

Background: Organ calcification has been reported across various systemic autoimmune diseases, often as a significant part of the clinical presentation, such as in systemic sclerosis or dermatomyositis. In systemic lupus erythematosus (SLE), calcifications are primarily described in coronary arteries (coronary artery calcification, CAC), cardiac valves, and kidneys, with a notable prevalence of CAC in younger patients due to premature atherosclerosis. Other types of organ calcification, including calcifications in the bronchi, pericardium, thymus, and spleen, have mostly been documented in case studies. These findings are often incidental, typically identified by CT scans, and considered subclinical, although their clinical correlations and potential impact on disease outcomes remain unclear.
Objectives: This study aims to provide systematic, controlled data on the prevalence of organ calcifications in patients with SLE by thoracic CT scans, and its correlation with key lupus characteristics, cardiovascular disease risk factors, and CAC severity.
Methods: This study is a clinical case-control cross-sectional study including 112 SLE patients matched by age- and sex to 156 population controls. The SLE patients originate from the PLUSHEART cohort [1] and the control from the Copenhagen General Population Study. CAC and organ calcification were assessed by thoracic non-contrast CT scans by an ECG-gated cardiac protocol on a 320-multidetector scanner. Visible organ calcifications were evaluated for the bronchi, spleen, pericardium, and thymus. CAC was quantified with the Agatston method. The patients and control were clinically evaluated for traditional cardiovascular risk factors included in the Framingham Risk Score; i.e. age, sex, smoking, total cholesterol, HDL cholesterol, treated or untreated systolic blood pressure, and diabetes. The SLE patients were evaluated for key lupus factors, i.e., lupus nephritis (LN), anti-phospholipid antibodies (APL), and, as a surrogate marker for overall disease burden, accumulated organ damage by the SLE Damage Index (SDI).
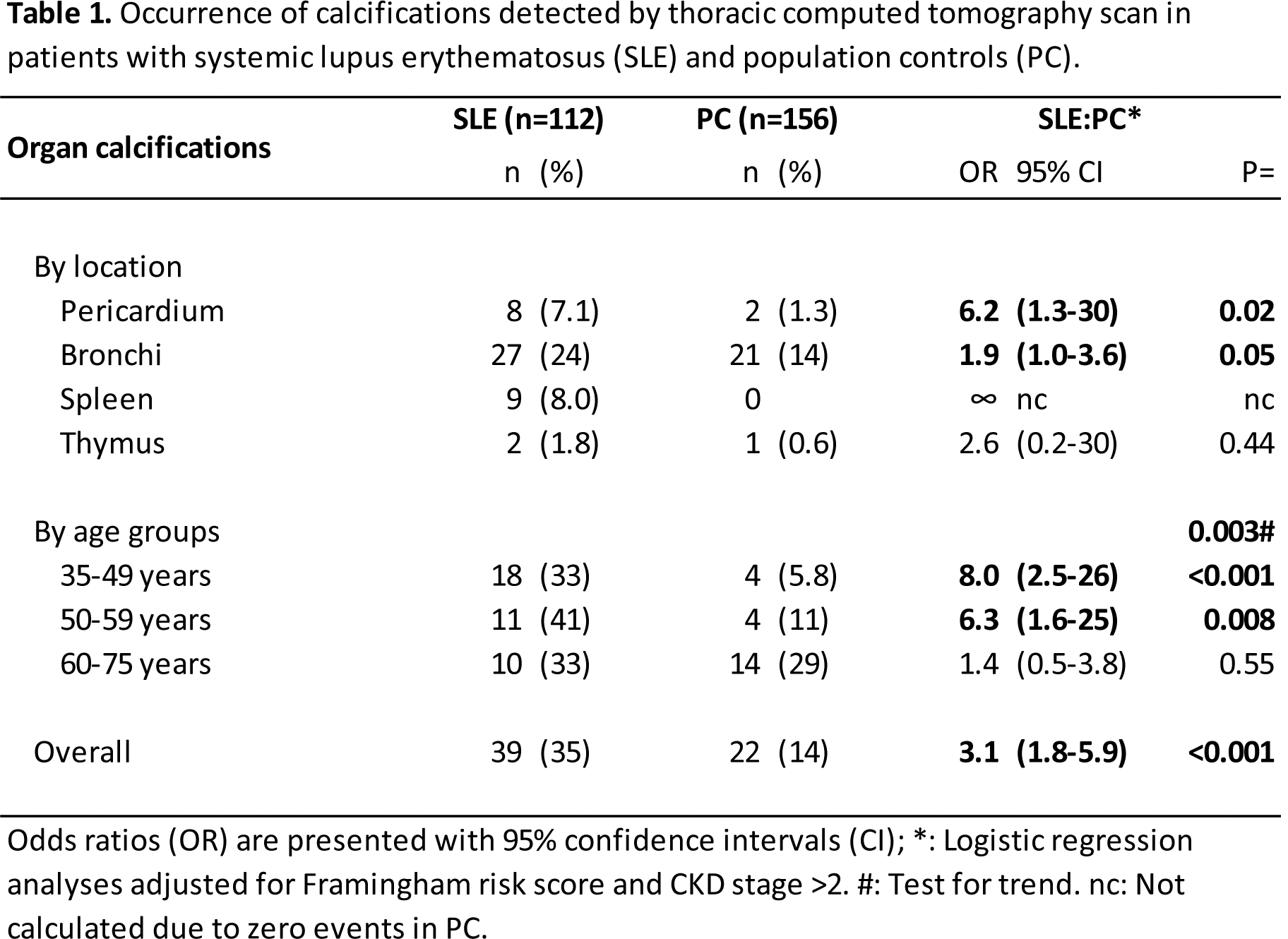
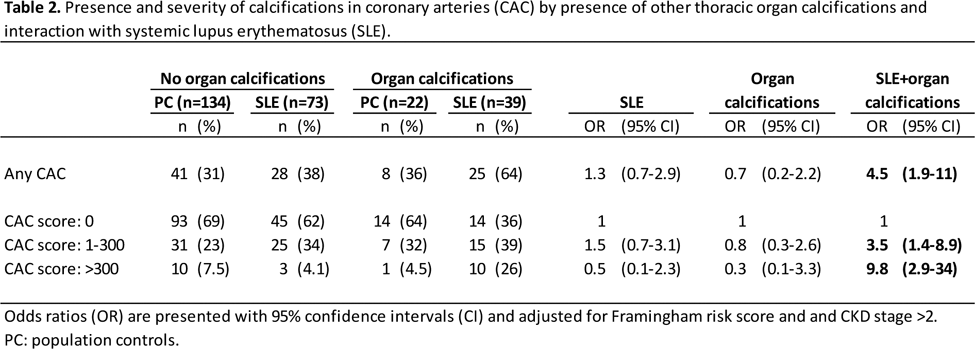
Results: Basic characteristics: SLE patients and controls were equal regarding biological sex (SLE: 90% female), age (52.1 ± 10.1, years ± SD), and ancestry (96% Scandinavian). Lupus characteristics: The SLE patients had a median disease duration of 16.5 years (range 1.7-41), an SDI of 1 (0-9), 63% presented with APL, and 21% with LN. Cardiovascular risk factors: Similar numbers of SLE patients and controls had hypertension: 55% (only SLE figures shown), diabetes: 3.6%, obesity (BMI≥30): 13%, and HDL cholesterol: 1.6±0.5 mmol/L. Compared to controls, the SLE patients had a lower total cholesterol (5.0 ±1.0 vs 5.5±1.1 mmol/L) but were more likely to use statins (16% vs 5.2%), have a chronic kidney disease (CKD) stage >2 (13% vs 4.5%), and smoke (current 19% vs 12%). The Framingham score median was 2.7% in SLE and equal between groups. Prevalence of calcifications: The occurrence of organ calcification is illustrated in Table 1. The overall prevalence of OC in SLE and control was 35% and 14%, respectively. In SLE, the organ calcifications were located in bronchi (24%), spleen (8%), pericardium (7%) and thymus (1.8%) and the prevalence was higher in SLE at all loci except the thymus. Further, the odds of having any organ calcification were increased in patients aged < 60 years with ORs of 6.3 (age: 50-59) and 8.0 (age: 35-49). CAC was prevalent in 47% of SLE patients and in 31% of controls (OR, 95%CI: 2.0, 1.2-3.2). Organ calcification and lupus characteristics: In a multivariable logistic regression analysis including CKD, LN, APL, and SDI only SDI was associated with organ calcification, beta=0.26 and p=0.03. Organ calcification and cardiovascular disease risk : In SLE, organ calcification was not associated with any of the individual Framingham Risk Score items (data not shown), whereas in controls organ calcification was associated with age (Spearmans rho=0.25, p=0.001), total cholesterol (0.16, p=0.043), and receiving antihypertensive (0.18, p=0.024). Organ calcification and CAC : Of the individuals without organ calcification, the SLE patients and controls presented with similar prevalence of CAC, 31% and 38% (Table 2). Of the individuals with organ calcification, the SLE patients presented with higher prevalence of CAC, 64%, compared to controls, 36%. With adjustment for Framingham items, the odds of having CAC were 4.5 higher (95%CI 1.2-25) when having both SLE and organ calcification. For CAC Agatston scores >300 this association was even stronger, OR 9.8 (2.9- 34).
Conclusion: The prevalence of organ calcification was significantly higher in SLE patients compared to controls for the bronchi, spleen, and pericardium, and especially pronounced in patients younger than 60 years. In SLE patients, organ calcification was not correlated with cardiovascular risk factors, but correlated with overall damage, by the SDI. Finally, the presence of organ calcification correlated with the excess risk of CAC and CAC severity in SLE patients.
REFERENCES: [1] PLUSHEART-cohort: Hermansen ML, et al. 2018, doi: 10.1093/rheumatology/key201.
Acknowledgements: NIL.
Disclosure of Interests: Amanda Hempel Zinglersen: None declared, Line Kjær Winberg: None declared, Klaus Fuglsang Kofoed: None declared, Andreas Fuchs: None declared, Søren Jacobsen Astra Zeneca, Lundbeck.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (