

Background: Despite increased risk of severe COVID-19 outcomes, updated COVID-19 vaccine uptake remains inadequate among people with autoimmune rheumatic diseases (AIRD). This issue is particularly acute in the southern United States (U.S.).
Objectives: We aimed to identify key themes associated with barriers to and acceptance of receiving the updated COVID-19 vaccine among people with AIRD who receive rheumatology care at a large academic medical practice in the U.S. Deep South.
Methods: This qualitative study involved focus groups of adults with AIRD taking immunosuppressive medications and who had received at least one COVID-19 vaccine. We developed a semi-structured interview guide that addressed key domains around vaccinations including experiences living with AIRD, perceptions about the risk of contracting COVID-19 infection, experience with the COVID-19 vaccine, and best practices for receiving vaccine-related information. We approached eligible patients during routine outpatient rheumatology clinic visits and obtained verbal informed consent. Focus group interviews were conducted both in-person and virtually, and were audio recorded and transcribed using a HIPAA-compliant transcription service. Transcripts were coded using NVivo 14 and analyzed using inductive/ deductive hybrid thematic analysis to identify overarching themes and subthemes. This process integrated: (1) deductive coding based on pre-existing literature on barriers and facilitators to vaccinations in the general population using a social ecological framework with (2) inductive coding that emerged directly from the data.
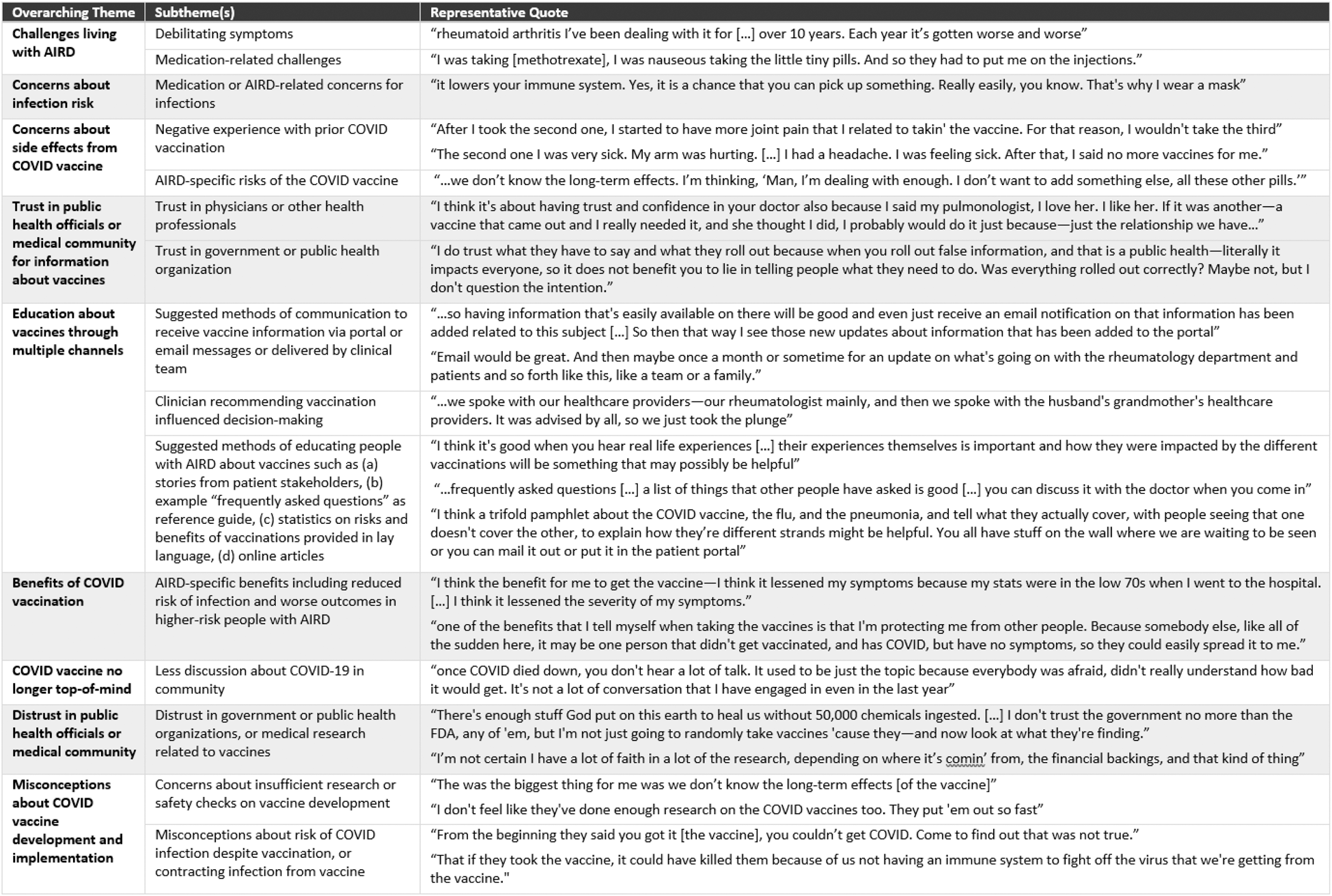
Results: From May through November 2024, N=32 individuals with AIRD participated in 8 focus groups each with 2-5 participants to reach thematic saturation. Participants had a mean (SD) age of 57 (15) years, 26 (81%) were female, and 14 (4%) were Black or African American race (Table 1). Thematic analysis revealed 9 overarching themes (Table 2). A key overarching theme involved challenges living with AIRD and using immunosuppressive medications for treatment, which reflected the negative impact of AIRD on individuals’ quality of life. Key barriers to vaccination emerged from several overarching themes, including (1) concerns about potential or experienced adverse effects from the COVID-19 vaccine including risk of underlying AIRD flare following vaccination; (2) perception that COVID-19 is no longer top-of-mind in the community; (3) distrust in vaccine-related recommendations from public health officials, the medical community, and the published COVID-19 vaccine research; and (4) misconceptions about COVID-19 vaccine development and implementation. Multiple facilitators to vaccination emerged including (1) concerns about infection risk including the role of AIRD and immunosuppressive medications implicated in infection risk; (2) trust in public health officials or medical community related to vaccine recommendations; and (3) perceived benefits of the COVID-19 vaccine. Lastly, a key theme emerged related to suggestions on patient-centered approaches to improve acceptance of vaccine-related information including methods for providing education about vaccines through multiple channels. Participants endorsed several methods of communication to receive vaccine information including via secure institutional portal or email messaging. They also endorsed methods for educating patients about vaccinations such as through stories by patient stakeholders, examples of “frequently asked questions” as a reference guide for use during discussions with clinicians, and improved access to online resources from trusted sources in clear transparent lay language.
Conclusion: We identified several modifiable barriers as well as facilitators associated with vaccine acceptance among people with AIRD, including improving patient understanding of the benefits of vaccination, leveraging patients‘ high degree of trust of medical providers to promote vaccine uptake, and best-practices for communicating vaccine-related information. Compared to previous data on factors influencing decisions by AIRD patients to receive the original COVID-19 vaccine [1-3], the key themes associated with acceptance to or hesitancy to receiving the updated COVID-19 vaccine persist. Future studies may incorporate these factors as part of an intervention aimed at improving vaccine uptake among people with AIRD.
REFERENCES: [1] Abad N, Messinger SD, et al. A qualitative study of behavioral and social drivers of COVID-19 vaccine confidence and uptake among unvaccinated Americans in the US April-May 2021. PLoS One. 2023;18(2):e0281497.
[2] Holladay EE, Mudano AS, et al. COVID-19 Vaccine Uptake, Hesitancy, and Flare in a Large Rheumatology Practice Network. Arthritis Care Res (Hoboken). 2024;76(1):111-9.
[3] Manrique de Lara A, Colmenares-Roa T, et al. Sociocultural and moral narratives influencing the decision to vaccinate among rheumatic disease patients: a qualitative study. Clin Rheumatol. 2023;42(8):2199-207.
Table 1. Demographic and clinical characteristics of participants who participated in focus groups.
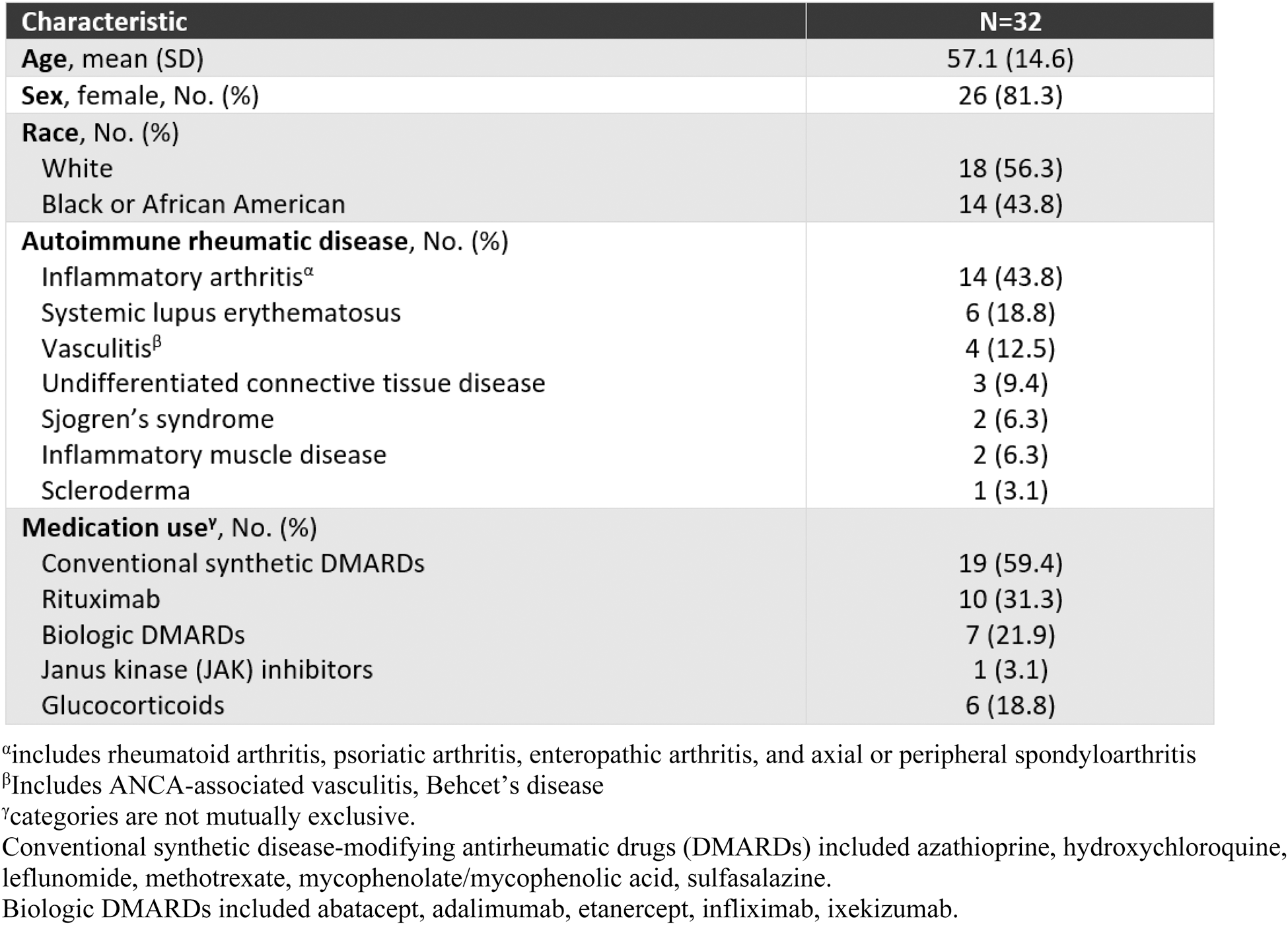
Table 2. Key overarching themes and subthemes emerging from qualitative data analysis of 8 focus groups.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (