

Background: People with rheumatoid arthritis (RA) or axial spondyloarthritis (axSpA) frequently face restrictions in work participation [1, 2]. Whereas support for people with rheumatic and musculoskeletal diseases (RMDs) to participate in healthy and sustainable paid work is recommended [3], research on the effectiveness of vocational interventions is limited.
Objectives: To compare the effectiveness on work-related outcomes and cost-utility of a multimodal, physiotherapist (PT)-led, vocational intervention with usual care in adults with RA or axSpA and a reduced work ability.
Methods: (Self-)employed people with RA or axSpA and a reduced self-reported work ability (Work Ability Index – Single Item scale (WAS) ≤7/10) and/or RA/axSpA related sick leave (≤6 months) were randomized to a 12-month PT-led vocational intervention or usual care. The intervention consisted of 10-21 personalized PT-led sessions including mandatory modalities (i.e., work-oriented assessment, patient education, exercise therapy, referral-roadmap of work-related professionals) and optional modalities (i.e., workplace examination, self-management course). Assessments were performed at baseline, and at three, six and twelve months follow-up. Primary outcome was the change in WAS (Numeric Rating Scale (NRS) 0-10) at 12 months. Secondary outcomes included the following work-related assessments: Work Productivity and Activity Impairment questionnaire (WPAI), job satisfaction (NRS 0-10) and self-efficacy at work (NRS 1-5). Analyses were done using linear mixed models taking into account all timepoints. For the economic analysis, participants and PTs recorded measurements of medical and non-medical (including productivity) costs. Quality-adjusted life years (QALYs) were estimated using the EQ-5D-5L and EQ-VAS. Costs and QALY differences were analyzed according to the intention-to-treat principle using cost-effectiveness acceptability curves.
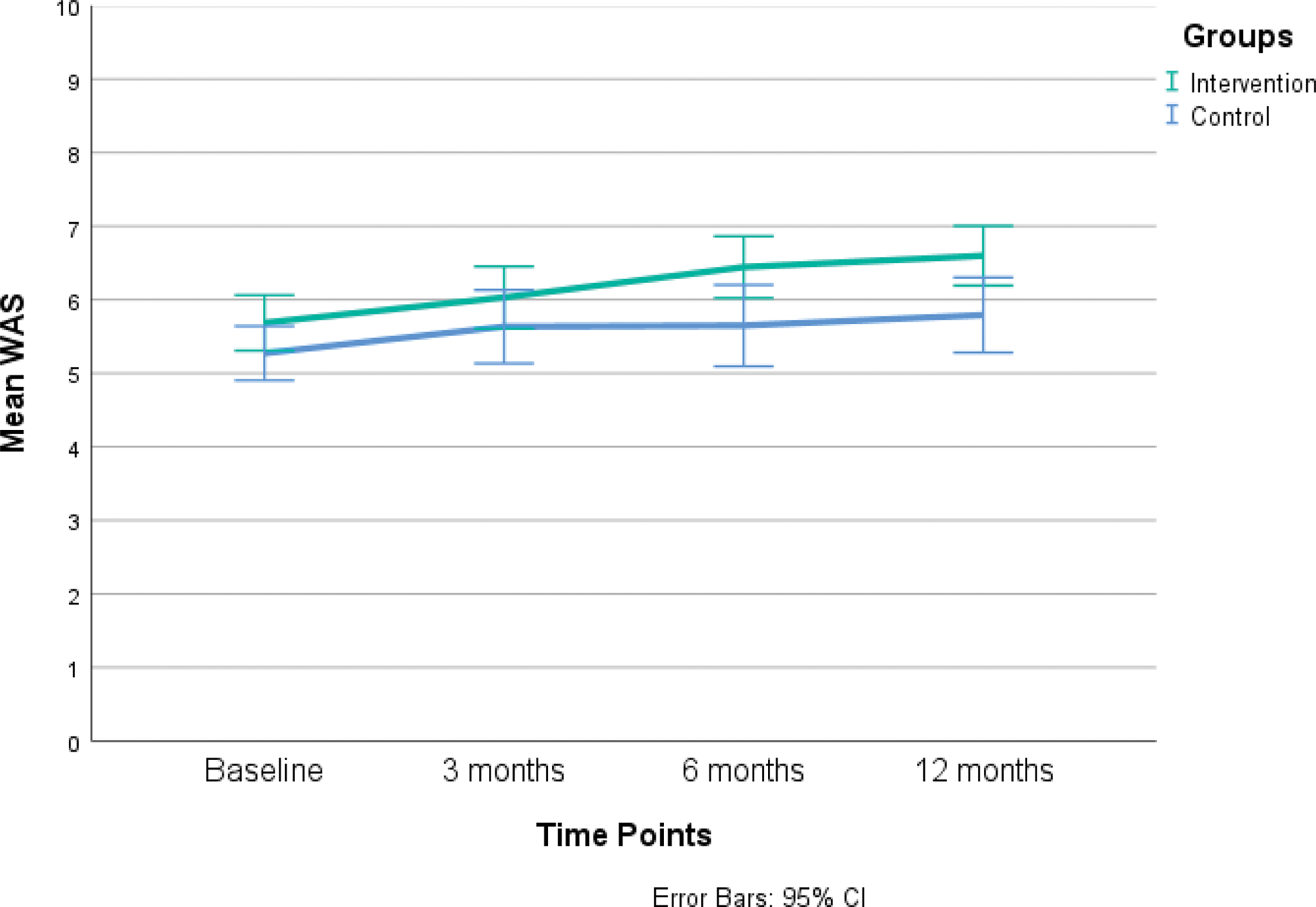
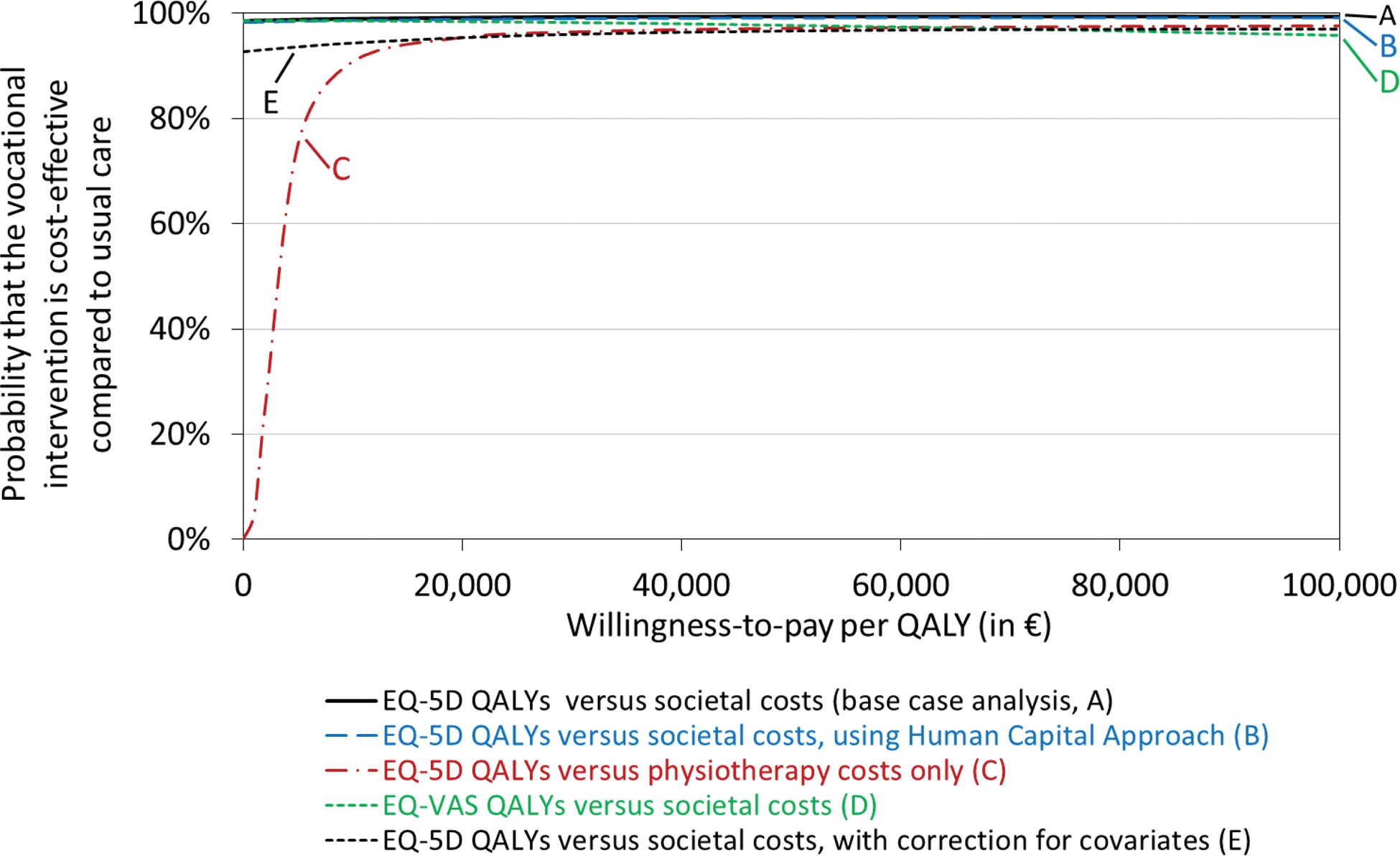
Results: In total, 140 people (n=80 RA; n=60 axSpA; 79% female) were randomized to the intervention (n=70) or control group (n=70). The 12 months of follow-up were completed by 96% of both the intervention (n=67) and control group (n=67) At 12 months, no significant difference between the groups was seen for the WAS (estimated mean difference (MD) 0.40, 95% CI (confidence interval) -0.22, 1.01) (Figure 1). Likewise, the secondary work outcomes did not show any difference between the two groups, except for a statistically greater improvement of job satisfaction in the control group at 12 months (MD -0.72, 95% CI -1.30, -0.13). The QALYs were non-significantly in favor of the intervention group by 0.05 according to the EQ-5D-5L (95% CI 0.00, 0.10) and by 0.01 according to the EQ-VAS (95% CI -0.03, 0.05). The mean direct costs of the intervention were €395 per participant, with an average of 9.5 sessions utilized by 90% of the participants. In the usual care group, on average 5.6 PT sessions were used by 29% of the participants. The total societal costs significantly favoured the intervention group after 12 months, showing a difference of €-4324 (95% CI €-8169, €-479). At a willingness-to-pay threshold of €20,000 per QALY, the intervention had a 95% likelihood of being the cost-effective strategy, which result remained after adjustment for covariates (Figure 2).
Conclusion: Although not with respect to work-related outcomes, the PT-led, vocational intervention in people with RA or axSpA and a reduced work ability tended to be superior with respect to QALYs. Moreover, total societal costs were lower in the intervention group, warranting the conclusion that the intervention is likely to be cost-effective compared to usual care. Further exploration of the discrepancy between work outcomes and QALYs and possible explanations for the higher costs in the usual care group is needed.
REFERENCES: [1] Kirkeskov, L. and K. Bray, Employment of patients with rheumatoid arthritis - a systematic review and meta-analysis. BMC Rheumatol, 2023. 7 (1): p. 41.
[2] Nikiphorou, E. and S. Ramiro, Work disability in axial spondyloarthritis. Current Rheumatology Reports, 2020. 22 : p. 1-8.
[3] Boonen, A., et al., 2021 EULAR points to consider to support people with rheumatic and musculoskeletal diseases to participate in healthy and sustainable paid work. Annals of the rheumatic diseases, 2023. 82 (1): p. 57-64.
Line diagram of mean WAS scores at each timepoint.
Cost-effectiveness acceptability curve showing the probability that the 12-month PT-led vocational intervention is cost-effective compared with usual-care, over a range of values for the willingness-to-pay for an additional quality-adjusted life year (QALY).
Acknowledgements: This study is funded by the Dutch Arthritis Society (ReumaNederland) and the Scientific College of Physical Therapy (WCF) of the Royal Dutch Society for Physical Therapy (KNGF).
Disclosure of Interests: Nienke Bakker: None declared, Jesper Knoop: None declared, W.B. van den Hout: None declared, Nathan Hutting: None declared, Josephine Engels: None declared, J.B. Staal: None declared, Marieke van der Leeden: None declared, Annelies Boonen Pfizer, Novartis, UCB, Galapagos, Eli-Lilly, Abbvie, Annemiek Willemze: None declared, Michael Nurmohamed: None declared, M.G.J. Gademan: None declared, T.P.M. Vliet Vlieland: None declared, Salima van Weely: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (