

Background: Idiopathic orbital myositis (IOM) is characterised by non-infectious, non-neoplastic space occupying lesions in the orbit which leads to significant threat to vision if left untreated. Chronic IOM cases pose significant diagnostic challenges, and treatment often fails to ameliorate symptoms due to underlying muscle fibre damage. There is scarcity of data regarding treatment and prognosis, due to its rarity.
Objectives: Our aim is to characterise the clinical phenotypes of IOM and to evaluate the effectiveness and safety of various therapeutic strategies.
Methods: Patients diagnosed with IOM between January 2012 to December 2023 were included after ruling out other causes of orbital inflammation. Clinical features, laboratory parameters, imaging and treatment and its response were collected from electronic medical record. Treatment response defined as Complete Remission (CR), Partial Remission (PR) or No Response (NR) as per defined parameters.
Results: Among 10 patients diagnosed with IOM, majority were women (8/10) with mean age of 38.9 (±14.21) years. Demographic features, treatment details, outcome and comparison with different published cohort were summarised in Table 1. Bilateral orbital involvement was seen in seven patients. Six patients received corticosteroid pulse therapy in view of sight threatening involvement followed by oral steroids. Four patients were on steroids initially not on other Immunosuppressants (IS). Two patients who relapsed while tapering steroids were shifted to rituximab (RTX) and the other to mycophenolate mofetil (MMF). Both were in remission at the end of the follow-up period but developed permanent disability in the form of restricted eye movements. On median follow-up of 37.4 months (IQR 12-60). 6/9 had CR, 1/9 had PR.
Conclusion: IOM has variable presentations and often diagnosis is difficult to make. Treatment response with steroids is often excellent, however needs steroid sparing agent to prevent adverse events, relapses and permanent damage.
REFERENCES: [1] Yan J, Lu Z, Wu Z, Li Y, Chen Z, Mao Y, et al. Features associated with recurrence of idiopathic orbital inflammatory pseudotumor. Yan Ke Xue Bao. 2007 Mar;23(1):58–64.
[2] Ota M, Shimizu T, Yoshida H, Kawata A, Kinoshita M, Nakano S, et al. Clinical features and therapeutic responses of idiopathic orbital myositis. Neurol Clin Neurosci. 2015;3(2):63.
[3] Avni-Zauberman N, Tripathy D, Rosen N, Ben Simon GJ. Relapsing migratory idiopathic orbital inflammation: six new cases and review of the literature. Br J Ophthalmol. 2012 Feb;96(2):276-80. doi: 10.1136/bjo.2010.191866. Epub 2011 Apr 27.
[4] Montagnese F, Wenninger S, Schoser B. “Orbiting around” the orbital myositis: clinical features, differential diagnosis and therapy. J Neurol. 2016 Apr;263(4):631–40.
Comparison of our cohort from other previously published cohort.
| Number of patients/ Author | Benedikt GH [1]
| 5/Makiko Ota [2]
| 6/Noa Avni-Zauberman [3]
| F.Montagnese [4]
| Our cohort (10) |
|---|---|---|---|---|---|
| Age (mean) | 46 | 46 | 36 | 44 | 37 |
| Male/ Female | 3 | 4/1 | 2/4 | 3/4 | 2/8 |
| Clinical features | |||||
| Eye pain | 5 | 4 | 4 | 5 | 10 |
| Ptosis | 1 | 2 | - | - | 6 |
| Proptosis | 2 | 1 | 1 | - | 7 |
| Diplopia | 5 | - | 4 | 7 | 5 |
| EOM Restriction | 5 | 4 | 6 | 7 | 10 |
| LOOM | 3 | 5 | 9 | ||
| SEOM | 2 | 2 | 1 | ||
| MRI Orbit | |||||
| Enlargement of extraocular muscles | 5 | 5 | 10 | ||
| Other abnormality | 1 optic nerve | 2 optic nerve | |||
| Treatment | |||||
| Steroid dose | 5 | 1mg/kg | 1mg/kg | 1 mg/kg | 0.5-1mg/kg |
| Steroid pulse | 5 | 0 | - | 6 | |
| IS | 0 | ||||
| Methotrexate | 1 (on relapse) | 1(on relapse) | 1 | ||
| Azathioprine | 3 | 1 | 1 | ||
| Mycophenolate mofetil | - | - | 3 | ||
| Calcineurin inhibitor | - | - | - | ||
| Rituximab | - | - | - | - | 3 |
| Outcome | 2 PR,3 CR | On tapering steroid relapse | 1 PR
|
||
| Relapse at last follow up | 2 | 2 | 6 | 3 | 2 |
| Muscle atrophy/fibrosis on follow up | 2 | 2 | 6 | 2 | 1 |
Limited oligo symptomatic ocular myositis (LOOM) limited to muscle and conjunctival congestion and Severe exophthalmic ocular myositis (SEOM) presents with ptosis, chemosis and proptosis. Rarely peri scleritis, dacryoadenitis’s and peri neuritis can be seen. IS – Immunosuppressant.
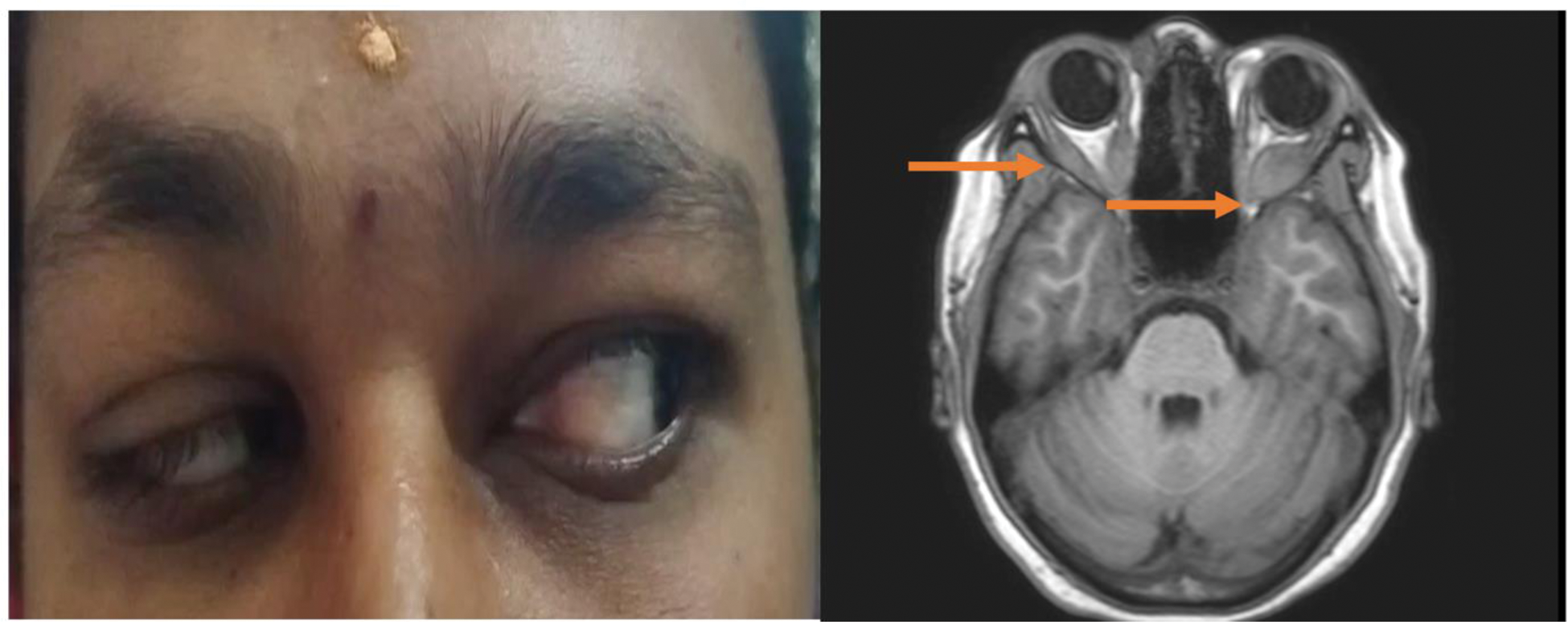
Showing proptosis in right eye and on imaging by MRI showing heterogenous enhancement in extra ocular muscles.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (