

Background: Systemic lupus erythematosus (SLE) is an autoimmune disorder marked by significant clinical diversity and considerable variability in disease course and outcomes. Cluster analysis in heterogeneous diseases can identify distinct patient subsets, offering potential value in predicting treatment response patterns and facilitating the development of personalized monitoring plans.
Objectives: To identify clinical phenotypes of SLE through cluster analysis and assess their value as predictors of treatment response.
Methods: The study included 280 Ukrainian SLE patients (aged 37 [25-48] years; 87,1% females) not optimally controlled at cohort entry. Patients were classified via hierarchical cluster analysis based on the Ward method and the Euclidean distance, using the following variables: sex, age at disease onset, SLE disease activity index (SLEDAI-2K), SLICC/ACR damage index (SDI), and cumulative clinical manifestations (arthritis, nephritis, serositis, lymphadenopathy, mucocutaneous, vascular, neurological, cardiac and pulmonary involvement, fever). At the baseline visit, all patients were assigned clinically appropriate standard-of-care SLE therapy according to current EULAR recommendations. At the follow-up visit (6±2 months), 108 patients were assessed for treatment response, defined as a decrease in SLEDAI-2K score of ≥4 points from baseline and/or achievement of low disease activity state (SLEDAI-2K ≤4, no activity in major organs, no new disease activity, physician global assessment (PGA) ≤1, prednisolone dose ≤7,5 mg/day, maintenance dose of immunosuppressive drugs) [1] or remission (SLEDAI-2K=0, PGA <0.5, prednisolone dose ≤5 mg/day, maintenance dose of immunosuppressive drugs) [2]. Logistic regression analysis was performed to assess the association between clustering membership and treatment response rates.
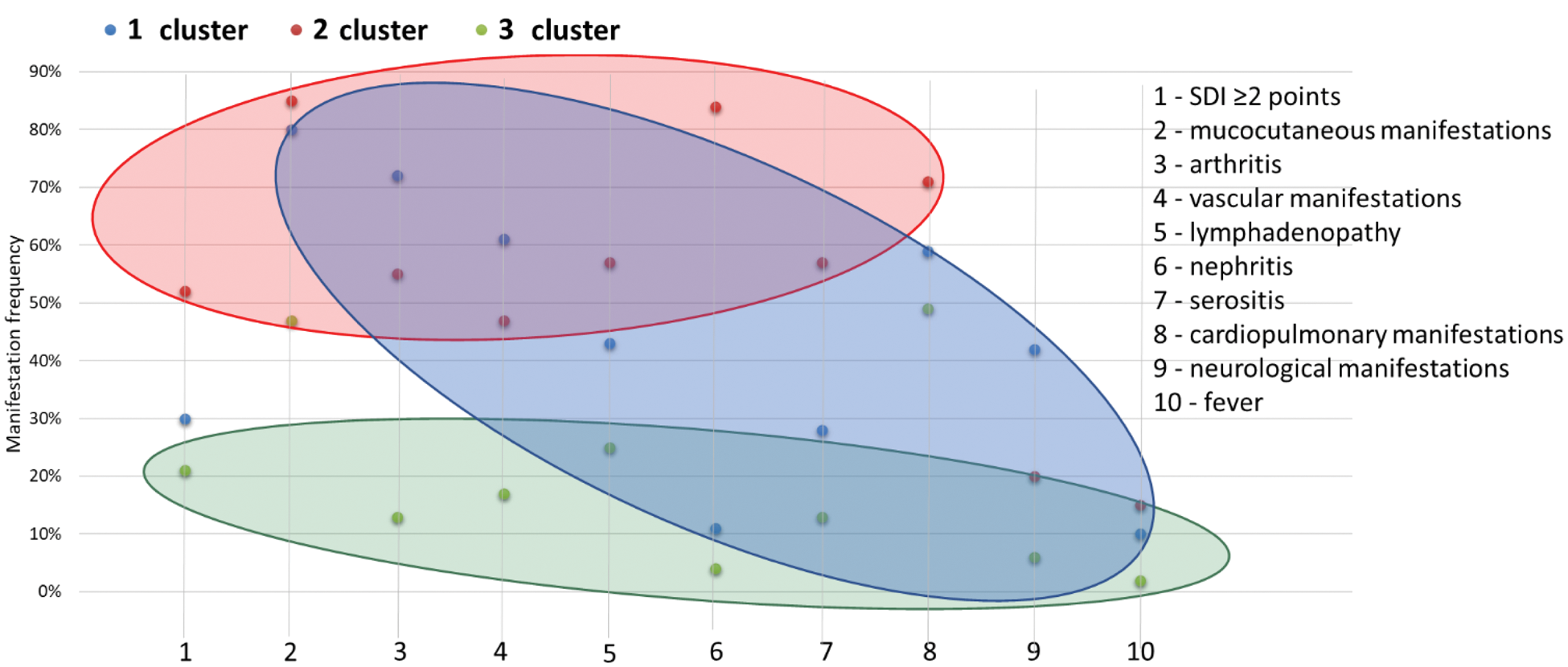
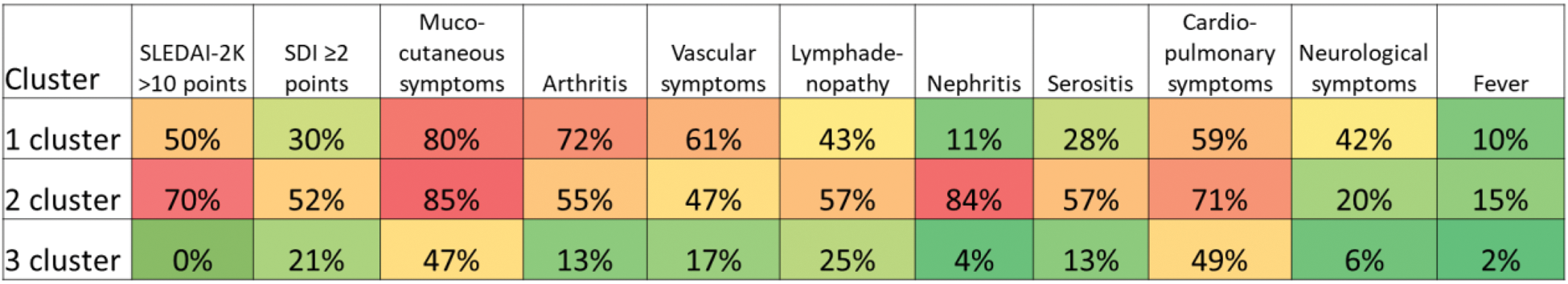
Results: Three distinct clinical phenotypes were identified (Figures 1 and 2). Cluster 1 (n=105, 37%) included patients with predominant neurological and vascular involvement, arthritis, and moderate-to-high SLE activity (median SLEDAI-2K score 10 [8-15] points). Cluster 2 (n=122, 44%) patients exhibited activity in renal, serosal, cardiorespiratory domains, with the highest baseline SLEDAI-2K (14 [10-18] points) and SDI (2 [1-2] points) scores. Cluster 3 (n=53, 19%) captured patients with limited-organ manifestations and low disease activity (SLEDAI-2K score 2 [0-4] points). Patients in Cluster 2 were the youngest at disease onset (26 [19-36] years, p=0.018). No gender differences were observed between the clusters. At the follow-up visit, nearly half of the patients (n=47; 43.5%) achieved a clinical response. Specifically, 6 patients (5.6%) achieved remission, 25 patients (23.1%) attained lupus low disease activity state, and 16 patients (14.8%) had a reduction in the SLEDAI-2K score by ≥4 points. Cluster 3 displayed a significantly higher proportion of responders at follow-up visit (68%), compared to Cluster 1 (32%) and Cluster 2 (46%) (p=0.022). Logistic regression analysis showed that Cluster 3 membership was a predictor of response to therapy (odds ratio [OR] 4.60, 95% confidence interval [CI] 1.48-14.30, p=0.008). Conversely, Cluster 1 membership was associated with a lower likelihood of achieving clinical response (OR 0.47, 95% CI 0.26-0.85, p=0.013). The odds of treatment response in Cluster 2 were higher (OR 1.82, 95% CI 0.77-4.33) compared to Cluster 1, though the statistical difference was not reached (p=0.175). The area under the receiver operating characteristic curve for the model was 0.64 (95% CI 0.54-0.74, p=0.028).
Conclusion: The cluster approach may enhance patient management by enabling early identification of clinical patterns. Our study delineates three distinct clinical phenotypes in SLE patients with different treatment response rates. A cluster with predominant nervous system and vascular involvement is associated with the lowest probability of treatment response. These findings support the need for further investigation into neuropsychiatric SLE and development of updated targeted therapeutic strategies.
Cluster analysis of patients with systemic lupus erythematosus revealing three clinical disease subsets.
Prevalence of clinical manifestations in clusters of systemic lupus erythematosus.
REFERENCES: [1] Franklyn K, et al. Definition and initial validation of a Lupus Low Disease Activity State (LLDAS). Ann Rheum Dis 2016;75:1615-1621.
[2] van Vollenhoven RF, et al. 2021 DORIS definition of remission in SLE: final recommendations from an international task force. Lupus Sci Med 2021;8:e000538.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (