

Background: Fatigue is one of the most common and disabling symptoms which might impair quality of life (QoL) in patients affected by chronic diseases [1]. Previous data showed that 35-82% of patient with rheumatic diseases (RDs) reported fatigue [2]. Fatigue is often associated with the perception of increased disease activity and has been identified as one of the factors implicated in the failure to achieve remission [3].
Objectives: We aimed to 1 ) assess fatigue in our cohort of RDs patients using validated questionnaires, to evaluate any differences in fatigue 2a ) compared with healthy subjects and 2b ) between various RDs subgroups and 3 ) the associations of fatigue with demographic, clinical features and potential confounders (sleep quality and sleepiness, anxiety and depression, quality of life, social functioning).
Methods: We conducted a cross sectional observational monocentric study including patients with rheumatoid arthritis (RA), systemic lupus erythematosus (SLE) and primary Sjögren syndrome (pSS) and healthy volunteers (HV) who agreed to participate to the study between August 2023 and July 2024. Patients with a primary diagnosis of major sleep disorder and fibromyalgia were excluded. Fatigue was rated on a visual analogue scale (fVAS: 0-100 mm; with higher scores indicating greater fatigue) and through FACIT-Fatigue (range score: 52-0; with lower scores indicating greater fatigue) and modified Mental Fatigue Scale (m-MFS). Additionally, all patients completed questionnaires investigating sleep quality (sqVAS and Medical Outcomes Study-Sleep Scale, MOS-SS), daily sleepiness (Epworth Sleepiness Scale, ESS), anxiety (Generalized Anxiety Disorder 2-item, GAD-2), depression (Patient Health Questionnaire-2, PHQ-2), QoL (EuroQoL 5 Dimensions 5 Levels, EQ-5D-5L) and social functioning (Social Functioning Questionnaires, SFQ).
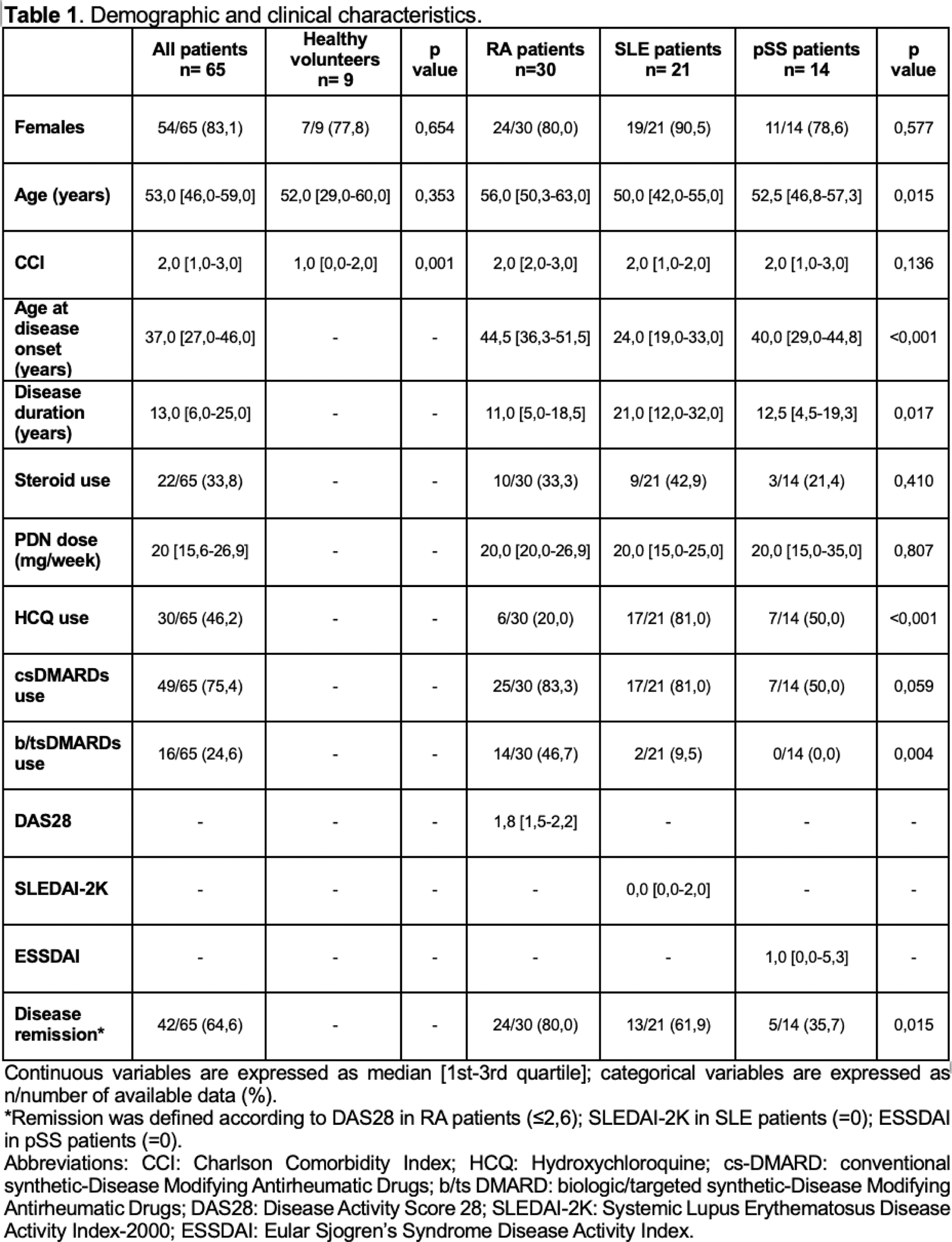
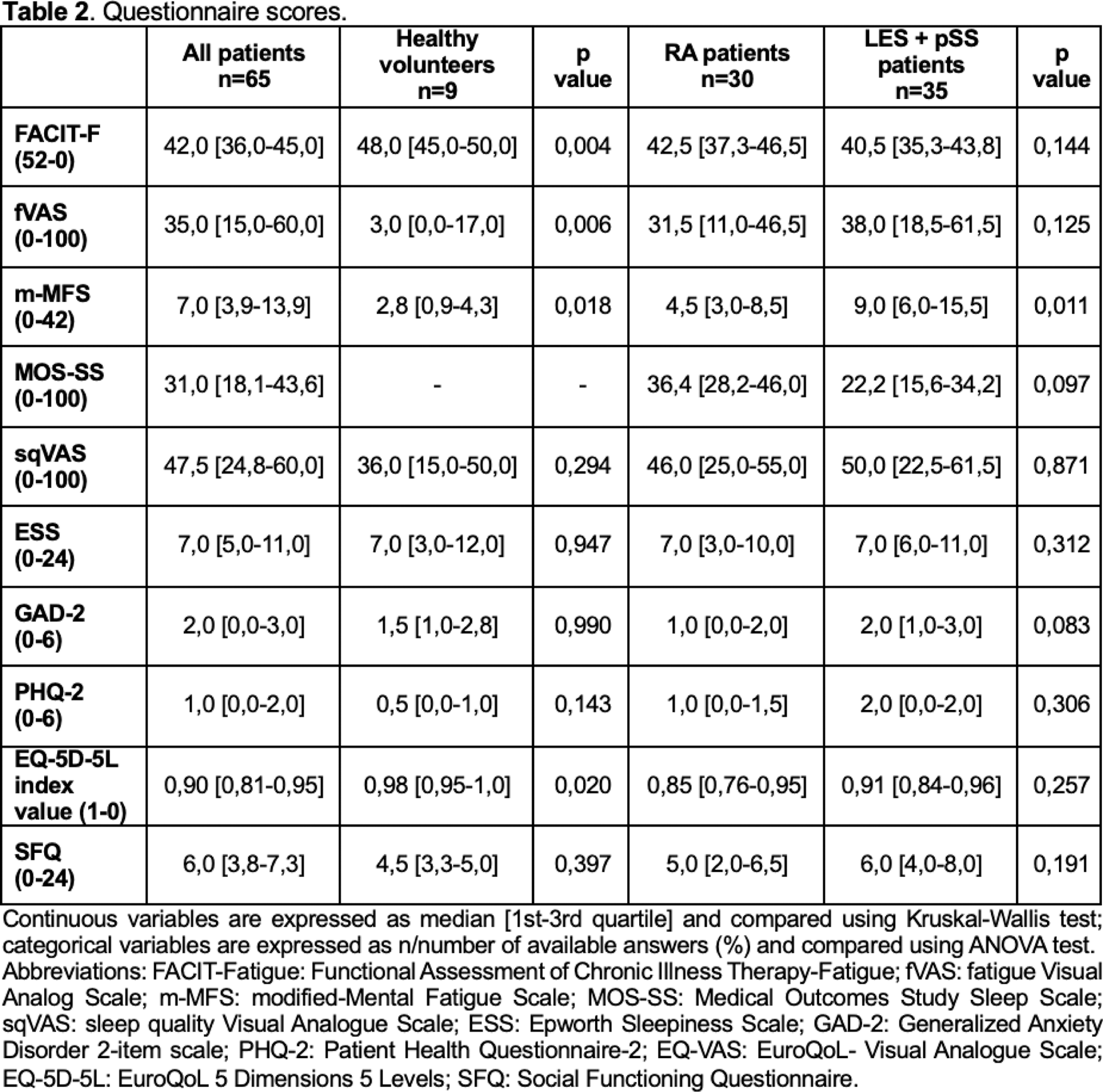
Results: We enrolled 65 patients (30 RA, 21 SLE, 14 pSS) and 9 HV (Table 1). 1 ) In the patient cohort the median fVAS, FACIT-Fatigue and m-MFS were 35,0 [15,0-60,0], 42,0 [36,0-45,0] and 7,0 [3,9-13,9] respectively. A good construct validity was observed correlating fVAS with FACIT-Fatigue and m-MFS (rs:-0.81, p<0.001 and rs:0.42, p:0.002). 2a ) Comparing the questionnaire scores RDs patients reported more fatigue, both physical and mental, and worst QoL and global health status (Table 2). 2b ) No differences between the different RDs subgroups regarding the questionnaires scores were observed except for m-MFS, showing a higher mental fatigue in patients with systemic connective tissue disease than RA patients (Table 2). 3 ) Female patients reported higher fVAS scores (meaning greater fatigue) as compared to males (39.0 [20.0-60.0] vs 14.0 [0.0-35.0], p:0.0125), while no significant correlations were found between fVAS scores and age, disease duration and Charlson Comorbidity Index. Among RA patients, DAS28 correlated positively with fVAS scores (rs:0.55, p:0.002) meaning that as disease activity increases, fatigue worsens; in SLE and pSS subgroups no correlations with disease activity were found. Finally, fVAS correlated positively with sqVAS (rs:0.36, p:0.004), ESS (rs:0,28, p:0.022), MOS-SS (rs:0.38, p:0.050), GAD-2 (rs:0.45, p<0.001), PHQ-2 (rs:0,31, p:0.028), SFQ (rs:0.41, p:0.003) and negatively with EQ-5D-5L index value (rs:-0.61, p:0.003). This implies that as fatigue worsens, so do sleep quality, anxiety and depressive symptoms, social functioning, quality of life and global health status.
Conclusion: In our cohort, the RDs patients reported worse fatigue and quality of life than healthy subjects. A greater fatigue appears associated with female sex as well as with sleep disturbances, anxiety symptoms, depression, poorer social functioning and lower QoL, without differences according to the RD diagnosis or disease activity indices. Future perspectives include the implementation of the results with the questionnaire scores obtained during subsequent follow-up visits to evaluate the data consistency. Indeed, to manage effectively fatigue, we need tools that can measure these symptoms accurately and reliably.
REFERENCES: [1] L Chen et al. Annu Int Conf IEEE Eng Med Biol Soc. 2022.
[2] Overman CL et al. The prevalence of severe fatigue in rheumatic diseases: an international study. Clin Rheumatol 2016.
[3] Pollard LC et al. Fatigue in rheumatoid arthritis reflects pain, not disease activity. Rheumatology 2006.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (