

Background: The cardiovascular risk (CVR) is increased in both rheumatoid arthritis (RA) and Sjögren’s disease (SjD), contributing to disease morbidity. However, how the associated SjD affects CVR in patients with RA is not clear.
Objectives: Our aim was to investigate the impact of associated SjD on the CVR of RA patients.
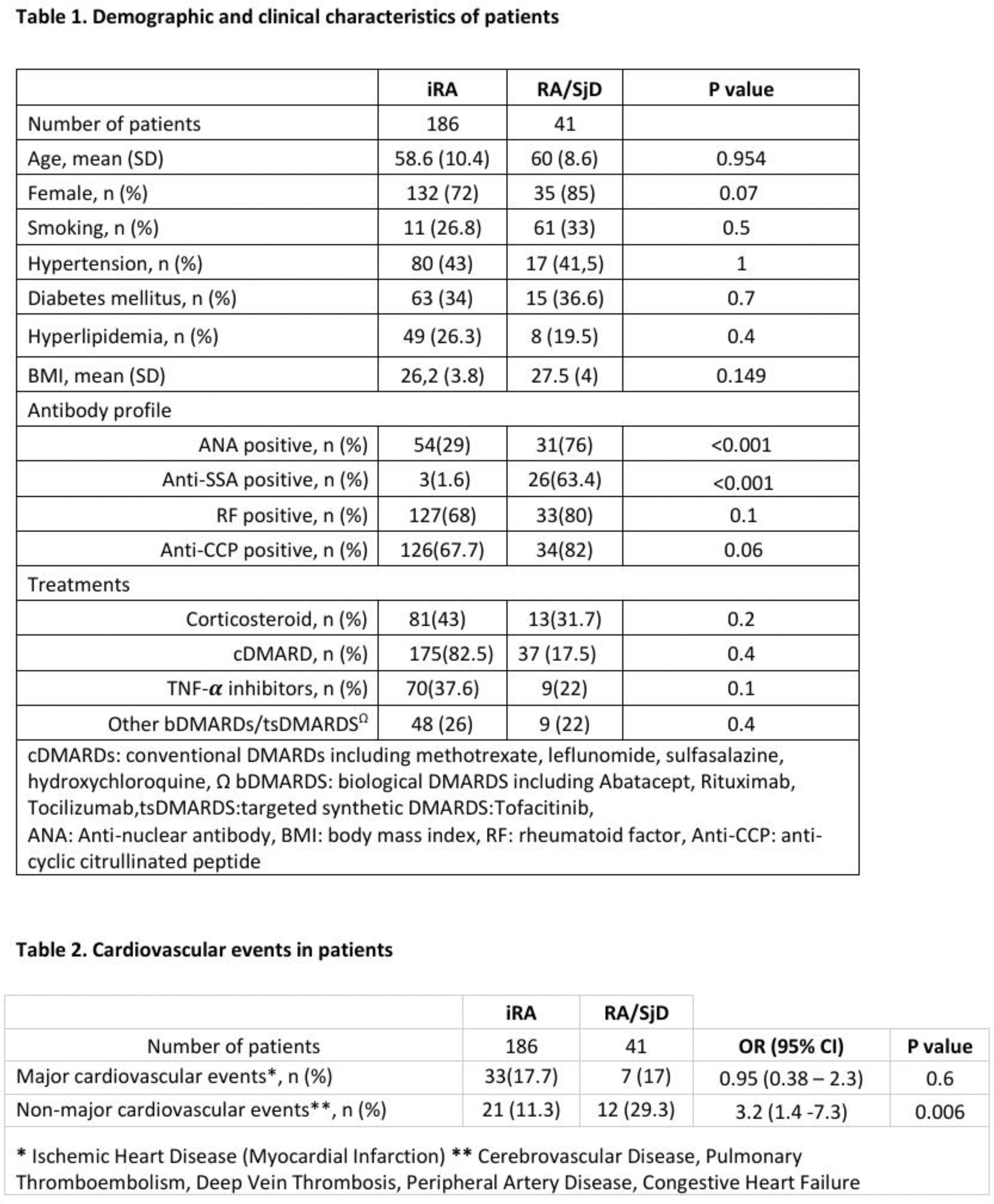
Methods: The medical records of patients with RA registered at our rheumatology outpatient clinic between 1995 and 2024 were reviewed. Demographic and clinical data were recorded according to a standardized data table, including major cardiovascular events (acute myocardial infarction, ischemic heart disease) and non-major cardiovascular events (cerebrovascular diseases, thromboembolic events, heart failure, peripheral vascular disease). The frequency of major and non-major CV events, as well as associated variables, were compared in two groups of patients defined by the presence of associated SjD. Patients with age below 18 years or above 75 years, diagnosis of SjD, SjD has been associated to autoimmune conditions other than RA, history of chronic HIV/HCV infection, IgG4-related disease, sarcoidosis, or lymphoproliferative disorders, failure to attend follow-up in the last year were excluded.
Results: After the exclusion of 828 ineligible patients due to insufficient data to assess CVR and follow-up duration, 186 patients with isolated RA (iRA) and 41 patients with RA and SjD (RA/SjD) were included. Demographic and clinical characteristics were given in Table 1. The prevalence of major CV events were similar. However, non-major cardiovascular events were more common in the RA/SjD group (29% vs. 11%, p=0.006). Among the RA/SjD patients, the frequency of non-major cardiovascular events was higher in patients with anti-SSA positive compared to anti-SSA negative patients (58% vs. 42%, p=0.012). In the iRA group, major cardiovascular events were related to higher disease activity, age, BMI, and steroid use. In addition, all iRA patients with non-major cardiovascular events were under biologic therapy. Thus, it is anticipated that their disease activity was high during at least one phase of their disease.
Conclusion: This study highlights that the prevalences of major CV events were similar between patients with iRA and those with RA and associated SjD. However, non-major CV events were more common in patients with RA/SjD compared to iRA. Notably, anti-SSA positivity appears to further amplify this risk in RA/SjD patients. In the iRA group, major CV events were linked to traditional risk factors such as advanced age, higher BMI, and steroid use, as well as disease severity. The findings suggest that associated SjD may enhance inflammatory processes in patients with RA, potentially contributing to the development of non-major CV events. The observed association between biologic therapy and non-major CV events warrants further investigation to determine whether this is due to residual disease activity or other factors.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (