only 1% with inclusion of 60 patients with primary FM, reflecting a high prevalence in all other diagnosis categories. Among all patients with a positive MDHAQ screening index for ANX, DEP, and/or FM, one of the 3 was positive in 271 (43%), 2 of the 3 in 214 (34%), and all 3 in 149 (24%) (Figure 1, excluding patients with primary FM). Prevalences were lower in patients with crystalline arthritis in inflammatory diagnoses and in BMD disorders in non-inflammatory diagnoses, consistent with clinical experience. An important limitation of these findings involves data from only one setting and would likely vary at other settings according to cultural and socioeconomic variables as well as the prevalence of different diagnoses.
Conclusion: In 1337 patients seen in routine care (excluding 60 with primary FM), positive screening on MDHAQ indices was seen in 30% for ANX, 25% for FM, 24% for DEP, and 44% for any of the 3 indices. Although this study (and perhaps any study) does not provide definitive data concerning the prevalence of ANX, DEP, and/or FM in different rheumatic diagnoses, positive screening is common, and affects assessment, management, and outcomes of all rheumatic diseases, including indices to assess inflammatory activity. An MDHAQ, completed by most patients in 5-10 minutes prior to seeing a rheumatologist, provides a feasible strategy to screen for ANX, DEP, and FM in all patients.
REFERENCES: NIL.
Proportion of patients in each category that are negative or positive for any of the 3 MDHAQ indices for anxiety, depression, and/or fibromyalgia and each individual index
| 1° Diagnosis | n | % ANX, DEP, & FM neg | % ANX, DEP,
| % Anxiety
| % Depression
| % FM
|
|---|---|---|---|---|---|---|
| Crystal arthritis | 50 | 70% | 30% | 20% | 20% | 12% |
| Vasculitis | 27 | 70% | 30% | 19% | 22% | 7% |
| Systemic sclerosis | 23 | 65% | 35% | 35% | 9% | 9% |
| Other Inflammatory | 54 | 63% | 37% | 17% | 15% | 26% |
| Spondyloarthropathy | 29 | 62% | 38% | 31% | 21% | 28% |
| Rheumatoid arthritis | 366 | 57% | 43% | 25% | 23% | 27% |
| Psoriatic arthritis | 40 | 55% | 45% | 33% | 30% | 25% |
| Stomach lupus erythematosus | 215 | 55% | 45% | 33% | 23% | 22% |
| Polymyalgia rheumatica | 22 | 55% | 45% | 18% | 27% | 27% |
| Sjogren syndrome | 45 | 53% | 47% | 33% | 27% | 24% |
| Myositis | 21 | 52% | 48% | 38% | 33% | 10% |
| Bone mineral disorders | 55 | 58% | 42% | 36% | 24% | 18% |
| Osteoarthritis | 238 | 54% | 46% | 32% | 25% | 31% |
| Other non-inflammatory | 152 | 48% | 52% | 39% | 31% | 24% |
| Total without primary FM | 1337 | 56% | 44% | 30% | 24% | 25% |
| Primary FM | 60 | 22% | 78% | 55% | 55% | 53% |
| Totals – all pts | 1397 | 55% | 45% | 31% | 25% | 26% |
Positive screening for anxiety, depression and fibromyalgia in patients seen in routine rheumatology care, excluding patients with primary fibromyalgia.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (