

Background: The Triglyceride-Glucose-BMI index (TyG-BMI) is a reliable method for detecting insulin resistance (IR), with effectiveness comparable to the gold standard: the hyperinsulinemic-euglycemic clamp. Elevated TyG-BMI levels have been associated with an increased cardiovascular (CV) risk, as well as subclinical atherosclerosis and cardiac dysfunction. Both IR and rheumatoid arthritis (RA) promote a state of hyperglycemia that disrupts insulin signaling. Therefore, the use of TyG-BMI as a screening tool for CV risk assessment in this population is proposed, offering a practical and effective alternative for screening.
Objectives: To evaluate the association of the TyG-BMI Index with carotid plaque, left ventricular geometry, and subclinical cardiac dysfunction in patients with RA.
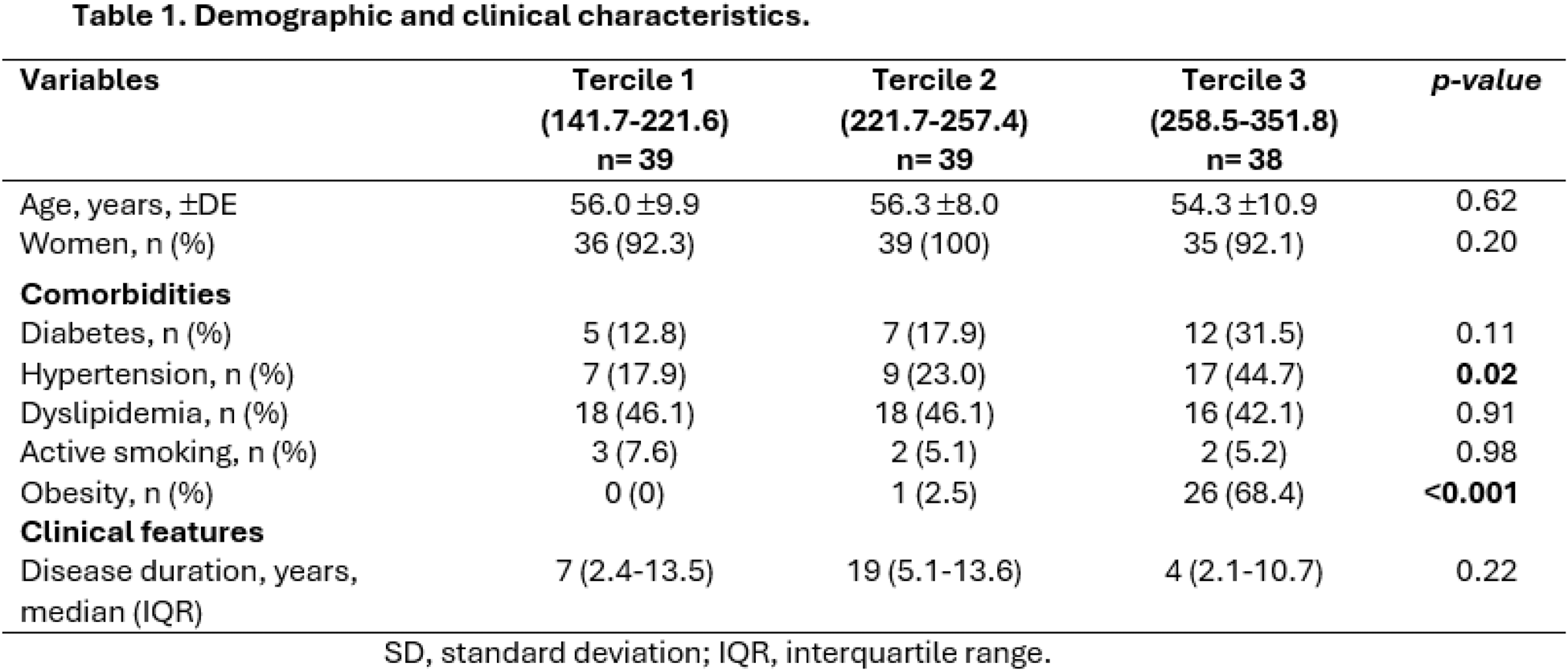
Methods: A Cross-sectional, descriptive, comparative study was conducted. Patients aged 30 to 75 with RA who met the 2010 ACR/EULAR criteria were included. Those with CV disease history were excluded. Carotid ultrasound and transthoracic echocardiogram were performed on all participants. CP was defined as a diffuse carotid intima-media thickness (IMT) ≥1.2 mm or focal thickness ≥0.8 mm. The echocardiographic assessment included left ventricular mass index (LVMI), relative wall thickness (RWT), tricuspid annular plane systolic excursion (TAPSE), and left ventricular ejection fraction (LVEF). Subclinical diastolic dysfunction (SDD) was defined according to the 2016 American College of Cardiology classification, and subclinical systolic dysfunction (SSD) of the left ventricle (LV) was defined as a global longitudinal strain (GLS) >-18%. To calculate the TyG-BMI index, serum triglyceride (TG) levels, fasting blood glucose (FBG), and body mass index (BMI) were used with the following formula: TyG-BMI Index = Ln [TG (mg/dL) × FBG (mg/dL)/2] × BMI. Participants were categorized into tertiles based on the TyG-BMI: ranges <221.7 for the first tertile, 221.7 to 257.4 for the second tertile, and values >257.4 for the third tertile. Group distribution was evaluated using the Kolmogorov-Smirnov test. Comparisons were made using the Chi-square test, ANOVA, or Kruskal-Wallis test. A p-value ≤0.05 was considered statistically significant.
Results: A total of 116 patients with RA were recruited: 39 in the first and second tertiles, and 38 in the last tertile according to the TyG-BMI index (Table 1). The majority were women, with an average age of 55.5 years. Although not statistically significant, TyG-BMI index values ≥258.5 showed a higher frequency of comorbidities (except dyslipidemia). In the second tertile, the highest prevalence of unilateral CP was observed (28.2%, p=0.89), the lowest presence of bilateral CP (12.8%, p=0.84), and the major prevalence of concentric remodeling (43.5%, p=0.054). In the third tertile, lower values of LVEF were found compared to the first tertile, with statistical significance in the Tukey post-hoc analysis (62.1 ± 4.9 vs 59.5 ± 4.2, p=0.045). Complete results are in Table 2.
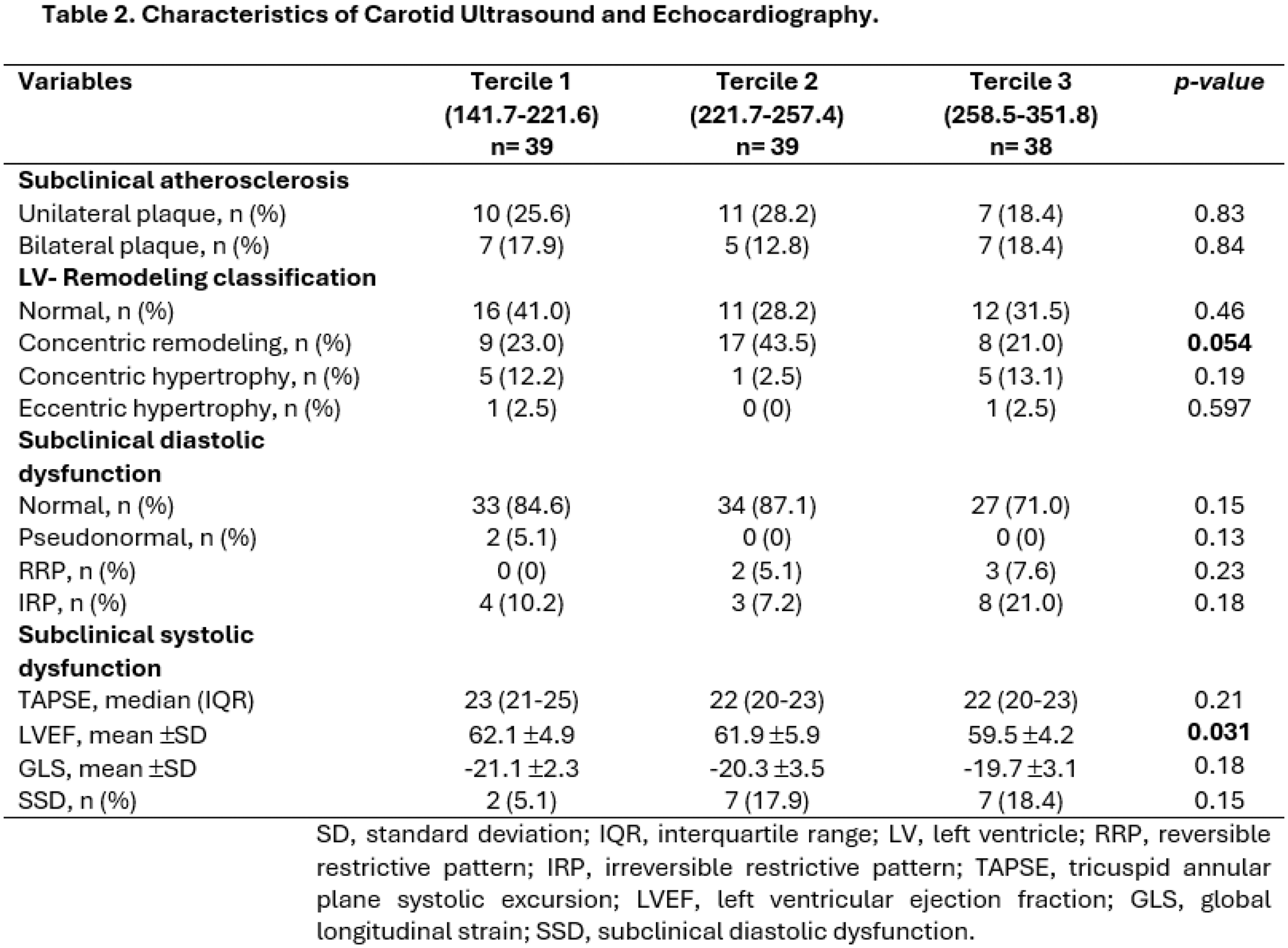
Conclusion: The TyG-BMI index is not associated with the presence of CP; however, its potential to identify subclinical systolic dysfunction (SSD) is notable, given the lower LVEF values in ranges ≥258.5. This is possibly due to the higher prevalence of obesity and hypertension, along with other comorbidities. Despite this, studies with larger sample sizes are needed. It is essential to integrate echocardiographic and carotid ultrasound assessments into CV risk evaluation for the early detection of these abnormalities.
REFERENCES: [1] Wang R, Cheng X, Tao W. Association between triglyceride glucose body mass index and cardiovascular disease in adults: evidence from NHANES 2011-2020. Front Endocrinol (Lausanne). 2024;15:1362667. doi:10.3389/fendo.2024.1362667.
[2] Yang S, Shi X, Liu W, Chen X, Zhang Y, Huang J. Association between triglyceride glucose-body mass index and heart failure in subjects with diabetes mellitus or prediabetes mellitus: a cross-sectional study. Front Endocrinol (Lausanne). 2023;14:1294909. doi:10.3389/fendo.2023.1294909.
[3] Nicolau J, Lequerré T, Bacquet H, Vittecoq O. Rheumatoid arthritis, insulin resistance, and diabetes. Joint Bone Spine. 2017;84(4):411-6. doi:10.1016/j.jbspin.2016.09.001.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (