

Background: Outcomes of randomised clinical trials aimed at delaying or preventing the onset of rheumatoid arthritis (RA) in individuals at risk have been published with variable results. In the APIPPRA study, we reported that 52 weeks of treatment with abatacept reduced rates of progression to RA, effects which were sustained beyond the treatment period [1]. We also documented reductions in the symptom burden, as well as sub-clinical joint inflammation defined by ultrasonography. The long-term effects of RA interception, however, are not known.
Objectives: To capture long term outcomes of APIPPRA study participants in the ALTO follow up study to establish the extent to which one year of abatacept treatment prevents or delays the onset of RA in subsequent years.
Methods: APIPPRA was a phase IIB randomised, double blind, placebo-controlled trial recruiting 213 ACPA + RF + or ACPA hi RF - individuals with inflammatory arthralgia without clinical synovitis. Consenting participants were randomised to receive 52 weekly subcutaneous injections of placebo (n=103) or 125mg abatacept (n=110) and followed up for a further 52 weeks after stopping treatment [1]. All study participants deemed eligible and randomised to the APIPPRA study who had received study drug and completed at least one study visit were invited to participate in the ALTO follow up study. The primary endpoint was the time to development of either clinical synovitis in ≥ 3 joints, or RA according to ACR/EULAR 2010 criteria, whichever was met first, where joint involvement required swelling. To capture outcomes during the period between the end of APIPPRA and the beginning of ALTO, as well as during longer term follow up, time to first treatment with disease modifying anti-rheumatic drugs, excluding corticosteroids, was included as a primary endpoint if met first. Primary endpoints were also evaluated after stratifying for serum autoantibodies defined at the APIPPRA baseline visit. Secondary endpoints included multiple disease activity assessments. To assess the safety of interception, severe adverse events (SAE) were recorded, as were events of special interest focusing on cardiovascular, cancer and infectious episodes.
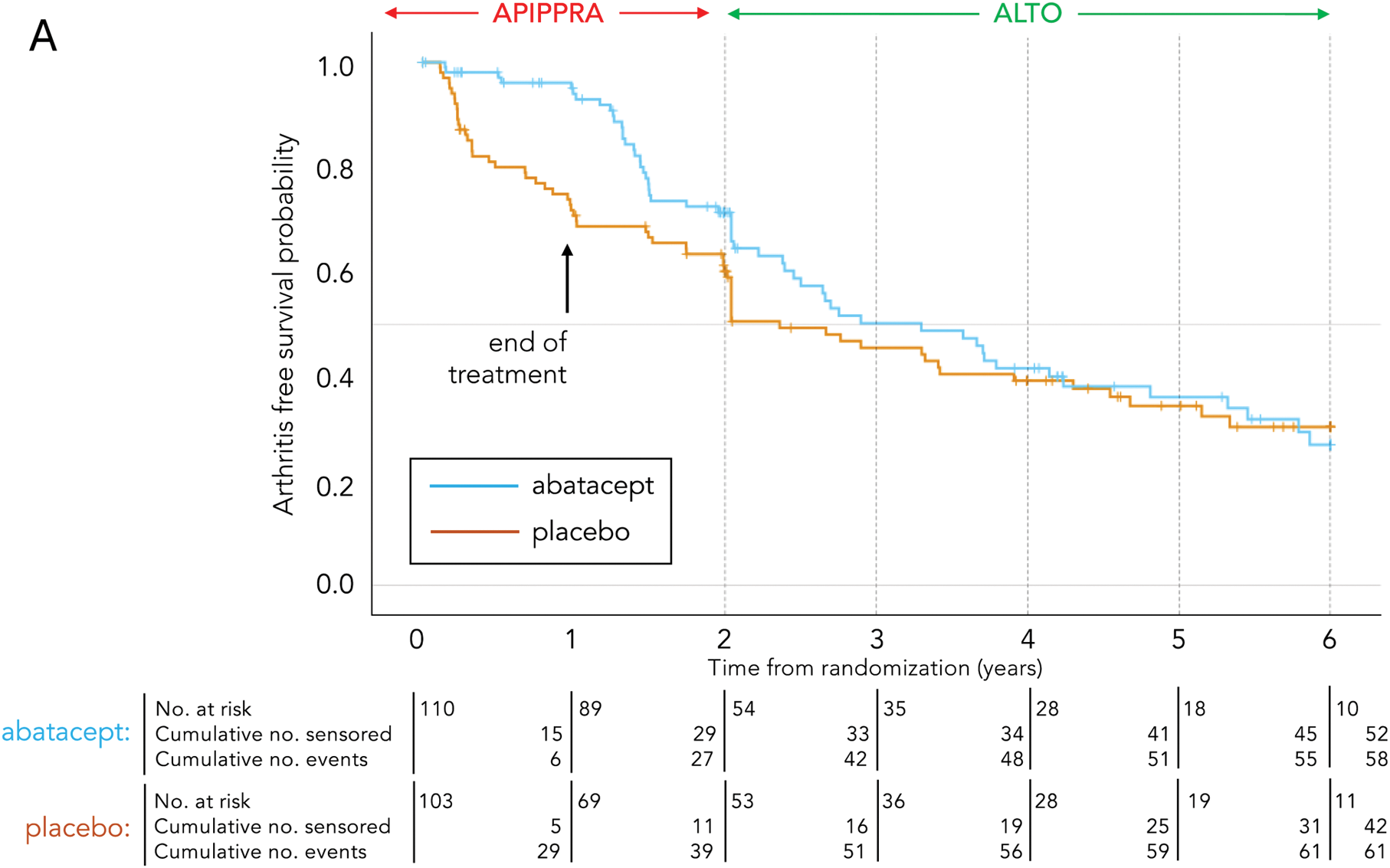
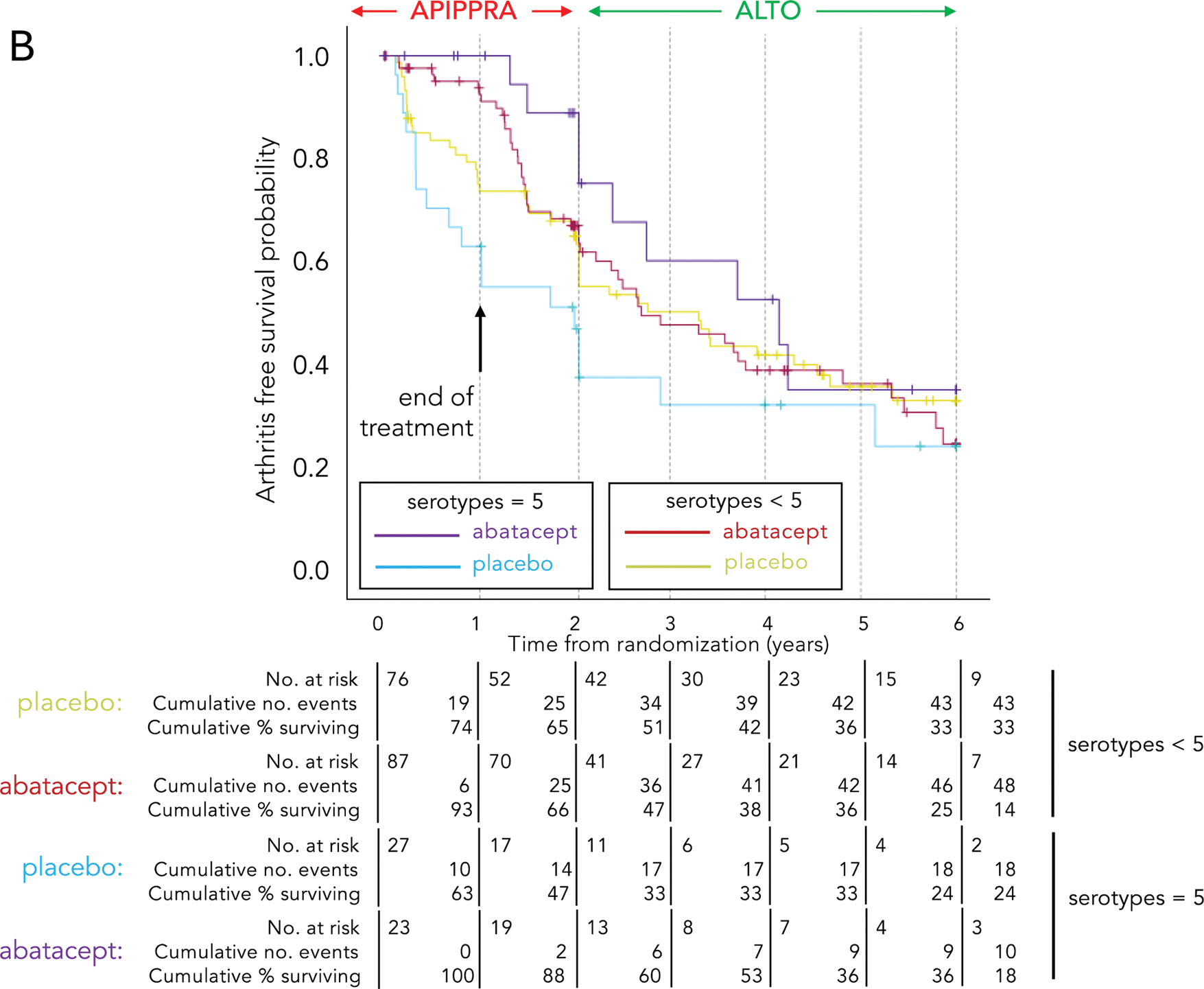
Results: Between 26 th April 2021 and 31 st January 2023, out of the 213 APIPPRA participants, 143 enrolled in ALTO, of whom 71 had been randomised to abatacept and 72 to placebo during the APIPPRA study. Mean age was 48 years, 78% were female and 60% were current or previous smokers, which is similar to the APIPPRA baseline demographic. Median follow up time from randomization to the APIPPRA study was 66 months (Q25-Q75: 54 – 78). At the end of follow up, there were a total of 119 primary outcome events. By the end of the first year after randomisation, the cumulative Kaplan-Meier proportion with arthritis was 29% in the placebo arm and 6% in the abatacept arm (difference of 23%). At the end of 2 years these were 40% and 30%, respectively (difference of 10%); at the end of the third and fourth years, the differences were 4% and 2% (Figure 1A). Differences between arms in restricted mean arthritis-free survival time (defined as areas under the two survival curves) up to 2 years were 3.3 months (95% CI 1.4 – 5.3; p=0.001), up to 3 years 4.4 months (95% CI 1.1 – 7.8; p=0.008), and up to 4 years 5.0 months (95% CI 0.38 – 9.8; p=0.039), while differences were no longer sustained at 5 years of follow up (5.2 months, 95% CI -1.0 – 11.4; p=0.102). Time to event analysis of primary outcomes stratified by baseline IgG ACPA levels revealed that after 2 years of follow up the cumulative proportion with arthritis was 49% in the placebo arm compared to 27% in the abatacept arm in those with levels ≥ 340 IU/ml; by 4 years it was 67% and 59% for placebo and abatacept, respectively. For those with an extended serotype characterised by IgG ACPA, IgA ACPA, anti-carbamylated protein antibodies, anti-acetylated protein antibodies and RF (designated “5 serotypes”), the cumulative proportion with arthritis was 53% for placebo and 12% for abatacept after 2 years, and 67% and 47% by the end of 4 years of follow up. For those carrying the extended serotype, differences between the placebo and abatacept arm were sustained to 6 years (Figure 1B), while the event rates for those individuals with < 5 serotypes were similar by approximately 18 months. There were 5 SAEs in those randomised to the abatacept arm and one in the placebo arm; none were deemed related to study drug. There were 7 events of special interest in the placebo arm and 5 in the abatacept arm, including a nail fungal infection, deemed possibly related to abatacept.
Kaplan-Meier arthritis-free survival curves by study arm for the combined APIPPRA and ALTO study periods for the intention to treat population (A) and stratified by baseline autoantibody status (B).
Conclusion: Interception with abatacept for one year delays progression to RA for up to 3 years after stopping drug. Those at highest risk of progression carry high levels of serum IgG ACPA and a mature autoantibody response, appear particularly sensitive to T cell co-stimulation modulation, and are those in whom a higher proportion achieve this delay. RA interception with abatacept appears to be well tolerated, with no new safety signals emerging during the follow up period.
REFERENCES: [1] Cope AP, Jasenecova M, Vasconcelos JC, Filer A, Raza K, Qureshi S, D’Agostino MA, McInnes IB, Isaacs JD, Pratt AG, Fisher BA, Buckley CD, Emery P, Ho P, Buch MH, Ciurtin C, van Schaardenburg D, Huizinga TJW, Toes R, Georgiou E, Kelly J, Murphy C, Prevost AT, on behalf of the APIPPRA Study Investigators. Abatacept in individuals at high risk of rheumatoid arthritis: a randomised, multi-centre, placebo-controlled phase 2B interception trial. Lancet 2024;403:838-849.
Acknowledgements: The APIPPRA trial and ALTO follow up study are Investigator Sponsored Research (ISR) studies funded by Bristol Myers Squibb, and jointly sponsored by Guy’s and St Thomas’ NHS Foundation NHS Trust and King’s College London in the UK and Leiden University Medical Center in the Netherlands. Bristol Myers Squibb have played no role in data acquisition or analysis.
Disclosure of Interests: Andrew Cope Bristol-Myers Squibb, Galapagos, Janssen, Bristol-Myers Squibb, Janssen, UCB, Abbvie, Nucleome Therapeutics, Galvani, Lilly, Bristol-Myers Squibb, UCB, Janssen, Marianna Jasenecova Bristol Myers Squibb, Joana Vasconcelos Bristol Myers Squibb, Andrew Filer: None declared, Karim Raza: None declared, Sumera Qureshi Bristol Myers Squibb, Maria Antonietta D’Agostino Bristol Myers Squibb, Iain B. McInnes Bristol Myers Squibb, Bristol Myers Squibb, Stefan Siebert: None declared, John Isaacs: None declared, Arthur Pratt: None declared, Benjamin A. Fisher Bristol Myers Squibb, Christopher D Buckley: None declared, Paul Emery Bristol Myers Squibb, Bristol Myers Squibb, Bristol Myers Squibb, Kulveer Mankia Bristol Myers Squibb, Pauline Ho: None declared, Maya Buch: None declared, Coziana Ciurtin: None declared, D. van Schaardenburg: None declared, Tom Huizinga Bristol Myers Squibb, Bristol Myers Squibb, Rene E.M. Toes Bristol Myers Squibb, Caroline Murphy Bristol Myers Squibb, A. Toby Prevost Bristol Myers Squibb.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (