

Background: Health literacy (HL) has been deemed central to the prevention and control of noncommunicable diseases by the World Health Organisation (WHO), including the rheumatic and musculoskeletal diseases. However, the association between HL, other social determinants of health, patient-reported outcomes and clinical outcomes in people with inflammatory arthritis (IA), remains poorly understood.
Objectives: To determine the association between HL, as defined by the widely applied nine-dimension Health Literacy Questionnaire (HLQ), and social determinants of health, clinical and non-clinical outcomes in people with IA recruited to the National Early Inflammatory Arthritis Audit (NEIAA) in England.
Methods: NEIAA is an observational cohort that includes adults with a diagnosis of an IA recruited since 2018. Patients with a confirmed IA diagnosis were identified from NEIAA and invited to complete a survey via an online platform between March and May 2024, comprising the HLQ; Work Productivity and Activity Impairment questionnaire; Generalised Anxiety Disorder (GAD-2) and Patient Health Questionnaire (PHQ-2); socio-demographics including employment, education and marital status; current and previous disease-modifying anti-rheumatic drugs (DMARDs); self-reported disease activity, tender and swollen joint counts. The HLQ has nine domains: 1. HPS: Feeling understood and supported by healthcare providers; 2. HSI: Having sufficient information to manage health; 3. AMH: Actively managing my health; 4. SS: Social support for health; 5. CA: Appraisal of health information; 6. AE: Ability to actively engage with healthcare providers; 7. NHS: Navigating the healthcare system; 8. FHI: Ability to find good health information; 9. UHI: Understanding health information well enough to know what to do. The survey was distributed to 3300 individuals with those responding matched with original records within the NEIAA. Multivariable linear or logistic regression analyses adjusting for age and gender were conducted to determine associations between each of the HLQ domains, and socioeconomic and clinical variables.
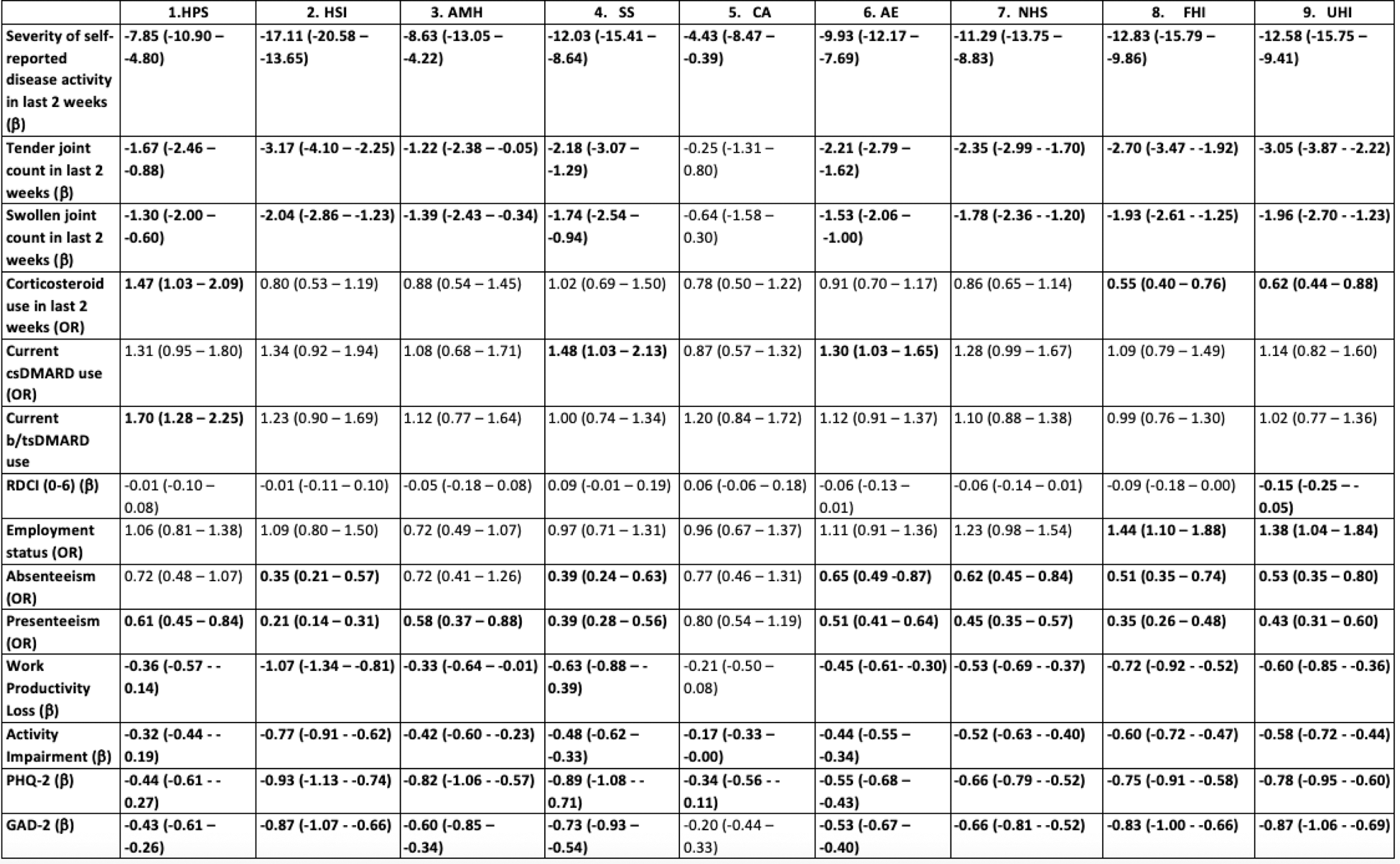
Results: A total of 995 patients with IA were included. The median age was 59 years (IQR 50-67) and 66% were female (Table 1). HL, across all domains, was associated with high self-reported disease activity in the past 2 weeks and greater anxiety and depression (GAD-2 and PHQ-2; Table 2). Low HL in all HLQ domains, aside from CA (5. Appraisal of health information), was significantly associated with more severe joint pain and stiffness and higher tender and swollen joint counts. High HL in the HPS domain (1. Feeling understood and supported by healthcare providers; OR 1.47 [1.03 – 2.09]) and low HL in FHI (8. Ability to find good health information; OR 0.55 [0.40 – 0.76]) and UHI (9. Understanding health information well enough to know what to do; OR 0.62 [0.44 – 0.88]) domains were associated with increased likelihood of corticosteroid use in the past 2 weeks. People on conventional synthetic DMARDs (csDMARDs) were more likely to have high HL in SS (4. Social support for health; OR 1.48 [1.03 – 2.13]) and AE (6. Ability to actively engage with healthcare providers; OR 1.30 [1.03 – 1.65]) domains, compared to those not taking a csDMARD. People on a biologic or targeted synthetic DMARD (b/tsDMARD) were more likely to have high HL in the HPS domain (OR 1.70 [1.28 – 2.25]), compared to those not taking a b/tsDMARD. No difference was seen in other domains of HL between those taking and not taking these drugs. Regarding work, high HL in FHI (OR 1.44 [1.10 – 1.88]) and UHI (OR 1.38 [1.04 – 1.84]) domains was associated with increased likelihood of being employed. Low HL in HLQ domains HSI, SS, AE, NHS, FHI and UHI was associated with high levels of absenteeism. Low HL in all domains except CA was associated with greater levels of presenteeism and greater work productivity loss. Low HL across all domains associated with greater activity impairment. Only low HL the UHI domain ( β -0.15 [-0.25 – -0.05]) was significantly associated with greater comorbidity burden, even after adjusting for smoking status. Outcomes for all analyses were largely unchanged after controlling for education as an additional covariate.
Conclusion: Low HL in some or all domains is associated with poorer physical and mental health, decreased likelihood of being on immune-modulating treatment, poorer work outcomes and greater comorbidity burden in IA. Low HL in domains 8 (Ability to find good health information) and 9 (Understanding health information well enough to know what to do) were associated with increased likelihood of corticosteroid use, poor work outcomes and greater comorbidity burden. Access to and understanding health information may therefore be a target for HL interventions to improve these aspects. Our study is the largest and richest IA cohort to date to explore HL in granular detail, using a robust and validated tool (HLQ) in IA. Our results highlight the unmet need to actively assess and account for HL in the management of patients, in line with WHO’s public health strategy.
Table 1. Demographics of study cohort and mean scores on Health Literacy Questionnaire by domain.
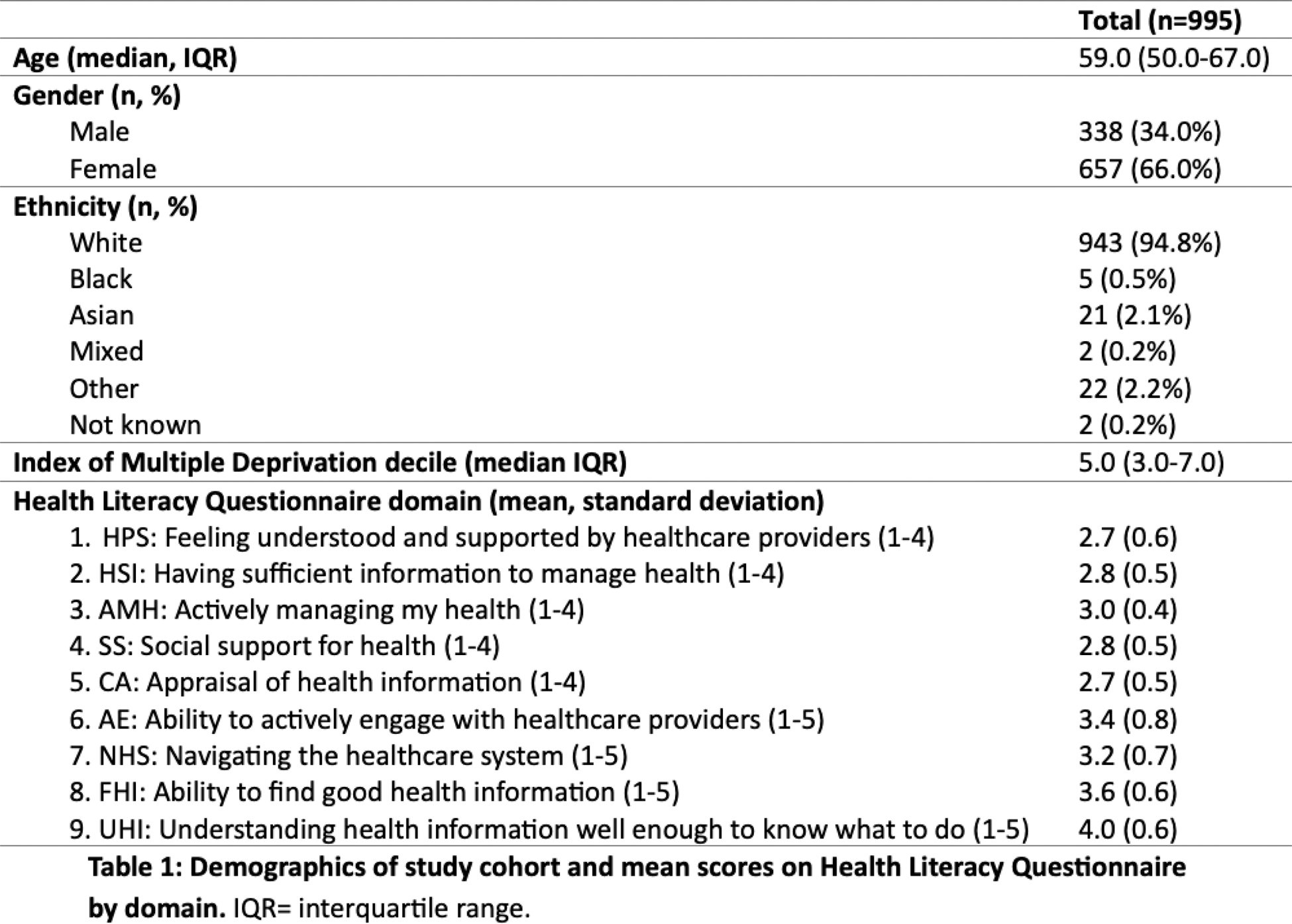
Table 2. Regression models, testing for associations between the nine domains of the Health Literacy Questionnaire and clinical and non-clinical outcomes, adjusted for age and gender. Outcomes of logistic regression models are presented as odds ratios (OR) and 95% confidence intervals (CI); outcomes of linear regression models are presented as beta coefficients (β) and 95% CI. csDMARD: conventional synthetic disease-modifying anti-rheumatic drug. b/tsDMARD: biologic or targeted synthetic disease-modifying anti-rheumatic drug. RDCI: Rheumatic Diseases Comorbidity Index. PHQ-2: 2-item Patient Health Questionnaire. GAD-2: 2-question Generalised Anxiety Disorder 2-item questionnaire.
REFERENCES: NIL.
Acknowledgements: This work was generously funded by a FOREUM Early Career Grant (EN) and the King’s College Hospital Charity (MD).
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (