

Background: Behçet’s syndrome (BS) is a systemic autoinflammatory vasculitis [1]. The pathogenesis of BS is associated with immune system dysregulation, in which multiple subsets of immune cells are involved [2]. CD161 + regular T cells (Treg) are a specific subset of Tregs. Previous studies have shown that CD161+ Treg cells can secrete several inflammatory cytokines during inflammatory states, exhibiting pro-inflammatory effects while impairing immune regulation [3]. CD161 + Treg plays an important role in autoimmune diseases.
Objectives: This study aims to investigate the alterations and clinical relevance of CD161 + Treg cells in BS, and to explore their role in the pathogenesis of the disease.
Methods: This is a retrospective, single-center study conducted in Beijing. A total of 182 patients diagnosed with BS in rheumatology and immunology department of Peking University People’s Hospital from 2018 to 2024 and 114 healthy controls (HC) were enrolled in this study. All patients met the International Criteria for Behcet’s Disease (ICBD) [4]. Disease activity was assessed using the Behçet’s Disease Current Activity Form (BDCAF) with all patients being in the active phase at enrollment (BDCAF ≥ 1). Basic demographic and clinical data were recorded at the time of enrollment. CD4 + CD25 hi CD127 low CD161 + T cells (CD161 + Treg) in peripheral blood were analyzed by flow cytometry. Statistical analysis was performed using the Wilcoxon rank-sum test, Chi-square test, and logistic regression analysis, with a p-value < 0.05 considered statistically significant.
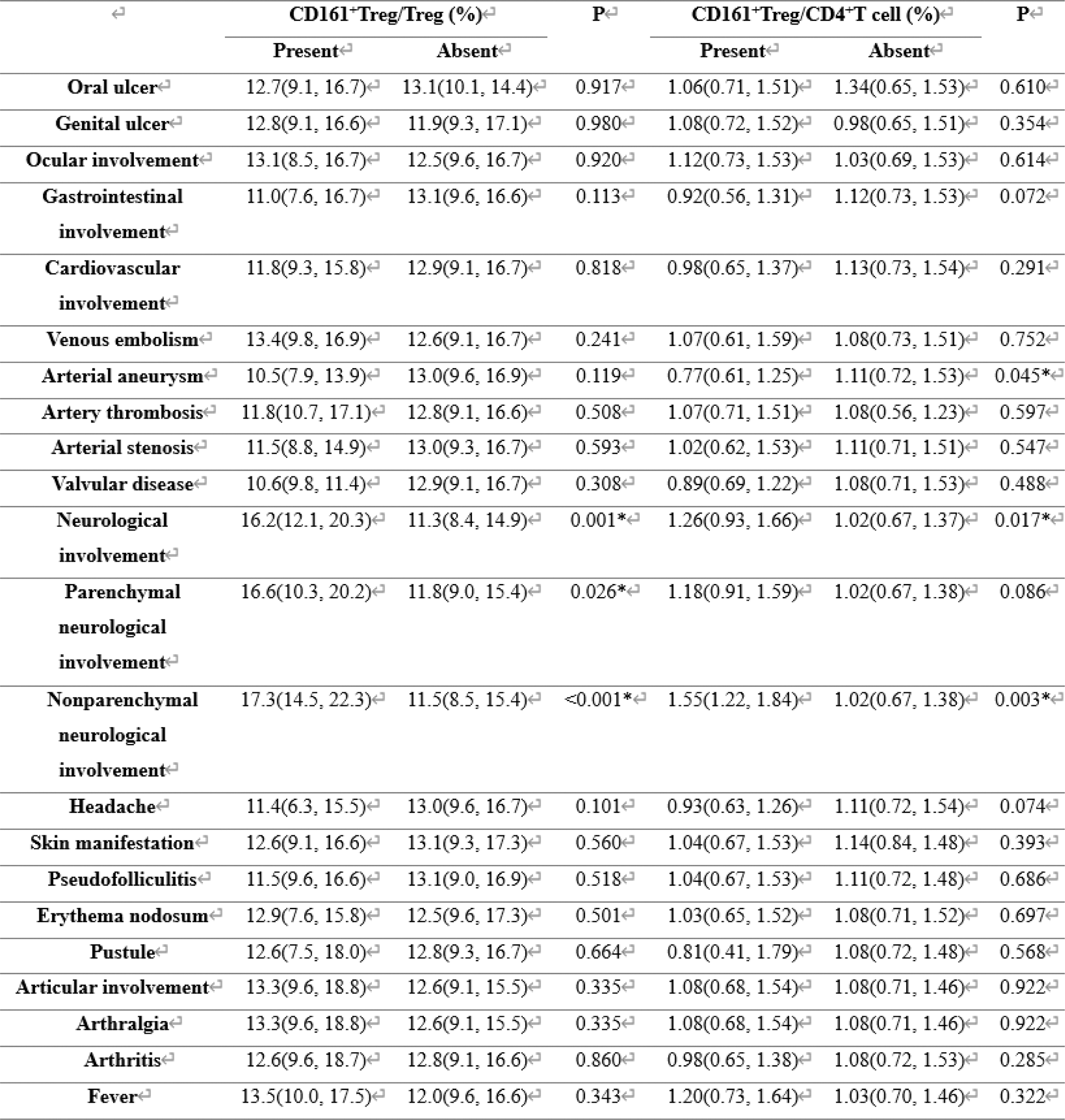
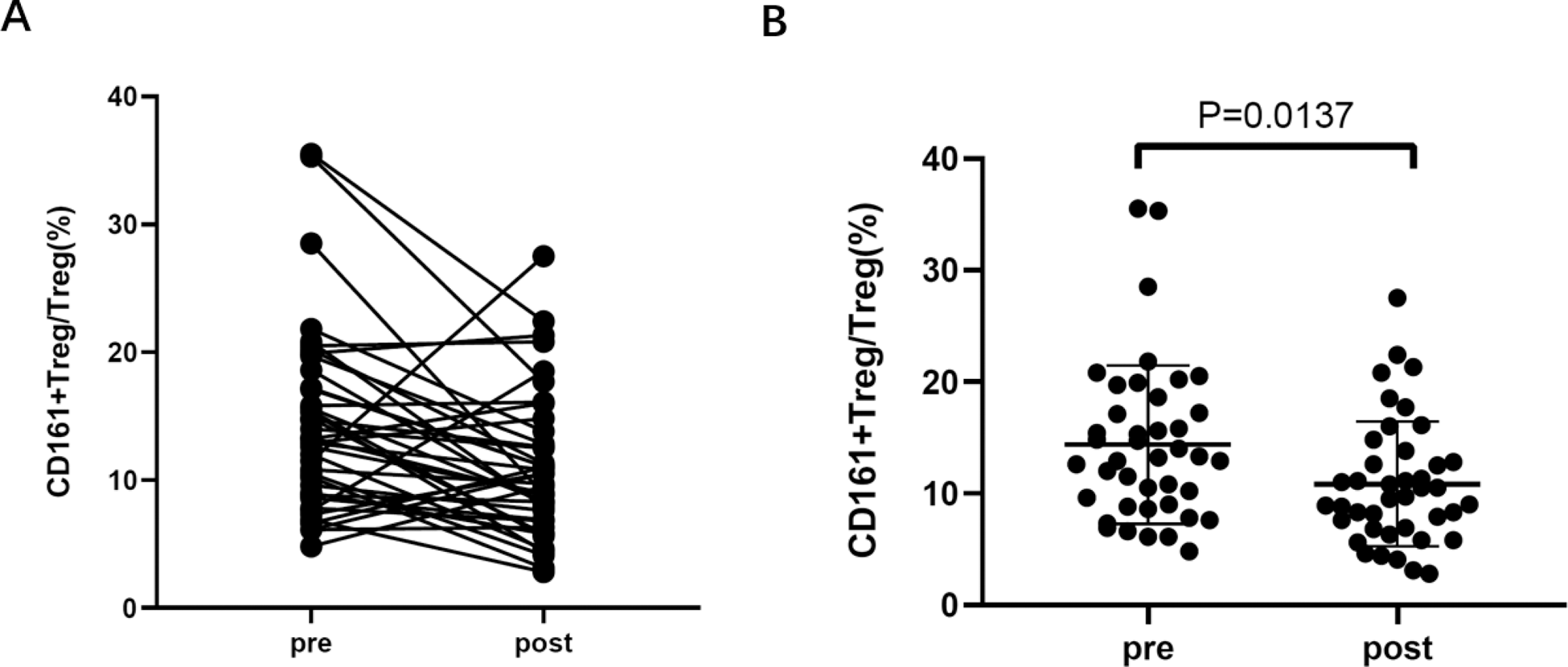
Results: Compared to HCs, the proportion of CD161 + Treg among total Treg [12.90 (9.60, 16.70) vs. 10.60 (8.59, 13.20), p<0.001] and among CD4 + T cells [1.10 (0.73, 1.53) vs. 0.84 (0.64, 1.09), p<0.001] in peripheral blood was significantly increased in BS patients (Figure 1). The proportion of CD161 + Treg among total Treg in peripheral blood was negatively correlated with the proportion of Foxp3 + Treg among CD4 + T cells (R = −0.348, p < 0.001), and positively correlated with the proportion of effector T cells among CD4 + T cells (R = 0.335, p < 0.001). Patients with neurological involvement had a higher proportion of CD161 + Treg among Treg [16.20 (12.10, 20.30) vs. 11.30 (8.40, 14.90), p = 0.001] and among CD4 + T cells [1.26 (0.93, 1.66) vs. 1.02 (0.67, 1.37), p = 0.017] in peripheral blood (Table 1). The higher proportion of CD161 + Treg among Treg was identified as a risk factor for neurological involvement in BS [OR = 1.123, 95% CI (1.027, 1.227), p = 0.011]. Forty-one BS patients were followed up after treatment, and the proportion of CD161 + Treg among Treg significantly decreased after treatment [13.20 (9.00, 17.20) vs. 9.70 (6.90, 12.80), p = 0.014] (Figure 2). In 29 of these patients, the proportion of CD161 + Treg decreased, and in 27/29 of these patients, BDCAF scores were lower after treatment. In contrast, only 5/12 patients with increased CD161 + Treg had lower BDCAF scores. Decreased CD161 + Treg after treatment was associated with lower disease activity (p = 0.001).
Comparasion of CD161 + Treg in peripheral blood between patients with BS and HC.
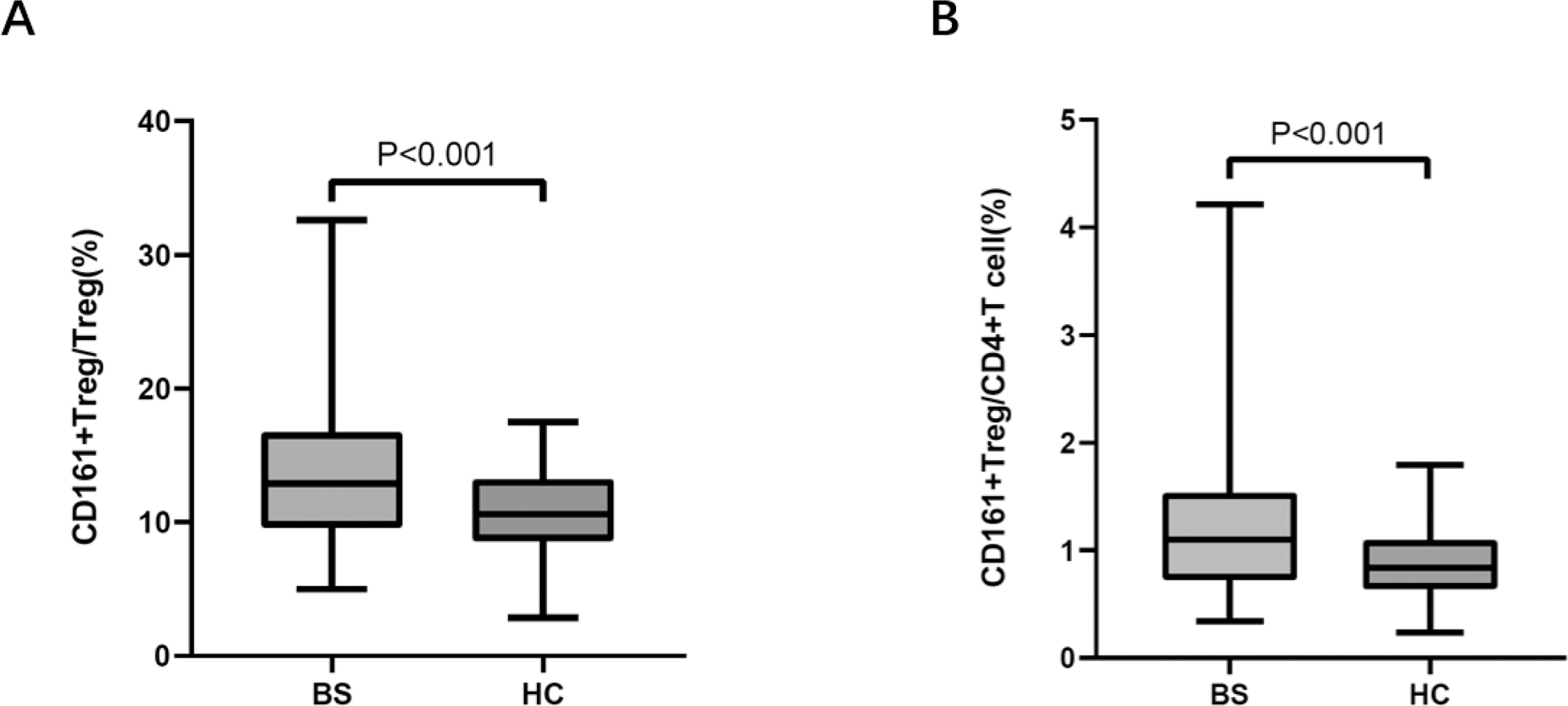
Table 1. Assosiation of different CD161 + Treg and different clinical manifestation of patients with BS
CD161 + Treg in patients with BS before and after treatment.
Conclusion: Patients with BS exhibit an increased proportion of CD161 + Treg among both total Tregs and CD4 + T cells in peripheral blood. A higher proportion of CD161 + Treg may serve as a risk factor for neurological involvement in BS. Following treatment, the proportion of CD161 + Treg in peripheral blood decreases, along with a reduction in BDCAF scores, suggesting its potential as a biomarker for disease activity in BS.
REFERENCES: [1] Emmi G, Bettiol A, Hatemi G, et al. Behçet’s syndrome[J]. Lancet, 2024. 403(10431): 1093-1108. DOI:/10.1016/s0140-6736(23)02629-6.
[2] Yazici Y, Hatemi G, Bodaghi B, et al. Behçet syndrome[J]. Nat Rev Dis Primers, 2021. 7 (1): 67. DOI:/10.1038/s41572-021-00301-1.
[3] Povoleri G A M, Nova-Lamperti E, Scottà C, et al. Human retinoic acid-regulated CD161(+) regulatory T cells support wound repair in intestinal mucosa[J]. Nat Immunol, 2018. 19(12): 1403-1414. DOI:/10.1038/s41590-018-0230-z.
[4] The International Criteria for Behçet’s Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria[J]. J Eur Acad Dermatol Venereol, 2014. 28(3): 338-47. DOI:/10.1111/jdv.12107.
[5] Bhakta B B, Brennan P, James T E, et al. Behçet’s disease: evaluation of a new instrument to measure clinical activity[J]. Rheumatology (Oxford), 1999. 38(8): 728-33. DOI:/10.1093/rheumatology/38.8.728.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (