

Background: Lupus nephritis (LN) is a frequent manifestation of Systemic Lupus Erythematosus, and a major cause of morbidity. LN relapses are common, and accumulation of LN relapses is associated with increasingly lower response rates to treatments and progressively higher risk of kidney damage [1]. According to current international guidelines [2, 3], mycophenolate mofetil (MMF) and cyclophosphamide (CYC) are the agents of choice for the induction treatment of new-onset LN, with alternatives including Rituximab (RTX) or calcineurin inhibitors (CNI) such as tacrolimus or cyclosporine. Little is known about the differential efficacy of distinct induction treatments for lupus nephritis at onset and relapses and about the potential influence of LN treatment at onset on treatment efficacy later on.
Objectives: To assess whether immunosuppressants used for LN may have distinct patterns of efficacy at LN onset and relapse.
Methods: This is a retrospective, double-center, observational study collecting data from LN patients between 1964 and 2024. Renal outcomes were categorized according to EULAR definitions as Complete Response (CR), Partial Response (PR), or Failure (FL), and renal response was assessed as the best response ever for each renal flare. Patients who received a different induction treatment compared to LN onset were classified as “switchers”. Statistical analyses were performed using SPSS software. Continuous and categorical data were expressed as medians (IQR1-IQR3). Categorical data were compared using the Chi-square test. Statistical significance was set at p ≤ 0.05.
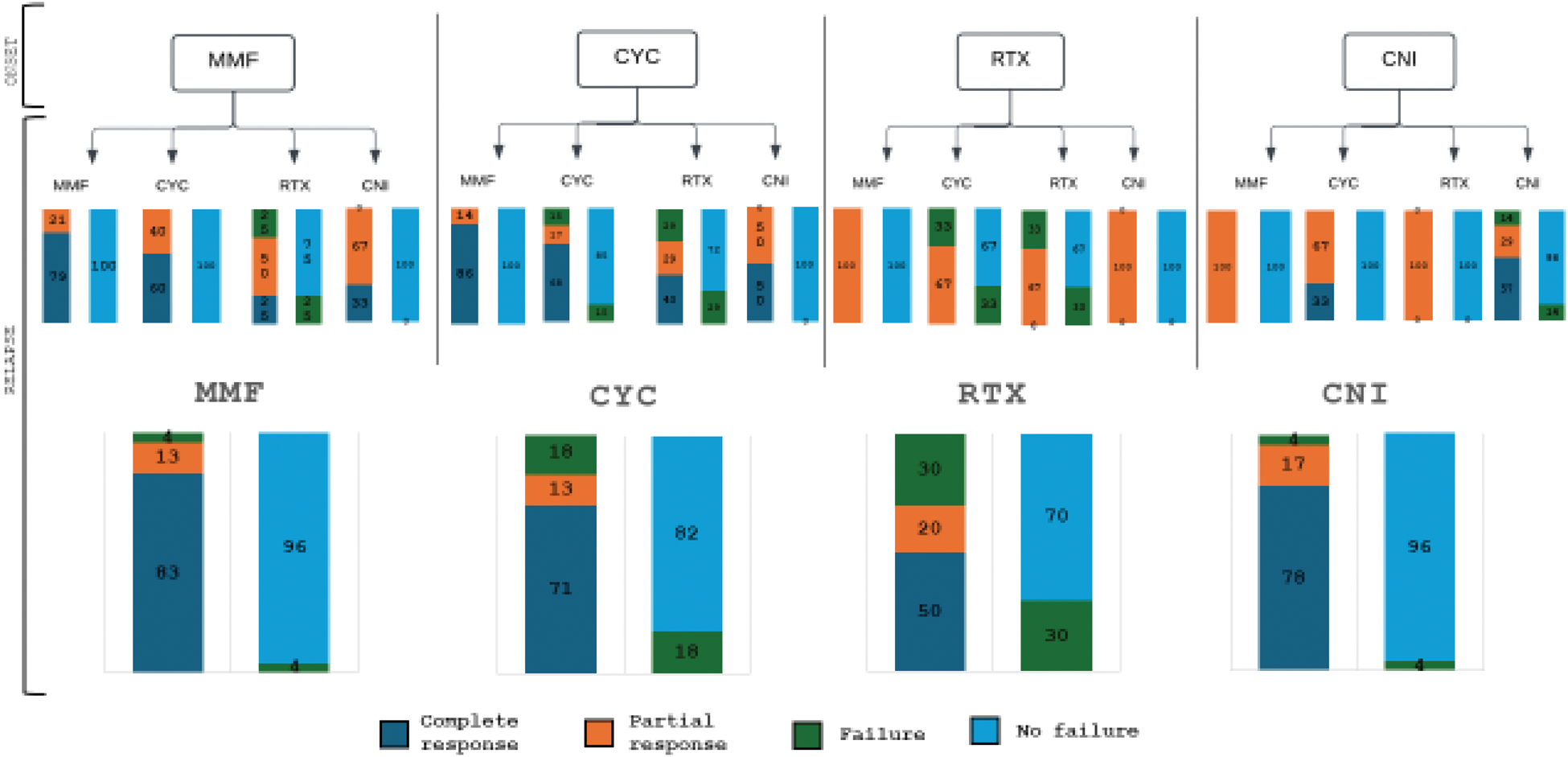
Results: Data from 286 patients (89% women) and 474 LN episodes (N= 188 relapses) were included: at the time of LN onset patient age was 32 (24-41) years, while 111 patients (39%) had one or more relapse(s) 37 (3-88) months after LN onset. Relapses were followed-up for 155 (69-261) months. Renal biopsy was performed in 310 cases: class IV nephritis were the most prevalent (32%), followed by class V (25%) and class III (15%). At onset, LN remission was induced with CYC (43%), MMF (20%), CNI (4%) and RTX (3%), while relapses were mainly treated with CYC (29%) and MMF (25%), followed by CNI (12%) and RTX (5%). Other patients received azathioprine or steroid therapy only. The outcomes for the first episodes and subsequent flares were 76% and 79% CR, 12% and 10% PR, and 11% FL, respectively. Overall, MMF, CNI, and CYC showed high rates of CR (83%, 78%, and 71%), but CYC also had a higher rate of FL (18% vs 4% with other treatments). Of the 111 relapsing patients, 59% were switchers. Numerically higher CR rates were observed among switchers than among other patients (94% vs 76%, p=0.08). Switchers to MMF had significantly higher CR rates when induced with CYC than with RTX at LN onset (86% vs 0%, p = 0.03). A similar trend was observed when comparing MMF non-switchers to CYC->MMF switchers (79% vs 86%, p=0.07). Switchers to CYC from MMF or CNI had no FL. CR were similar among CYC non switchers and MMF>CYC switchers. Response rates at relapse were similar between CNI switchers and non-switchers, with only 4% overall FL rate. No CR were observed in relapsing patients induced with RTX at LN onset, irrespectively of subsequent treatments (Figure 1).
Conclusion: MMF and CYC are most effective to induce remission at LN onset and relapse, with MMF showing lower FL rates at relapse. However, patients on CYC had a rather high number of flares. CNI are also associated with low FL rate at LN relapse. Relapses in patients receiving RTX at LN onset are probably more severe and might require more aggressive treatments. Notably, switching from LN onset regimen at relapse does not reduce and may be associated with higher CR rates.
REFERENCES: [1] Ioannidis, J. P. A. et al. Remission, relapse, and re-remission of proliferative lupus nephritis treated with cyclophosphamide. Kidney Int 57 , 258–264 (2000).
[2] KDIGO 2024 Clinical Practice Guideline for the management of LUPUS NEPHRITIS. Kidney Int 105 , S1–S69 (2024).
[3] Fanouriakis, A. et al. EULAR recommendations for the management of systemic lupus erythematosus: 2023 update. Ann Rheum Dis 83 , 15–29 (2023).
differential percentage outcome at LN onset and relapse among distinct regimens
Acknowledgements: NIL.
Disclosure of Interests: Giuseppe Alvise Ramirez Amgen, GSK, AZ, Vifor, Gabriele Domenico Gallina: None declared , Chiara Calabrese: None declared , Serena Nannipieri: None declared , Raffaele Ceniccola: None declared , Marta Calatroni: None declared , Francesco Reggiani: None declared , Giovanni Benanti: None declared , Enrica Bozzolo: None declared , Luca Moroni: None declared , Marco Matucci-Cerinic: None declared , Gabriella Moroni: None declared , Lorenzo Dagna: None declared .
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (