

Background: Around 1% of Canadians live with rheumatoid arthritis (RA), experiencing unpredictable flare-ups, leading to pain, fatigue, psychological distress, and reduced quality of life. Individuals with RA also have increased risks of cardiovascular disease and other chronic conditions. Physical activity (PA) is recommended to counteract debilitating symptoms, improve overall health, and reduce chronic disease risk in RA. However, PA levels among people with RA remain significantly lower than in the general population, largely due to significant PA barriers (e.g. pain and fatigue, concerns about safety, lack of tailored support, and limited RA-specific guidance). Tailored PA interventions are essential to increase PA levels among people with RA. To be effective, these interventions must target RA-specific PA barriers and facilitators using theory-driven, evidence-based behavior change techniques. While reviews of PA determinants exist in this population, there is a lack of patient-led priority setting to understand which determinants are most important to individuals with RA. Furthermore, the PA behavior change literature suggests that the linkage of patient priorities to behavioral theories is crucial for effective intervention design.
Objectives: We aimed to (1) determine the most important PA determinants for individuals with RA and (2) map determinants to the behavior change wheel, informing future theory-based PA interventions.
Methodological study overview.
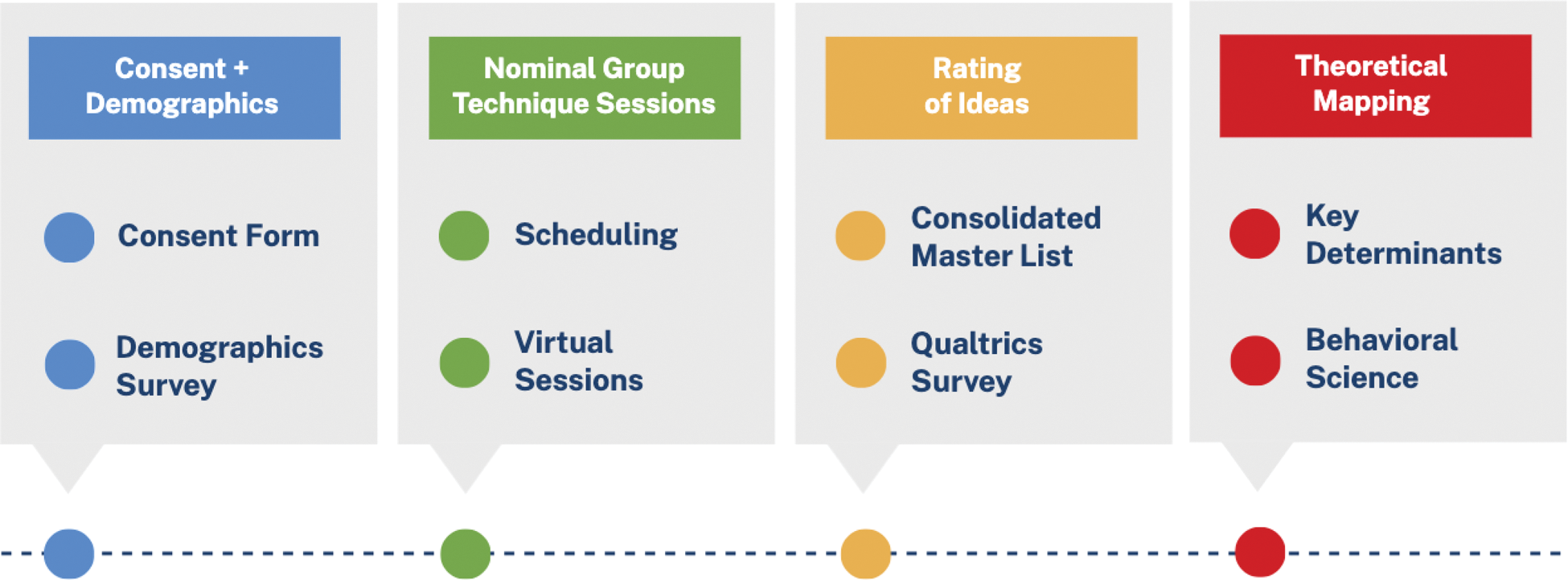
Methods: Nominal group technique (NGT) sessions were held with adults living with RA using a patient-oriented research approach (see Figure 1 for methodological overview). Participants completed a baseline questionnaire to report demographics and PA levels. Virtual NGT sessions were led by 2 co-facilitators from the research team. Sessions included introductions, silent idea generation, idea sharing, and group discussion to refine ideas. Barrier and facilitator lists were consolidated into a survey that participants completed post-session to rate the importance of each determinant on a 9-point Likert scale. Descriptive statistics were calculated for participant characteristics. Determinants were ranked in order of mean importance rating, followed by theoretical mapping of determinants using the behavior change wheel (BCW, i.e. grouping into capability, opportunity, or motivation categories) and theoretical domains framework (TDF, i.e. linking to one of 14 behavioral domains). Lastly, relevant intervention functions and behavior change techniques were selected to target each determinant.
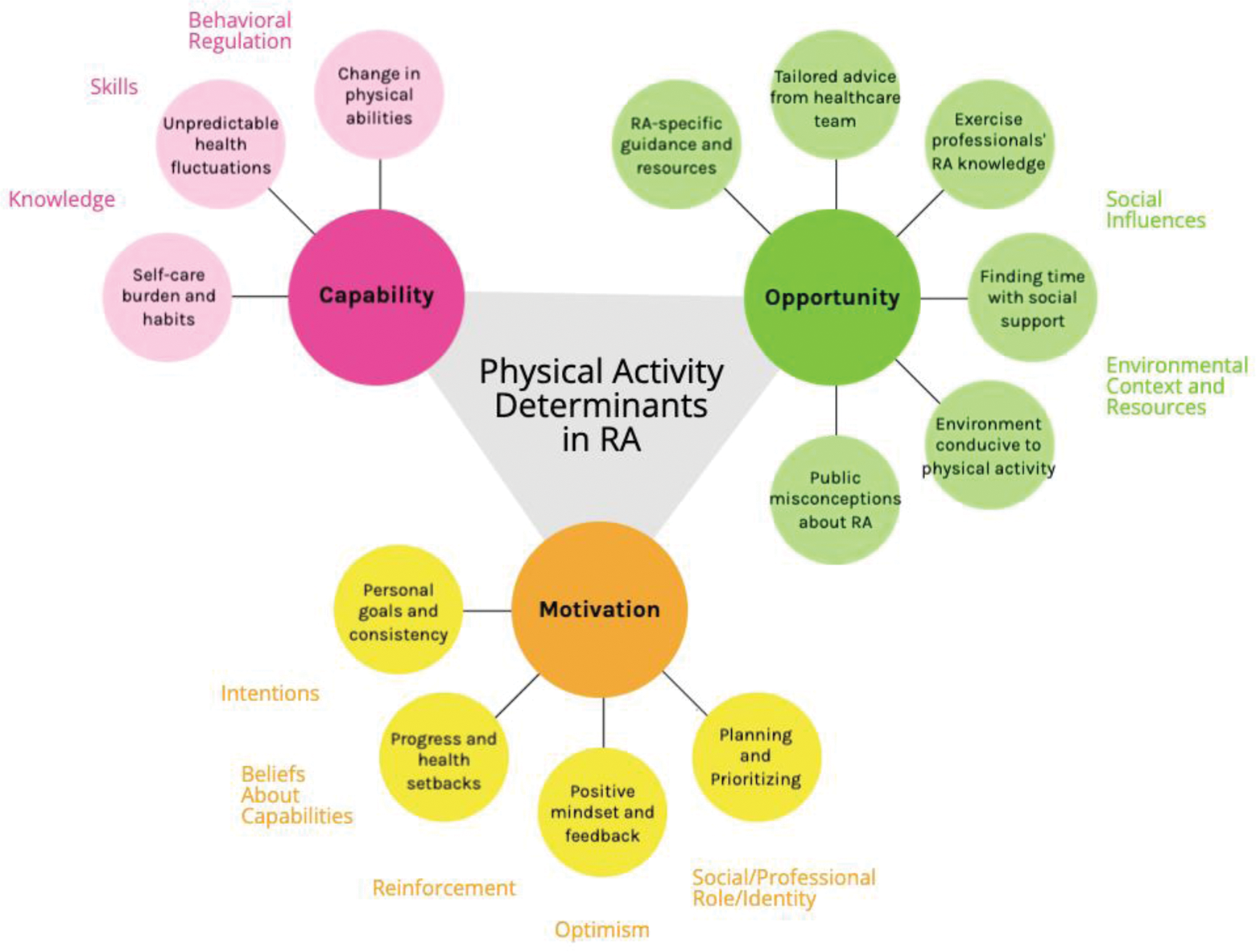
Results: A total of 14 individuals with RA participated in 3 NGT sessions that lasted 55-75 minutes. Participants had a mean age of 58.1 (SD=13.4) years and 20.0 (SD=21.8) years of living with RA. 85.7% were female, 78.6% white, and 85.7% had a university-level education. All participants were physically active, with a mean of 1.0 (SD=1.6) instances of high-intensity PA and 4.3 (SD=3.1) instances of moderate-intensity PA per week. In total, 22 PA barriers and 25 PA facilitators were discussed across 4 categories: personal factors, social support, physical condition, and environmental factors. The 3 most important barriers (importance ratings: 7.1-7.4/9) were (1) unpredictable symptom fluctuations, (2) chronic fatigue, and (3) lack of RA-specific PA knowledge. The 3 most important facilitators (importance ratings: 7.6-7.9/9) were (1) motivation to maintain function, (2) knowledge about tailoring PA to RA, and (3) increased confidence after experiencing PA benefits. After theoretical mapping (Figure 2), 3 determinants mapped to capability, 6 to opportunity, and 4 to motivation. Behavioral domains to target in future interventions include skills (capability), social influences (opportunity), and beliefs about capabilities (motivation), among others.
Results from theoretical mapping. Key determinants identified during the NGT are shown using colored circles. Determinants were mapped to TDF behavioral domains, which are displayed in colored text.
Conclusion: The priority setting identified the most important PA determinants among individuals with RA, which related to personal factors, social support, physical condition, and environmental factors. Theoretical mapping provided evidence-based, actionable insights for targeting these determinants and improving capability, opportunity, and motivation for PA in RA populations. These findings can inform development of resources, interventions, and clinical practices that support PA behavior change in RA care.
REFERENCES: NIL.
Acknowledgements: We would like to thank our patient partners who contributed their valuable ideas during the nominal group technique sessions. The project would not have been possible without their input and enthusiasm.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (