

Background: The Bronx, NY, home to approximately 1.3 million people, has one of the highest poverty rates (27.9%) in the United States [1]. According to the US Census, 6.5% of people are unemployed and 7.3% lack health insurance [1]. The NYC borough is predominantly composed of historically underserved groups, including Hispanic (55%) and Black (33.7%) communities. Montefiore Medical Center (MMC) is one of the leading medical institutions in the Bronx, servicing around 32% of the population. Socioeconomic factors are known to influence morbidity and mortality in systemic lupus erythematosus (SLE) [2]. Identifying and addressing socioeconomic determinants, on a community-specific level, has the potential to directly improve patients’ clinical outcomes and quality of life.
Objectives: This study aims to identify specific socioeconomic factors that predict adverse outcomes in the SLE population of the Bronx, to inform targeted interventions aimed at improving patient care.
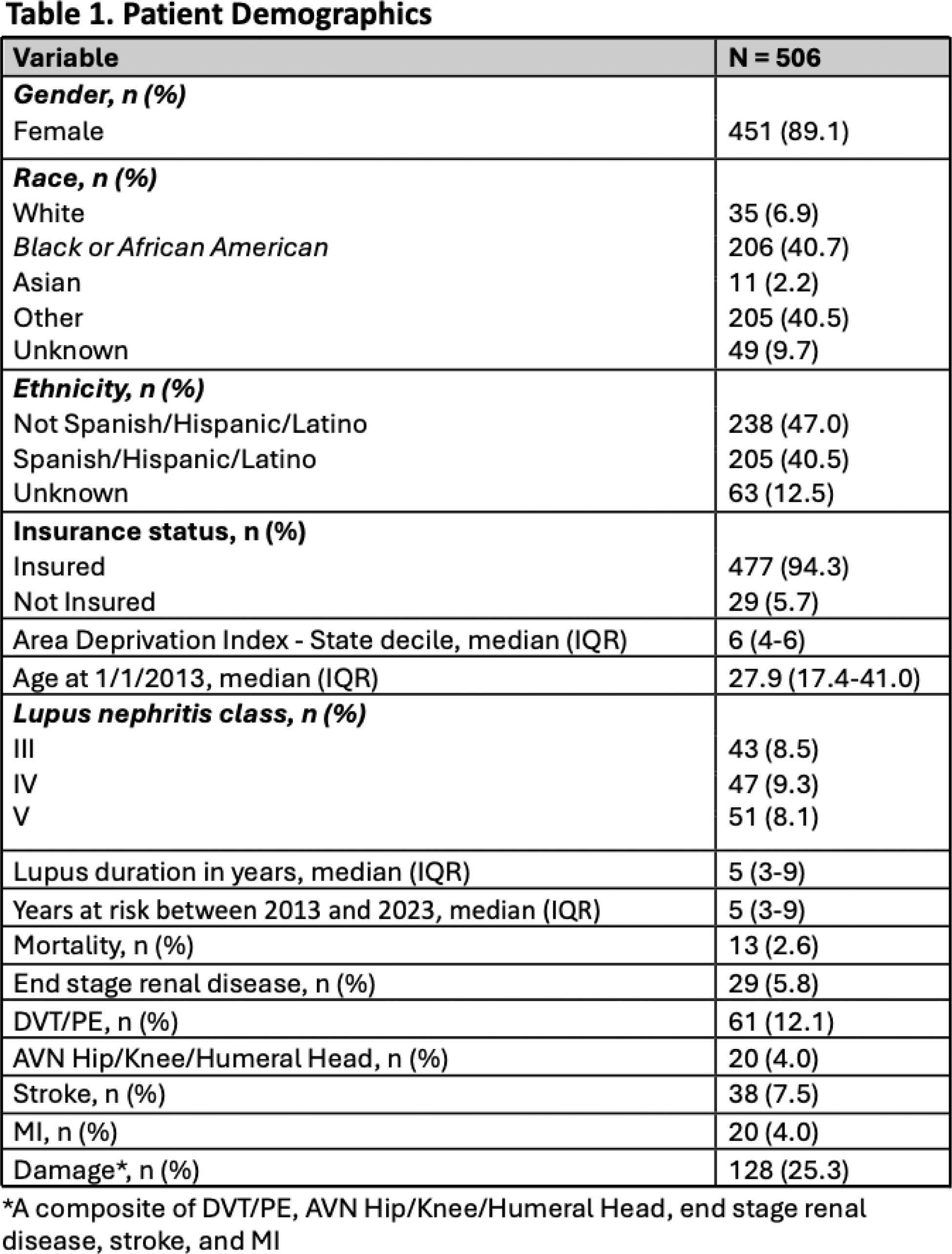
Methods: We conducted a retrospective cohort study of SLE patients who received care at MMC outpatient clinics between 2013-2023. Data collected included demographic information, factors related to socioeconomic status (such as area deprivation index (ADI) and health insurance status), in addition to disease-related damage measures, as detailed in Table 1. Spearman’s correlations were calculated between continuous variables. Poisson regression models for the counts with the years at risk as offset were fit. Logistic regression models for the binary outcomes with adjustment for the years at risk and other covariates were used to obtain p-values. All tests were two-sided, and p-value <0.05 was considered statistically significant. SAS software version 9.4 (Cary, NC, USA) was used for statistical analyses.
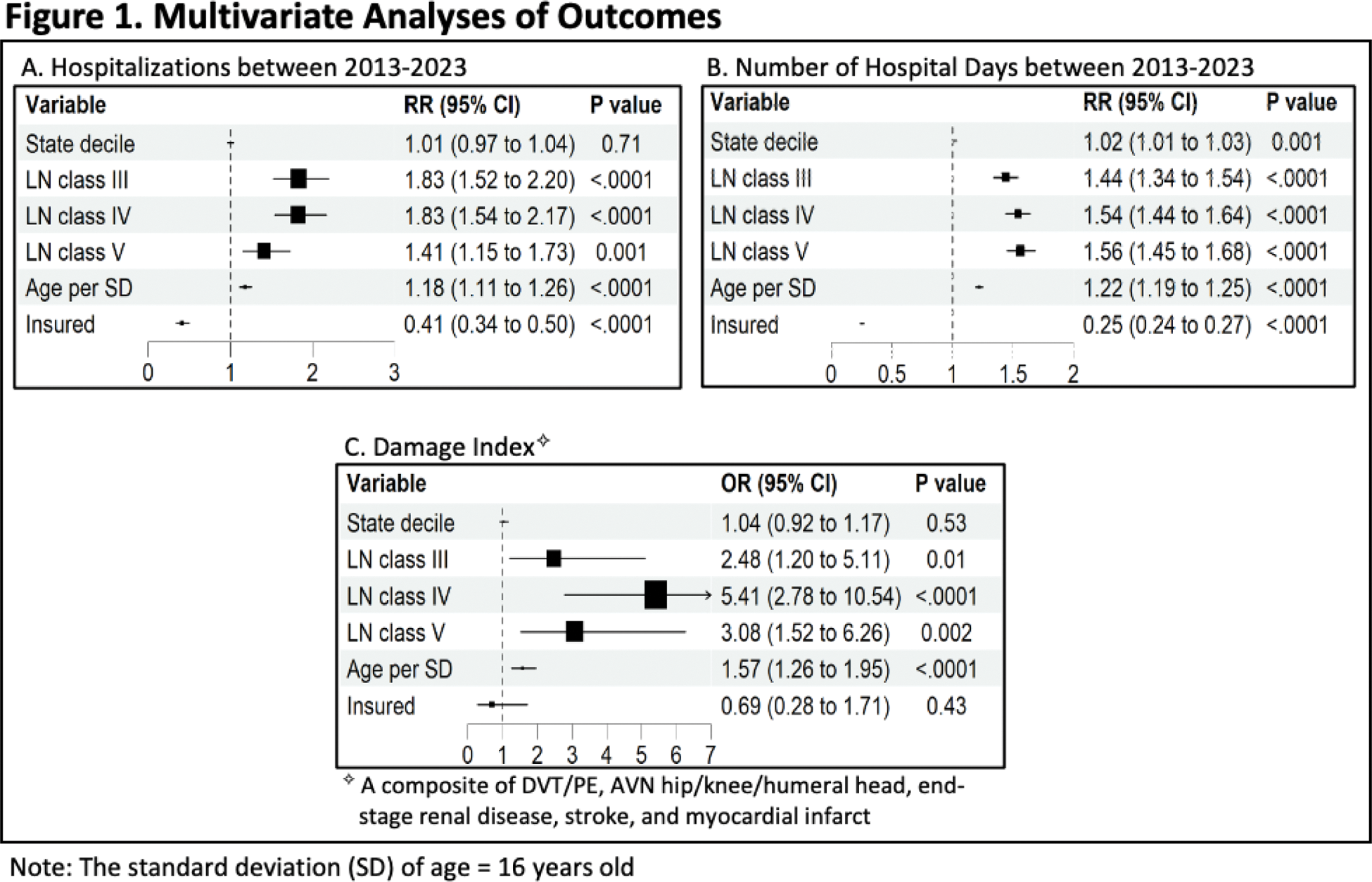
Results: A total of 506 SLE patients were included in the study, with Black (40.7%) and Hispanic (40.2%) patients comprising the largest racial/ethnic groups (Table 1). Of these, 477 patients (94%) had some form of health insurance, and these patients had significantly fewer hospitalizations (RR 0.41 [95% CI 0.34-0.50] p<0.0001; Figure 1A), with significantly less total hospital days than uninsured patients (median (IQR) of 5 (0-18) days vs. 13 (0-34) days, p<0.0001) (Figure 1). ADI, on the other hand, was not associated with hospitalizations, or damage in this patient population. As expected, lupus nephritis (LN), particularly class IV, was the primary driver of hospitalizations and damage (Figure 1). More specifically, patients with LN class IV were 17-times more likely to develop end-stage renal disease (ESRD) (OR 16.95 [95%CI 6.42-44.77], p<0.0001), and 4-times more likely to develop venous thromboembolism (OR 4.11 [95% CI 1.80-9.38], p=0.001), compared with non-LN patients. Age and disease duration also influenced hospitalizations and damage, but appear to be only clinically significant in the context of myocardial infarction (MI), as patients who had MI were significantly older than those who did not (median (IQR) age of 52 (36.3-60.5) vs. 27 (16.9-39.4); p <0.0001).
Conclusion: This study highlights the critical role of health insurance in minimizing hospitalizations in SLE patients living in the Bronx. Although all patients in our cohort, by definition, had access to rheumatology clinic, uninsured individuals likely face other barriers that limit their utilization of outpatient disease management resources. Other socioeconomic factors, such as the area deprivation index, did not appear to significantly influence hospitalization or damage in our cohort. As expected, the presence of LN, particularly class IV, was the key driver of severe outcomes, including ESRD and thrombosis. These findings emphasize that targeted interventions for high-risk, uninsured individuals, particularly those with more severe disease such as LN, is crucial for improving patient outcomes in this underserved population.
REFERENCES: [1] U.S. Census Bureau. (2023).
American Community Survey 5-Year Estimates, 2019-2023
. U.S. Department of Commerce, Economics and Statistics Administration. Retrieved from
[2] Alarcón, G. S., Calvo-Alén, J., McGwin, G., Jr, Uribe, A. G., Toloza, S. M., Roseman, J. M., Fernández, M., Fessler, B. J., Vilá, L. M., Ahn, C., Tan, F. K., Reveille, J. D., & LUMINA Study Group (2006). Systemic lupus erythematosus in a multiethnic cohort: LUMINA XXXV. Predictive factors of high disease activity over time.
Annals of the rheumatic diseases
,
65
(9), 1168–1174.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (