

Background: Antiphospholipid syndrome (APS) is a thrombo-inflammatory disease characterized by recurrent thrombotic events and obstetrical complications in the presence of pathogenic antiphospholipid antibodies. APS is classified as primary APS (PAPS) when there is no evidence of an underlying condition and secondary APS (SAPS) when another autoimmune disease, mainly systemic lupus erythematosus (SLE), is present.
Objectives: To describe the clinical and laboratory characteristics of patients with PAPS and SAPS, and to identify the differences between patients with only arterial thromboses and those with only venous thromboses.
Methods: A retrospective study was conducted on a Greek cohort of APS patients. Patient demographics, as well as clinical and serological features, were recorded. Comparisons were made between primary and secondary APS patients and among arterial and venous thromboses using parametric and non-parametric tests. Statistical significance was set at p < 0.05.
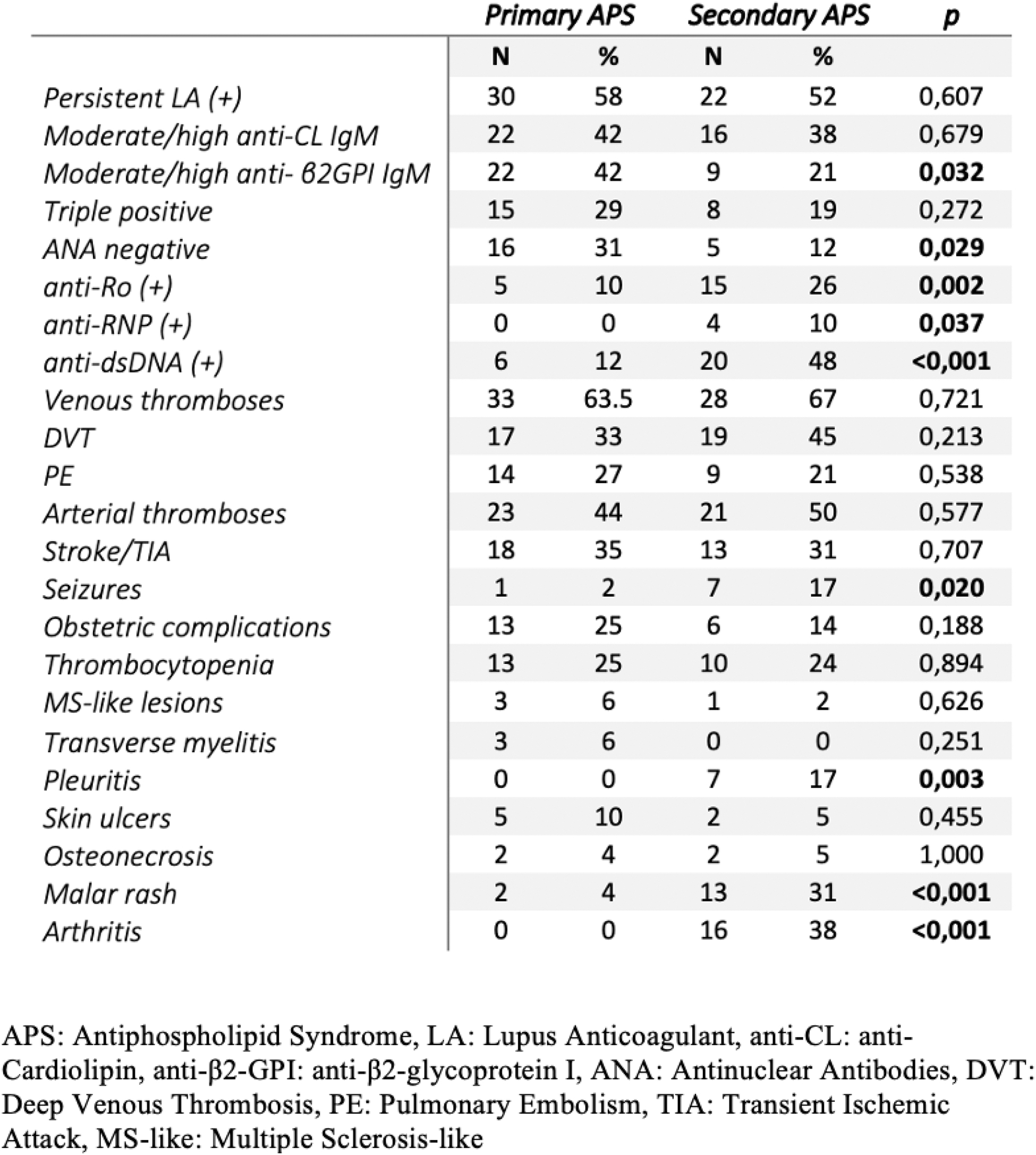
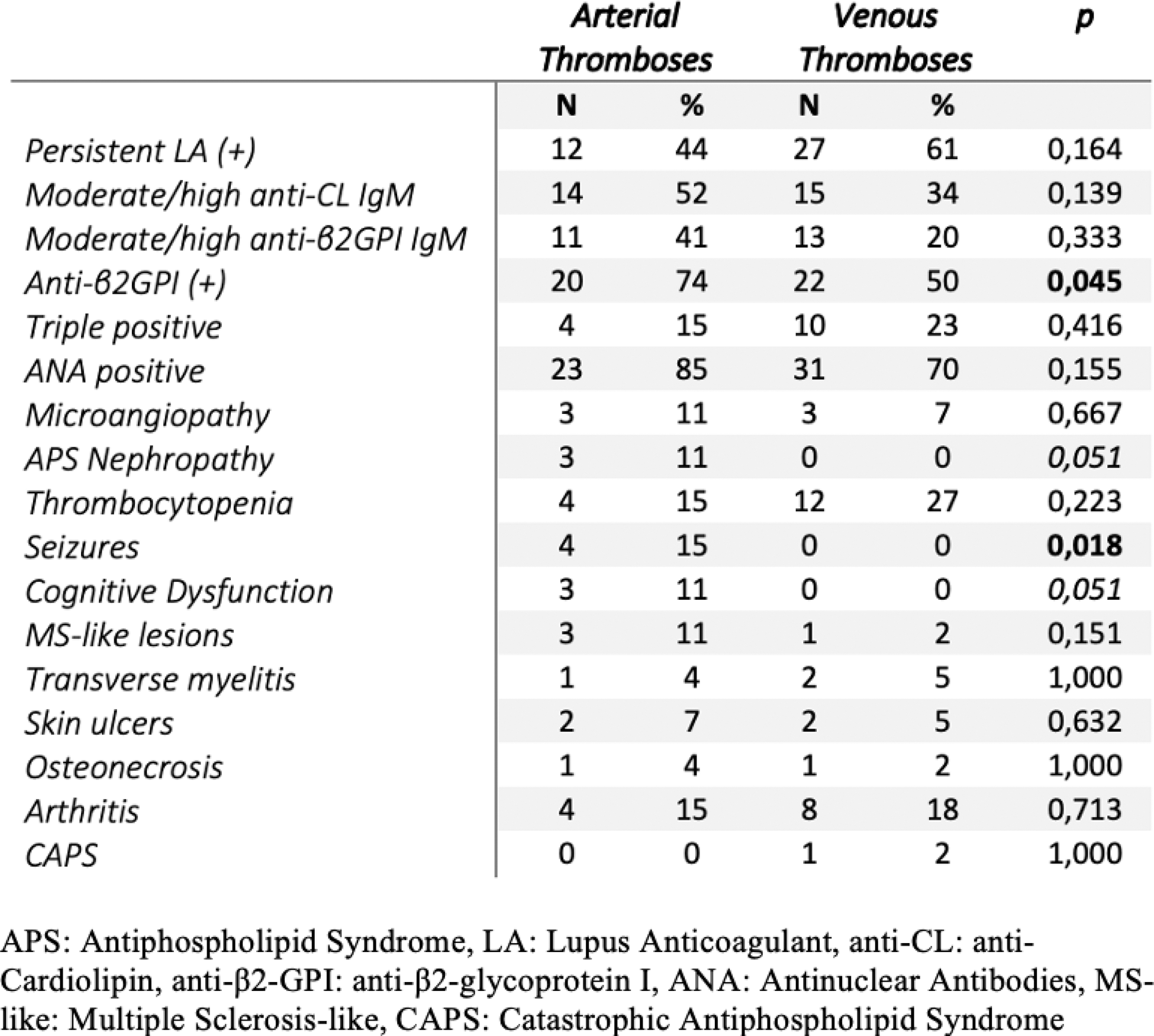
Results: Among 129 patients meeting the revised Sapporo criteria, 70 patients with PAPS and 59 with SAPS were included. After applying the 2023 ACR/EULAR classification criteria, 94 patients (72.9%) were classified as having APS. Of those, 52 were classified as having PAPS and 42 as having SAPS. The mean age at diagnosis was 41 ± 11 years; 69% (n=65) were female, and 29% (n=27) were active smokers. The most commonly detected antibodies included IgG and IgM anti-cardiolipin (anti-CL) at 61.7% and 40%, lupus anticoagulant at 55%, and IgG and IgM anti-β2-glycoprotein I (anti-β2GPI) at 42.5% and 33%. Additionally, triple positivity was detected in 25% (n=23). Regarding clinical manifestations, 61 patients (64.9%) suffered from venous thromboses (deep vein thrombosis: 38%, pulmonary embolism: 25%), 44 patients (47%) experienced arterial thrombosis (most commonly stroke: 33%), and 19 patients (20.2%) faced pregnancy complications relevant to APS. Other manifestations included thrombocytopenia (n=23, 25%), microvascular manifestations (n=11, 12%), APS nephropathy (n=6, 6%), osteonecrosis (n=4, 4%), transverse myelitis (n=3, 3%). and catastrophic APS (n=2, 2%). PAPS patients were more frequently positive for IgM anti-β2GPI (42% vs. 21%, p=0.032), less frequently positive for anti-Ro (10% vs. 36%, p=0.002), anti-RNP (0% vs. 10%, p=0.037), and anti-dsDNA (12% vs. 48%, p=0.001). Compared to PAPS, the SAPS group had a higher prevalence of patients with malar rash (31% vs. 4%, p<0.001), arthritis (38% vs. 0%, p<0.001), pleuritis (17% vs. 0%, p<0.001), and seizures (17% vs. 2% p=0.02) (Figure 1). Excluding patients with both arterial and venous thromboses, we identified 27 patients with exclusively arterial thrombosis and 44 with solely venous thrombosis. Compared to patients with venous thrombosis, those with arterial thrombosis were diagnosed at an older age (median age: 48 vs. 38, p=0.018) and had higher rates of arterial hypertension (30% vs. 7%, p=0.01) and anti-β2GPI (74% vs. 50%, p=0.045). In terms of clinical manifestations, patients with arterial thrombosis more frequently experienced epileptic seizures (15% vs. 0%, p=0.018), APS nephropathy (11% vs. 0%, p=0.051), and cognitive dysfunction (11% vs. 0%, p=0.051) (Figure 2).
Conclusion: In our cohort, no differences were found in the APS cardinal clinical and serological characteristics between patients with PAPS and SAPS, except for IgM anti-β2GPI, which was more frequently detected in PAPS. The underlying autoimmune disease in SAPS determined the only differences in the clinical and antibody profiles. A comparison of patients with arterial and venous thromboses showed that those with arterial thrombosis tended to be older and were more often positive for anti-β2GPI.
Comparative analysis of patients with primary and secondary APS
Comparative analysis of APS patients with arterial and venous thromboses
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (