

Background: Patients with rheumatoid arthritis (RA) are at increased risk of myocardial infarction (MI) and other cardiovascular events, likely due to a combination of several factors: increased prevalence of environmental RA risk factors such as smoking, direct effects of RA-related inflammation, indirect effects of the RA disease such as reduced physical activity, and effects of anti-rheumatic drugs. In this regard, the role of genetic predisposition to RA remains less well characterized. We have previously shown that RA-free siblings of patients with RA are at increased risk of MI, compatible with a role of genetics, but also that the genetic overlap between RA and MI is limited within the general population.
Objectives: To investigate whether an individual’s genetic predisposition to RA is associated with the risk of MI, both in RA and in the general population.
Methods: Using the Swedish EIRA case-control study, we identified 2692 patients with incident (diagnosed <12 months following first reported RA symptom-onset) RA diagnosed 2003-2020, and 2696 general population controls. In addition, using the Swedish Rheumatology Quality Register (SRQ) and its biobank (SRQb), we identified 1395 patients with incident RA diagnosed 2011-2019 and 2030 patients with established RA diagnosed 1955-2019. Polygenic risk scores (PRS) for RA were calculated as described in [1]. We linked data on these individuals to the Swedish Patient, Population and Death registers, and identified outcomes (incident MI, defined by ICD10-codes I20.0 or I21) during follow-up, which started at the date of the RA diagnosis (incident RA, and corresponding date for the controls matched to the EIRA cases for age, sex and residential area) or blood sampling (established RA in SRQb) and ended at the first occurrence of the outcome, emigration, death or end of the study period (December 31, 2022). We calculated the incidence of MI in each of the four groups, and visualized this using Kaplan-Maier curves. We assessed the association between the per-unit-increase in RA PRS and the incidence of MI using Cox regression, adjusting for age, sex, calendar year of start of follow-up, both separately in each of the four cohorts as well as combined using an indicator for cohort membership.
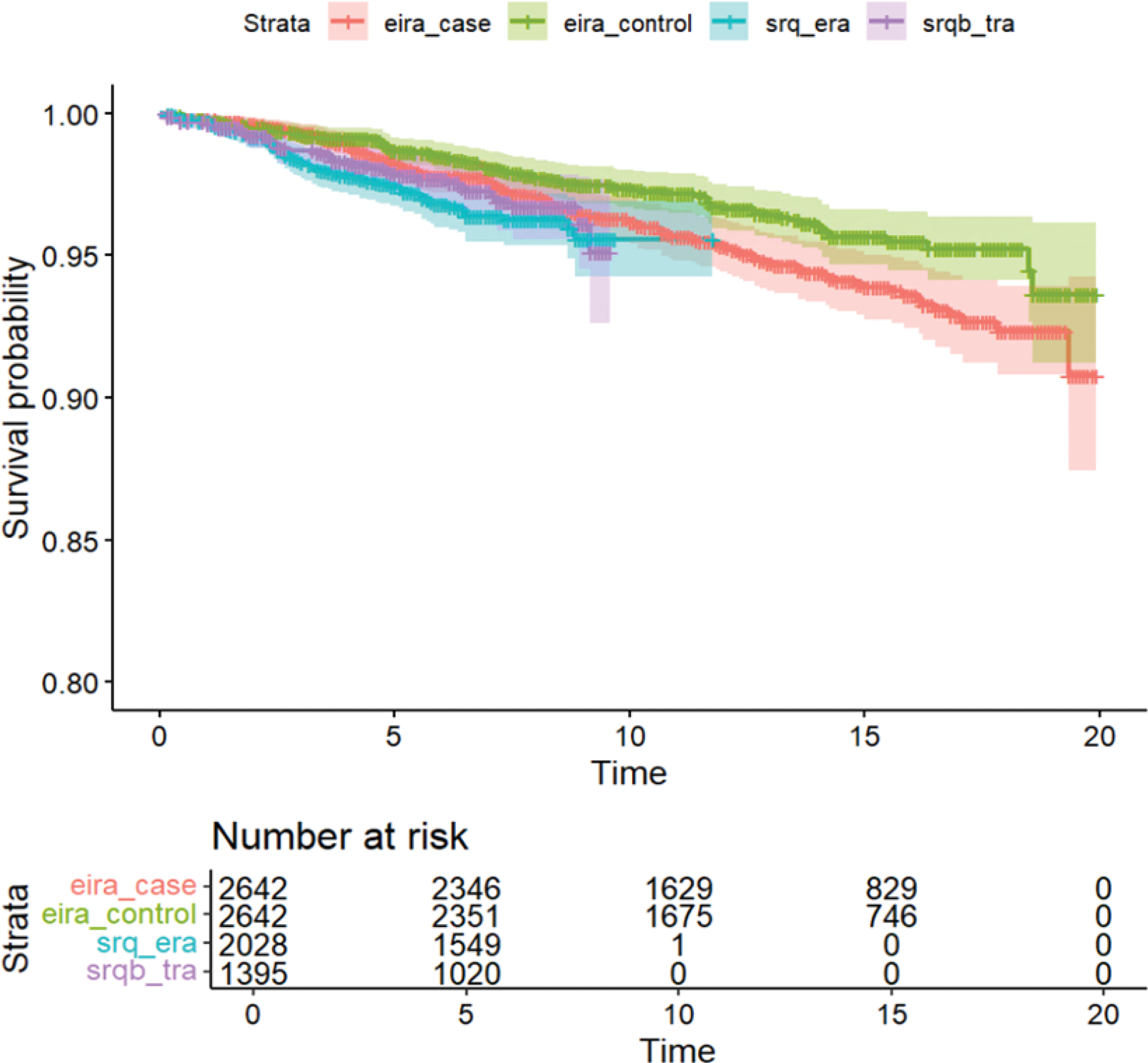
Results: 8707 unique individuals were included. Mean age at start of follow-up was 56 years and 72% were female. During an average of 10 years of follow-up, a total of 317 MI events occurred; mean incidence of 4.4 per 1,000 person-years in the RA group and 2.9 per 1,000 person-years in the general population sample (Figure 1). The RA PRS was not associated with MI incidence in the fully adjusted model, neither in the total sample nor in any of the RA subgroups or in the general population (Table 1).
Conclusion: An individual’s amount of genetic risk to develop RA is not associated with the risk of MI, neither in the presence, nor in the absence, of RA. These results suggest that the familiar aggregation of RA and MI risk is mainly due to other factors than genetic predisposition to RA, and underscore the role of traditional cardiovascular risk factors and RA disease management.
REFERENCES: [1] Sysojev AÖ, Alfredsson L, Klareskog L; Swedish Rheumatology Quality Register Biobank Group; Silberberg GN, Saevarsdottir S, Padyukov L, Magnusson PKE, Askling J, Westerlind H. Minor Genetic Overlap Among Rheumatoid Arthritis, Myocardial Infarction, and Myocardial Infarction Risk Determinants. Arthritis Rheumatol. 2024 Sep;76(9):1344-1352.
Study population, occurrence and hazard ratio of MI during follow-up
| Study population | N subjects | N incident MI | MI incidence per 1000 person-years | Adjusted Hazard Ratio per unit increase in RA-PRS* | Mean standardized RA PRS (SD) |
|---|---|---|---|---|---|
| All individuals | 8707 | 317 | 3.8 | 1.01 (0.89-1.15) | 0 (1) |
| Those with RA | 6065 | 230 | 4.4 | 0.95 (0.82-1.10) | 0.32 (0.89) |
| Matched controls** | 2642 | 87 | 2.9 | 1.16 (0.94-1.56) | -0.73 (0.86) |
*models adjusted for age at start of follow-up, sex, calendar year of start of follow-up and (where applicable) source cohort: RA or general population. **Matched to the early RA EIRA cases for age, sex and residential area.
Kaplan-Meier curve of MI occurrence over time since start of follow-up in three RA cohorts (Eira_case, SRQ_era, SRQb_tra) and the general population (eira_control)
Acknowledgements: Funding Swedish Research Council, Vinnova, ERA-PerMed, Swedish Heart Lung Foundation, ALF.
Disclosure of Interests: Helga Westerlind: None declared, Leonid Padyukov: None declared, Anton Sysojev Öberg: None declared, SRQ biobank group.: None declared, Saedis Saevarsdottir: None declared, Johan Askling Abbvie, BMS, Eli Lilly, Galapagos, MSD, Pfizer, Roche, Samsung Bioepis, Sanofi.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (