

Background: Retinal vein occlusion (RVO) represents a common ophthalmological disorder, that untreated, often leads to severely impaired vision. The classic vascular risk factors, aging and glaucoma, represent the core pathogenic factors for RVO [1, 2, 3]. However, antiphospholipid syndrome (APS) [4, 5] has been involved in a non-negligible number of patients with RVO.
Objectives: The main objective of the present study was to assess the performance of the new 2023 ACR/EULAR classification criteria [6] for APS in a cohort of patients with RVO fulfilling the Sydney classification criteria [7].
Methods: Prospective study of consecutive patients with RVO diagnosed with APS in a third-level University Hospital. The new 2023 ACR/EULAR classification criteria for APS were applied to all patients. Vascular risk factors, antiphospholipid antibody (aPL) profile, clinical management, and clinical outcomes were assessed and compared between those fulfilling the Sydney and the 2023 ACR/EULAR criteria.
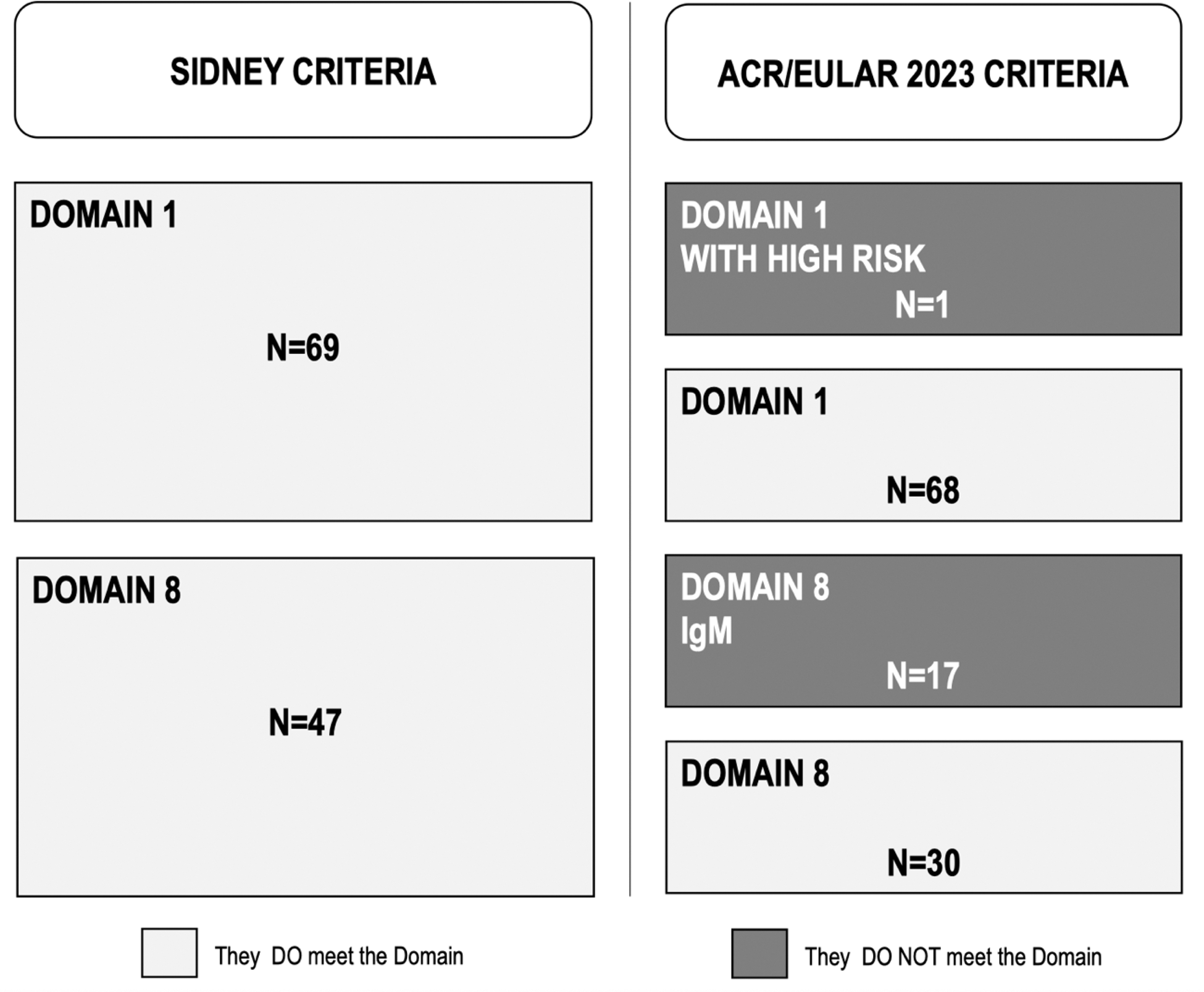
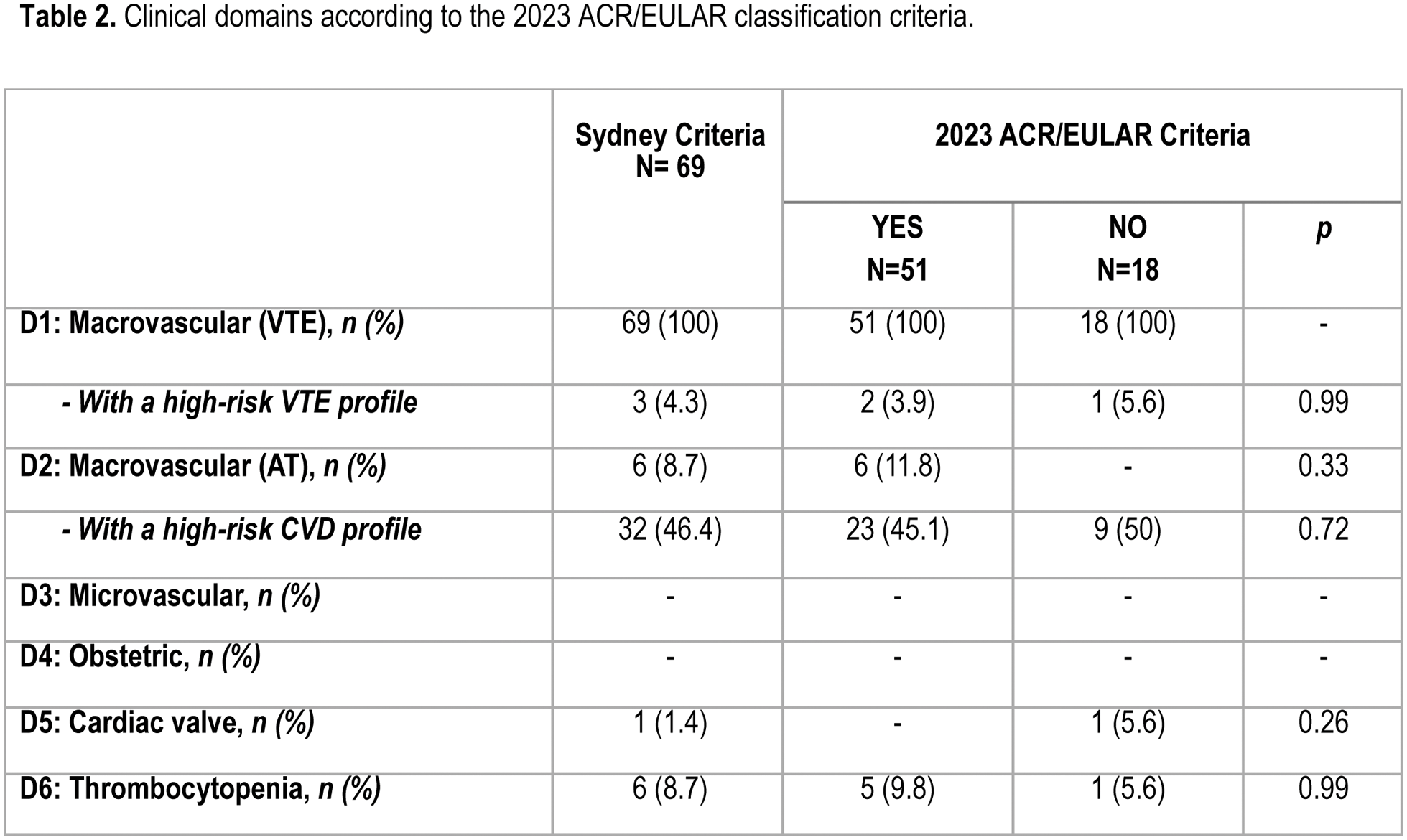
Results: Sixty-nine RVO-APS patients were included in the study. After applying the new classification criteria, 18 patients (26,1%) did not fulfill the new criteria for APS (Table 1) (Specifically, 17 (24.6%) were excluded due to the new Domain 8 (p<0.001), as they presented only aPL IgM serology, and 1 patient (1.4%) due to having high venous thromboembolic risk (VTE) with a clinical domain score <3. Interestingly enough, the presence of high arterial risk (45,1% vs 50%.; p=0.72) was greater than the presence of high VTE (3.9% vs 5.6%; p=0.99), in both, the 51 RVO-APS patients classifiedwith the 2023 ACR/EULAR criteria and the 18 cases excluded according to the new classification criteria (Table 2). Except for the expected differences in serological domains (Domain 7, p<0.001 and Domain 8, p<0.001), we did not find other significant differences in terms of prognosis or risk of recurrence between both groups of patients.
Conclusion: The implementation of the new ACR/EULAR 2023 classification criteria for APS resulted in the exclusion of about a quarter of previously diagnosed RVO-APS patients. The higher prevalence of manifestations of high arterial risk compared to high VTE among both newly classified and excluded APS patients highlights the importance of monitoring cardiovascular risk factors for both, the prevention and the management of potential retinal and cardiovascular events.
REFERENCES: [1] Cugati S, Wang JJ, Knudtson MD, Rochtchina E, Klein R, Klein BEK, et al. Retinal Vein Occlusion and Vascular Mortality. Ophthalmology. 2007 Mar;114(3):520–4.
[2] O’Mahoney PRA. Retinal Vein Occlusion and Traditional Risk Factors for Atherosclerosis. Archives of Ophthalmology. 2008 May 1;126(5):692.
[3] Napal Lecumberri JJ, Sedano Balbas C, Cañal Villanueva J, Hernández Hernández JL. Trombofilia y factores de riesgo vascular en la obstrucción venosa retiniana. Rev Clin Esp. 2013 Jun;213(5):229–34.
[4] Utz VM, Tang J. Ocular manifestations of the antiphospholipid syndrome. British Journal of Ophthalmology. 2011 Apr 1;95(4):454–9.
[5] Tektonidou MG, Andreoli L, Limper M, Amoura Z, Cervera R, Costedoat-Chalumeau N, et al. EULAR recommendations for the management of antiphospholipid syndrome in adults. Ann Rheum Dis. 2019 Oct;78(10):1296–304.
[6] Miyakis S, Lockshin MD, Atsumi T, Brach DW, Brey RL, Cervera R. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). Journal of Thrombosis and Haemostasis. 2006 Feb;4(2):295–306.
[7] Barbhaiya M, Zuily S, Naden R, Hendry A, Manneville F, Amigo M, et al. The 2023 ACR/EULAR Antiphospholipid Syndrome Classification Criteria. Arthritis & Rheumatology. 2023 Oct 28;75(10):1687–702.
Table 1. Patients classified as Antiphospholipid Syndrome by the Sydney and the 2023 ACR/EULAR criteria who meet or did not meet Domain 1 and Domain 8 from ACR/EULAR criteria.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (