

Background: Fatigue is recognised as one of the most challenging symptoms to manage in inflammatory rheumatic and musculoskeletal diseases (iRMD) [1] and is one of the most important outcomes for patients. While data on Rheumatoid Arthritis (RA), axial spondyloarthritis (axSpA), and Systemic Lupus Erythematosus (SLE) have been published, descriptions of fatigue in other iRMD are limited.
Objectives: To compare the distribution and development of fatigue between 2007 and 2023 in 12 different iRMD: RA, Adult Onset Still Syndrome (AOSD), axSpA, Psoriatic Arthritis (PsA), SLE, Sjögren’s Syndrome (SjS), Systemic Sclerosis (SSc), Idiopathic Inflammatory Myopathies (IIM), Mixed Connective Tissue Diseases (MCTD), Polymyalgia Rheumatica (PMR), Giant Cell Arteritis (GCA) and ANCA-associated Vasculitides (AAV).
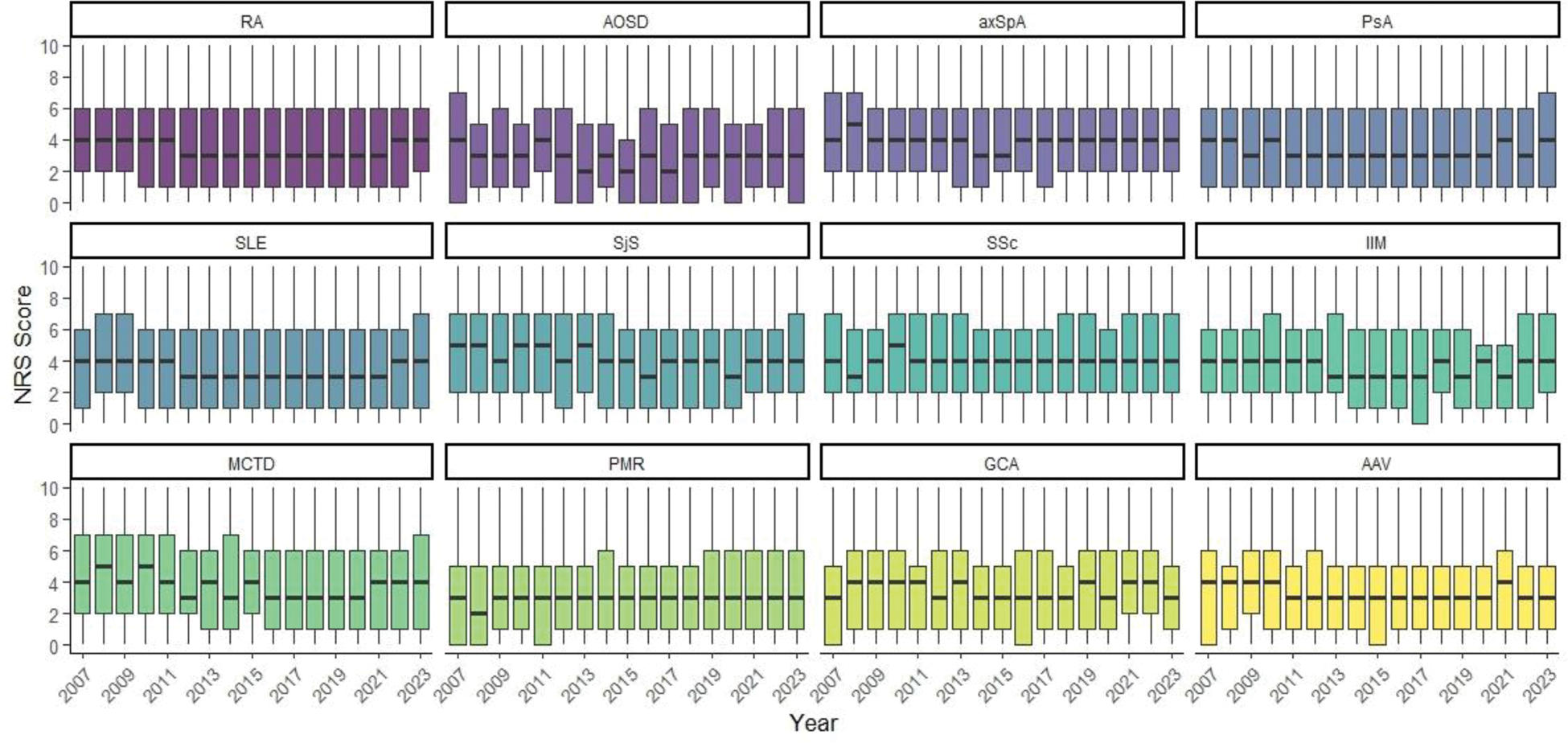
Methods: Adult patients with iRMD documented within the National Database of the German Collaborative Arthritis Centres were included. Fatigue was monitored by patients on numeric rating scales (NRS, 0-10). Present fatigue was defined as NRS >1 and severe fatigue as NRS >6. The frequency and severity of fatigue was compared between rheumatic diseases, years of documentation and gender. Boxplots show the distribution and development of fatigue.
Results: Each year, between 8,000 and 10,000 patients reported fatigue; for 2023, the characteristics are shown in Table 1. Averaged across all years, the highest proportion of fatigue was observed in patients with axSpA (80%) and SSc (79%), followed by SjS (76%), IIM and MCT (74%), RA and PsA (73%), SLE (71%), GCA (70%), AAV (69%), PMR (68%), while AOSD patients reported the lowest proportion (63%). Female patients had a higher proportion of severe fatigue in all iRMD, but most affected were women with axSpA (31% vs. 19% in men), PsA (27% vs. 15%), SSc (27% vs. 24%) and SjS (26% vs. 15%). Figure 1 shows no relevant improvement in patients fatigue assessments in all iRMD since 2007. Median values for SSc, SjS, axSpA and MCTD range from 3 to 5, for IIM, RCA, RA, SLE, PsA and AAV from 3 to 4, for AOSD from 2 to 4 and the lowest values had patients with PMR (2 to 3). We also observed a low variability of the interquartile range in all iRMD.
Characteristics of patients who documented fatigue from 2023
| RA
| AOSD
| axSpA
| PsA
| SLE
| SjS
| SSc
| IIM
| MCTD
| PMR
| GCA
| AAV
|
||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age in years | |||||||||||||
| Mean
| 62.9 (13.9) | 47.5 (13.2) | 50.9 (14.0) | 57.5 (14.3) | 48.0 (14.4) | 55.8 (14.6) | 57.5 (13.9) | 54.6 (17.0) | 53.5 (15.2) | 72.8 (8.9) | 74.2 (8.8) | 61.8 (13.9) | |
| Female (%) | 75 | 62 | 37 | 54 | 89 | 92 | 79 | 62 | 87 | 60 | 76 | 55 | |
| Disease duration in years | |||||||||||||
| Mean (SD) | 15.3 (11.4) | 12.7 (9.6) | 19.9 (13.2) | 15.1 (11.6) | 18.4 (11.1) | 14.3 (9.2) | 12.7 (9.4) | 11.2 (8.5) | 17.3 (9.8) | 6.2 (6.8) | 6.3 (5.5) | 12.2 (8.2) | |
| Median | 13.0 | 10.7 | 18.0 | 12.0 | 17.8 | 13.0 | 11.0 | 11.0 | 17.2 | 3.8 | 4.4 | 10.4 | |
| RAID-Fatigue (0-10)* | |||||||||||||
| Mean (SD) | 4.0 (2.9) | 3.5 (3.2) | 4.3 (2.9) | 4.3 (3.0) | 4.2 (3.0) | 4.3 (3.0) | 4.5 (3.0) | 4.7 (2.9) | 4.2 (3.2) | 3.5 (2.8) | 3.6 (2.8) | 3.6 (2.9) | |
| Fatigue >1 (%) | 76 | 63 | 80 | 78 | 76 | 77 | 81 | 83 | 75 | 73 | 71 | 71 | |
| Fatigue >6 (%) | 24 | 27 | 26 | 29 | 29 | 31 | 33 | 33 | 28 | 19 | 21 | 19 | |
SD Standard Deviation, * RAID Rheumatod Arthritis Impact of Disease, 0 = no fatigue to 10 = most severe fatigue
Boxplots of Fatigue per Year and Diagnosis
NRS numeric rating scale Score of fatigue from 0 to 10, Line represents the Median, Boxes show the interquartile range, Rheumatoid Arthritis (RA), Adult Onset Still Syndrome (AOSD), axial Spondyloarthritis (axSpA), Psoriatic Arthritis (PsA), Systemic Lupus Erythematosus (SLE), Sjögren’s Syndrome (SjS), Systemic Sclerosis (SSc), Idiopathic Inflammatory Myopathies (IIM), Mixed Connective Tissue Diseases (MCTD), Polymyalgia Rheumatica (PMR), Giant Cell Arteritis (GCA), ANCA-associated Vasculitides (AAV).
Conclusion: Fatigue is a frequent symptom across various iRMD, with axSpA, SSc and SjS being most severely affected. Since 2007 there was no relevant improvement in frequency and severity of patient reported fatigue across all diagnoses. Implications include regular assessment and (individual) therapeutic management of fatigue.
REFERENCES: [1] PMID: 38050029.
Acknowledgements: We thank all participating rheumatologists and patients for their valuable contributions. Funding: The National Database of the German Collaborative Arthritis centers is supported by the Association of Regional Cooperative Rheumatology Centres, the German Society for Rheumatology and joint contributions to the Rheumatological Training Academy and the German Rheumatism Research Centre by the following members of the Working Group of Corporate Members of the German Society for Rheumatology: AbbVie, AstraZeneca, GALAPAGOS, GSK, Medac, Pfizer and UCB.
Disclosure of Interests: Katja Thiele: None declared, Katinka Albrecht: None declared, Johanna Callhoff The author has received speaker honoraria from Janssen, Pfizer, Idorsia, Kirsten Karberg: None declared, Benjamin Köhler: None declared, Jutta Richter: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (