

Background: Chronic pain is frequent in patients with idiopathic inflammatory myopathies (IIM), despite having remitted disease. Some IIM patients may fulfill the fibromyalgia (FM) diagnostic criteria, which may negatively influence the patients’ reported outcomes (PROs) and may lead to overtreatment and decreased quality of life. Thus, the risk factors to present chronic pain and FM in IIM patients is a priority research area. The pathogenesis of FM is unknown, nonetheless, previous studies have described certain clinical, immunological and metabolomic features associated to this disease. The prevalence, as well as the features associated with the diagnosis of FM in IIM have not been previously addressed.
Objectives: The aim of this study was to analyze the clinical, immunological and metabolomic features associated to the diagnosis of FM in patients with IIM.
Methods: We performed a cross-sectional study including IIM patients from the Myositis Translational Research Cohort Salvador Zubirán (MYOTReCSZ) who fulfilled the EULAR/ACR 2017 criteria for IIM and had complete clinical response/ remission for 6 months in a referral center in Mexico. We applied the PROMIS Pain Interference Short Form 8a and in those patients with a score above 11, the widespread pain index (WPI) and the symptom severity score (SSS) were used to diagnose them as having FM, according to EULAR/ACR 2010 criteria. We measured the myositis disease activity and damage according to the disease activity core set measures. Peripheral blood mononuclear subsets were assessed by multiparametric flow cytometry; serum cytokines were measured by a multiplex luminometry assay, and an untargeted metabolomic analysis of the serum was conducted using gas chromatography coupled to mass spectrometry. The features associated to the diagnosis of FM in IIM patients were assessed by logistic regression.
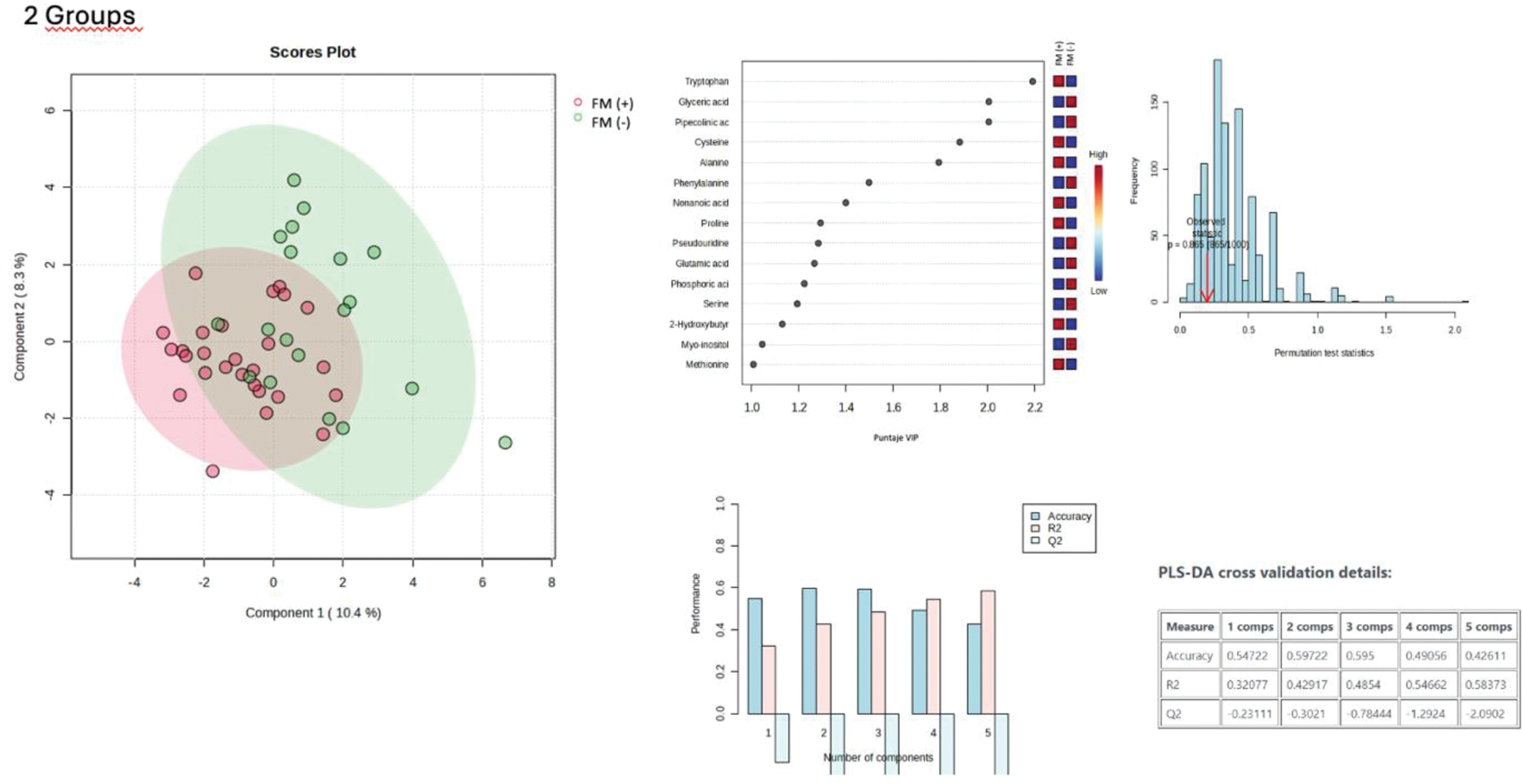
Results: We included 49 IIM patients, being dermatomyositis the most frequent IIM subtype. The prevalence of FM was 40.1% (20/49) and female sex was more frequent among patients with FM (95% vs 68.9%, p=0.016). Patients with IIM and FM displayed a higher patient reported global disease activity (PtGA) (3.5 vs 0.50, p=0.001), as well as muscular damage (1.5 vs. 1.0, p=0.023). Patients with FM more frequently received prednisone (55% vs 17.2%, p=0.005) and a at a higher dose. Immunologically, patients with IIM and FM had lower amount of T CD8+ cells (0.04 vs 0.13, p=0.045), B cells (58.4 vs. 152, p=0.052), and non-classical monocytes (16.4 vs 28.5, p=0.027), as well as higher levels of serum IL-6 (0.111 vs. 0.003, p=0.232). Regarding the metabolomic analysis, the tryptophan, glyceric acid, pipecolic acid, cysteine, and alanine were the metabolites with the highest discriminative score (VIP) for the presence of FM (Figure 1). The binary logistic regression (Table 1) showed that the PtGA (OR 14.4, 95% CI 2.44-360.79), the visual analog scale (VAS) of muscle damage (OR 7.80, 95% CI 1.77-143.86), the lung damage score (OR 2.94x10 -6 , 95% CI 8.40x10 15 -0.19) and MCP-1 levels (OR 2.17, 95% CI 1.07-8.17) were positively associated to FM, whilst the nonanoic acid levels were a protective factor (OR 0.01, 95% CI 1.47x10^-5-0.40, p=0.005).
Conclusion: Our data suggests a high prevalence of FM in patients with IIM in complete clinical response, which might be a source of chronic pain and decreased quality of life in this population. The main risks factors associated with FM in IIM are the PtGA, the VAS of muscle damage, lung damage score, as well as higher serum leves of pro-inflammatory cytokine MCP-1, whereas nonanoic acid levels were protective. This profile suggests that the presence of FM in IIM may be related to alterations in oxidative stress and the gut microbiome, as well as muscle damage. Our findings suggest that persistent pain in patients with IIM should raise suspicion for a diagnosis of FM. Further studies are required to assess if the diagnosis of FM is related to decreased quality of life, overtreatment and treatment-related comorbidities.
Binary logistic regression.
| Binary logistic regression. | ||||
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| Variable | OR (CI 95%) | P value | OR (CI 95%) | P value |
|
Patient global disease assessment
| 1,84 (1,33-2,84) | <0,0001 | 14,43 (2,44-360,79 | 0,003 |
|
Muscular damage global assessment
| 1,70 (1,33-2,84) | 0,016 | 7,80 (1,77-143,86) | 0,02 |
| Lung damage score (0-6 ) | 3,60 (0,95-18,21) | 0,058 | 2,94x10 -6 (8,40x10 15 -0,19) | 0,28 |
| MCP-1 (ng/mL ) | 1,07 (1,00-1,17) | 0,042 | 2,17 (1,07-8,17) | 0,15 |
| IL-8 (ng/mL ) | 1,29 (0,98-1,97) | 0,064 | 0,30 (0,03-1,35) | 0,59 |
| Nonanoic acid | 0,44 (0,15-1,12) | 0,089 | 0,01 (1,47x10 -5 -0,40) | 0,005 |
| Male sex (% ) | 0,11 (0,006-0,71) | 0,016 | ||
| Calcinosis (% ) | 2,8x10 -8 (NA-1,10) | 0,017 | ||
| Muscle damage score (0-5 ) | 1,63 (1,09-2,87) | 0,02 | ||
| PDN (% ) | 5,86 (1,66-23,41) | 0,005 | ||
| PDN dosis (mg ) | 1,27 (1,05-1,64) | 0,003 | ||
| CNI dosis (mg ) | 1.74 (1,07-6,79) | 0,015 | ||
| Percentage of B lymphocytes (% ) | 0,87 (0,77-0,97) | 0,015 | ||
| Absolute B lymphocytes(cells/µL ) | 0,99 (0,98-0,99) | 0,006 | ||
| IL-1β (ng/mL ) | 2,8x10 -13 (4,51 x10 -30 -0,36) | 0,022 | ||
| IL-6 (ng/mL ) | 3,6x10 6 (4,01-2,76 x10 21 ) | 0,009 | ||
| Tryptophan | 0,92 (0,84-0,99) | 0,035 | ||
* significant p value <0.05
Partial Least Squares Discriminant Analysis of the Metabolomic Profile in Patients with Idiopathic Inflammatory Myopathies, Comparing the Presence and Absence of Fibromyalgia.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (