

Background: Rheumatoid arthritis (RA) is a disease that causes joint dysfunction, which in turn triggers a decline in physical function. Mobility Disability, which is a concept that was proposed by the Japanese Orthopedic Association in 2007 as a national health policy target, is a condition of reduced mobility due to impaired physical function. Since RA, which leads to a decline in physical function, is a cause of Mobility Disability, there were reports indicating an association between RA and Mobility Disability [1]. However, there are few reports indicating an association between physical function assessment and Mobility Disability in patients with RA.
Objectives: The purpose of this study was to examine the relationship between Mobility Disability and assessment of physical function in RA patients.
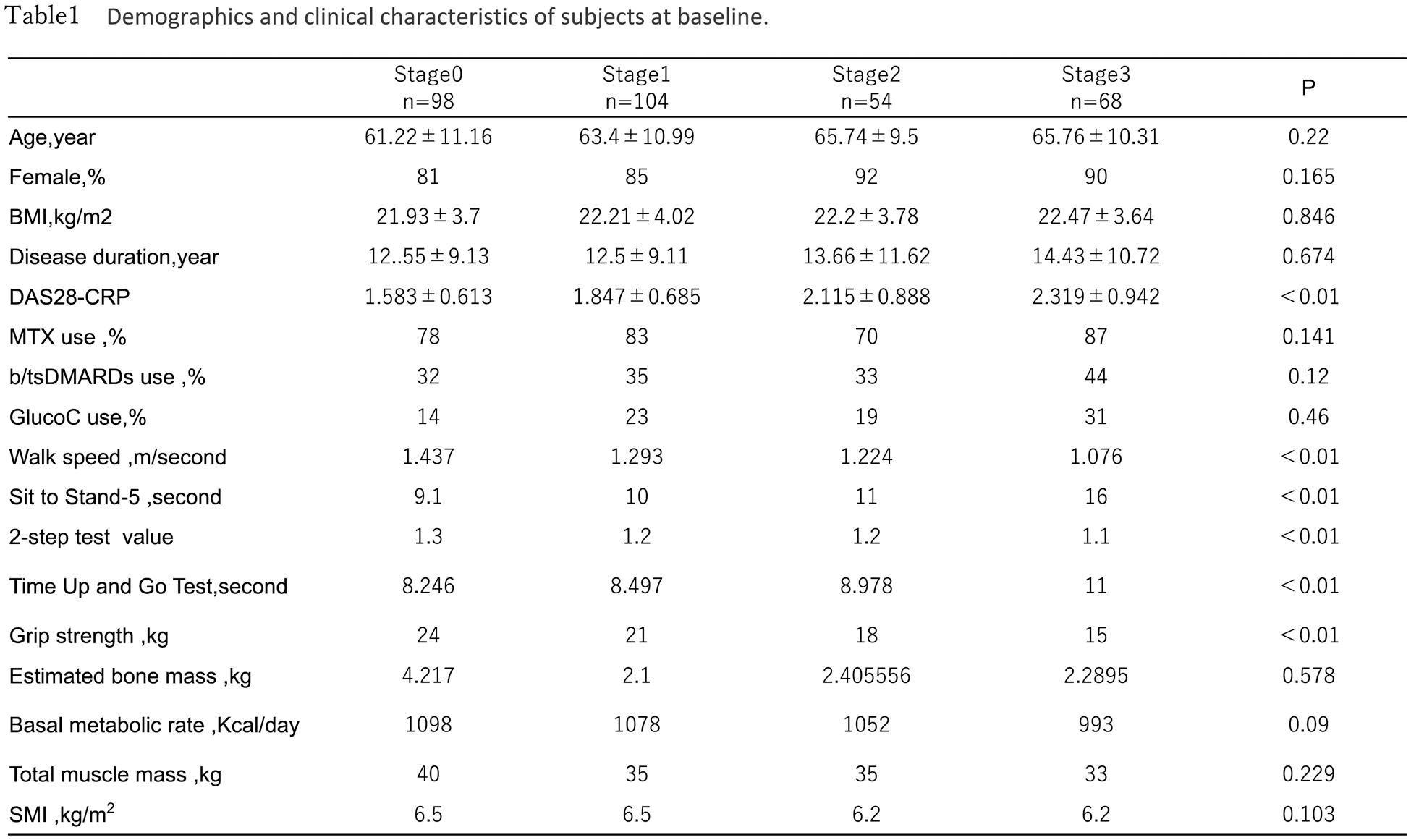
Methods: A total of 324 patients who participated in the prospective cohort study on frailty in RA patients (Fairy study) between March 2021 and December 2022 were included in the study. 25-question Geriatric Locomotive Function Scale (GLFS-25) is a screening tool consisting of 25 questions for the early detection of Mobility Disability, and a total score ranged from 0 (best) to 100 (worst). Mobility Disability stages are defined as follows: GLFS-25 <7 points for stage 0, 7-15 points for stage 1, 16-23 points for stage 2, and 24 points for stage 3 [2]. Basal metabolic rate, total muscle mass, and estimated skeletal muscle mass index (SMI) of the limbs were measured using bioelectrical impedance (BIA). Patient background, disease activity score (DAS-CRP), physical function (walking speed, Timed Up and Go Test [TUG], grip strength), basal metabolic rate, total muscle mass, and SMI were compared according to the Mobility Disability stage at the time of enrollment in the study, and analysis of variance was performed.
Results: Of the 324 patients, 30% was stage 0, 32% was stage 1, 16% was stage 2, and 22% was stage 3. Patient background for each Mobility Disability stage (0/1/2/3) was 61/63/66/66 years old (P=0.22), and DAS-CRP was 1.58/1.85/2.12/2.32 (P<0.01). Regarding physical function, walking speed was 1.44/1.29/1.22/1.08 m/sec (P<0.01), TUG was 8.25/8.50/8.98/11.0 seconds (P<0.01) and grip strength was 24/21/18/15 kg (P<0.01) (Table1). The basal metabolic rate was 1098/1078/1052/993 kcal (P<0.009), while total muscle mass was 40/35/35/33 (P=0.229) and SMI was 6.5/6.5/6.2/6.2 (P=0.103).
Conclusion: In RA patients, physical function declined as the Mobility Disability stage progressed, but the involvement of muscle mass was not clear.
REFERENCES: [1] Sobue Y, Kojima T, et al. Relationship between disease activity of rheumatoid arthritis and development of locomotive syndrome: A five-year longitudinal cohort study. Mod Rheumatol. 2021;31(1):101-7.
[2] Seichi A, Hoshino Y, et al. Development of a screening tool for risk of locomotive syndrome in the elderly: the 25-question Geriatric Locomotive Function Scale. J Orthop Sci. 2012;17(2):163-72.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (