

Background: T cell redirecting therapies (TCRT) leverage cytotoxicity from T cells to kill target cells. Chimeric antigen receptor (CAR) T cells express a CAR transgene, allowing T cells to recognize and kill cells expressing a specific antigen. In contrast, T cell engagers (TCE) are biologics which act as bridge between T cells and target cells, thereby redirecting their cytotoxicity. T cell redirecting therapies have demonstrated transformative therapeutic successes for B cell malignancies. More recently, CAR T and TCE therapy have been successfully applied to a variety of autoimmune diseases, including systemic lupus erythematosus, myasthenia gravis, multiple sclerosis, rheumatoid arthritis, idiopathic inflammatory myositis, systemic sclerosis and primary Sjögren’s syndrome [1, 2, 3]. While the clinical trial landscape is quickly evolving, TCRT are currently only applied in specialized centers and published patient numbers are still low. Hence, first-hand experience of most clinicians with TCRTs is limited.
Objectives: We aimed to assess the knowledge and perception of emerging T cell redirecting therapies amongst German rheumatologists, focusing on their therapeutic potential, barriers to application, and expectations for future implementation.
Methods: The prospective, web-based survey including questions on existing knowledge and possible applications in treated patients as well as potential barriers was distributed at the Congress of the German Society for Rheumatology, as well as via email, social media and QR Code from September 18th 2024 through January 5th 2025.
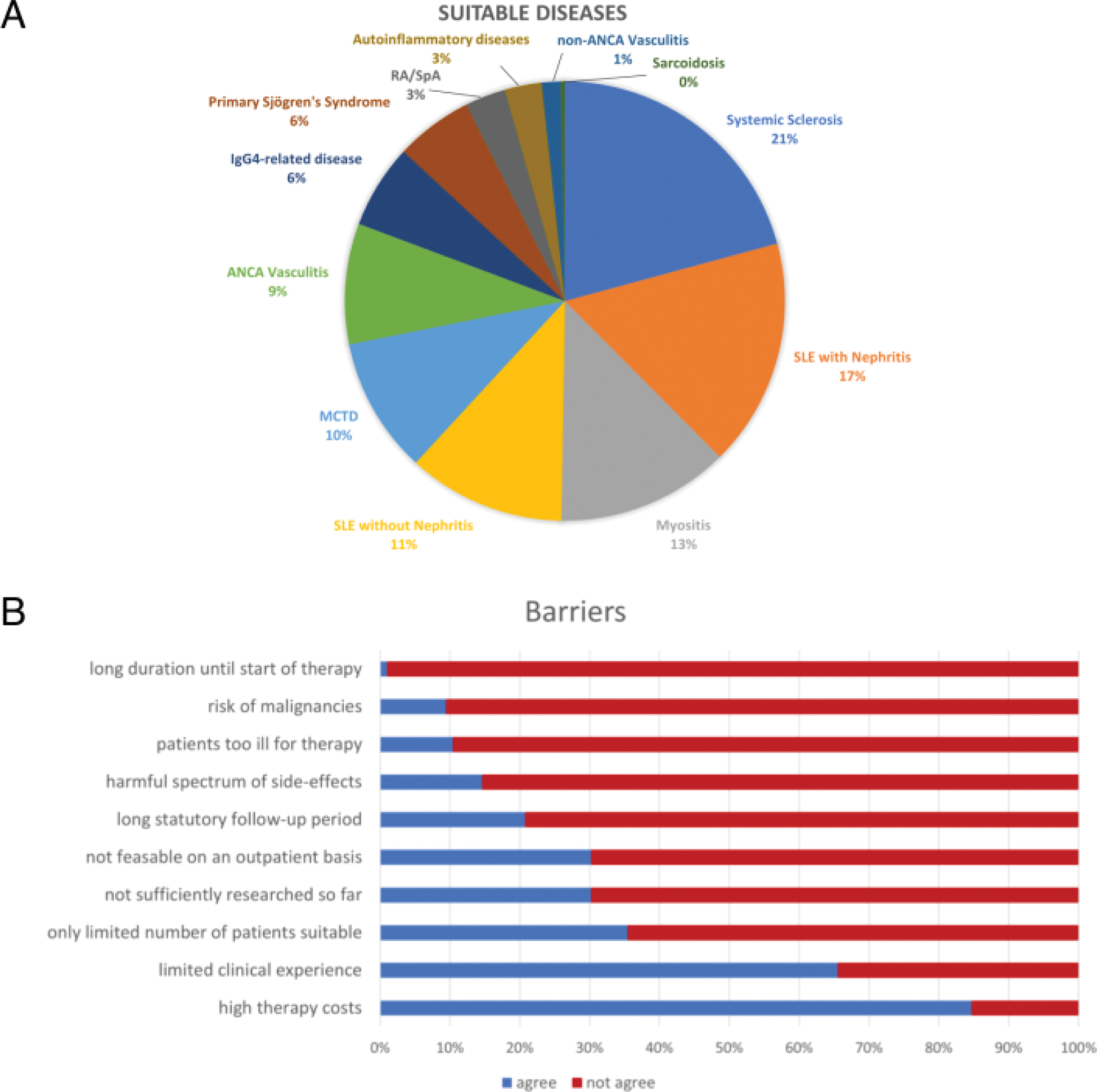
Results: In total, 98 rheumatologists completed the survey. Participants had a median age of 43.04 years; 53.1 % were female (Table 1). The majority of rheumatologists worked in a university hospital and overall, 67.7 % were specialized in rheumatology while 32.3 % were residents (Table 1). Almost all rheumatologists (94.8 %) were willing to refer patients to specialized centers for TCRT cell therapy. However, rheumatologists considered only 5 % of their patients suitable for TCRT. Possibly suitable diseases for TCRT approach stated by the participants were mainly connective tissue diseases (Figure 1a). When presented different case vignettes, participants suggested especially patients with severe organ involvement and extensive immunosuppressive treatment suitable for TCRT. Main barriers stated by German rheumatologists were high treatment costs (82%), limited clinical experience (65.5%) as well as limited applications in patients (35.4%) (Figure 1b). Most participants correctly stated cytokine release syndrome, neurotoxicity and infections as the most common side effects, and recognized chronic viral infections or heart failure as potential contraindications.
Conclusion: This study reflects that most German rheumatologists see a therapeutic option in TCRT, especially for patients with highly active systemic diseases and extensive previous immunosuppressive treatment. Participants demonstrated willingness to refer their own patients to specialized treatment centers. Participants were aware of potential side effects and contraindications of TCRTs. High treatment costs and limited clinical data were perceived as the main barriers for broader application of TCRTs in autoimmune diseases.
REFERENCES: [1] Müller F, Taubmann J, Bucci L, et al. CD19 CAR T-Cell Therapy in Autoimmune Disease - A Case Series with Follow-up. N Engl J Med. 2024;390(8):687-700. doi:10.1056/NEJMoa2308917.
[2] Hagen M, Bucci L, Böltz S, et al. BCMA-Targeted T-Cell-Engager Therapy for Autoimmune Disease. N Engl J Med. 2024;391(9):867-869. doi:10.1056/NEJMc2408786.
[3] Fischbach F, Richter J, Pfeffer LK, et al. CD19-targeted chimeric antigen receptor T cell therapy in two patients with multiple sclerosis. Med. 2024;5(6):550-558.e2. doi:10.1016/j.medj.2024.03.002.
Study population characteristics
| Women | 52/98 (53.1 %) | |
|---|---|---|
| Age in years | Mean ± SD | 43.04 ± 12.4 |
| Position | ||
| Resident | 30/93 (32.3 %) | |
| Board-certificated rheumatologist | 42/93 (45.2 %) | |
| Senior consultant | 14/93 (15.1 %) | |
| Chief physician | 7/93 (7.5 %) | |
| Type of Workplace | ||
| University Hospital | 44/95 (46.3 %) | |
| Tertiary care clinic | 4/95 (4.2 %) | |
| Specialist clinic | 6/95 (6.3 %) | |
| Primary care clinic | 6/95 (6.3 %) | |
| Own practice | 20/95 (21.1 %) | |
| Employed in practice or medical care center | 15/95 (15.8 %) |
A) Designated diseases potentially suitable for TCRT according to German rheumatologists, n=98. B) Potential barriers in TCRT stated by German rheumatologists, n=98
Acknowledgements: We would like to thank all participants as well as all members of the Working Group Young Rheumatology. IH and MTH share last authorship.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (