

Background: Interstitial lung disease (ILD) is a major cause of morbidity and mortality in systemic sclerosis (SSc). High-resolution computed tomography (HRCT) is the standard to diagnose and assess ILD progression. Artificial intelligence (AI)-assisted HRCT interpretation may improve the quantification and characterization of SSc-ILD, revealing as a potential tool to monitor for disease progression in SSc-ILD.
Objectives: Primary objective: to evaluate the correlation between AI-assisted quantitative HRCT interpretation with pulmonary function tests (PFTs) in SSc-ILD, compared with traditional visual scoring methods. Secondary objective: to assess the correlation of clinical outcomes with AI-assisted vs visual score-derived parameters.
Methods: Our observational study included 33 patients with SSc-ILD (79% females; median age 57 years (IQR 47-73), disease duration 5 years (IQR 2-6), 76% anti-Scl70, 9% anti-centromere, 6% anti-RNA pol III, 6% anti-Pm/Scl, 3% anti-nuclear antibody positive). Forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1) and diffusing capacity for carbon monoxide (DLCO) also adjusted for alveolar volume were assessed at both time points. HRCT images were evaluated at two time points 1 year apart (IQR 0.75-2.5 years). Visual scoring was performed according to Kazerooni et al [1]: two radiologists with expertise in thoracic imaging evaluated the images independently and resolved any disagreements through consensus. AI-assisted analysis was performed using Thoracic VCAR software (GE Healthcare, United States) to quantify volumes and percentages of ground glass opacities (GGO), fibrotic lung involvement, and normal lung. Patients were classified as having progressive or non-progressive ILD based on Erice criteria [2]. Treatment changes between the two time points were also recorded.
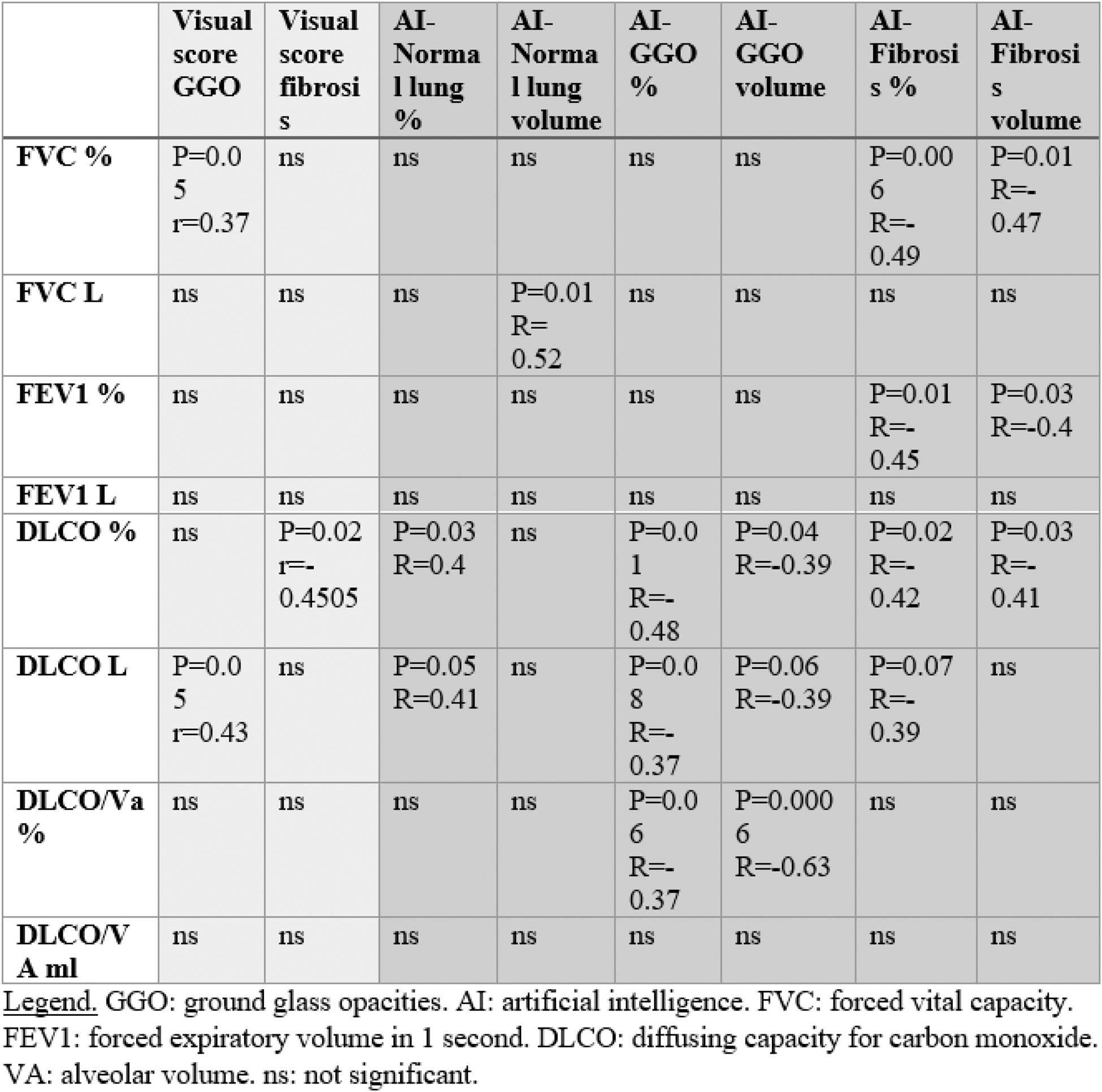
Results: Significant changes in HRCT visual scores were observed over time, as reflected by increasing percentages of fibrosis (p=0.0005) and GGO (p=0.06). AI-assisted analysis also revealed significant increase in the percentage of fibrosis (p=0.0007) and GGO (p=0.04), and a reduction of normal lung (p=0.009). AI-derived HRCT parameters correlated with PFTs, particularly with FVC and DLCO, at both timepoints, whereas visual scores showed minor correlations (Tables 1 and 2). Progressive ILD according to Erice criteria was observed in 48% of patients and correlated with the AI-determined volume of fibrosis at the second timepoint. No correlation was observed between the visual score and ILD progression.
Conclusion: AI-assisted quantitative HRCT analysis outperforms visual scoring in assessing the progression of fibrosis in patients with SSc-ILD, and show more significant correlations with PFT values. Subtle changes detected by AI-assisted quantitative HRCT analysis may better suggest disease progression in patients with SSc-ILD over time. Longitudinal prospective validation is needed to integrate AI into clinical practice for SSc-ILD management.
REFERENCES: [1] Kazerooni EA, et al. Thin-section CT obtained at 10-mm increments versus limited three-level thin-section CT for idiopathic pulmonary fibrosis: correlation with pathologic scoring. AJR Am J Roentgenol. 1997 Oct;169(4):977-83.
[2] George PM, et al. Progressive fibrosing interstitial lung disease: clinical uncertainties, consensus recommendations, and research priorities. Lancet Respir Med. 2020 Sep;8(9):925-934.
Table 1. Correlations between PFTs and visual score or AI interpretation of HRCT at timepoint 1.
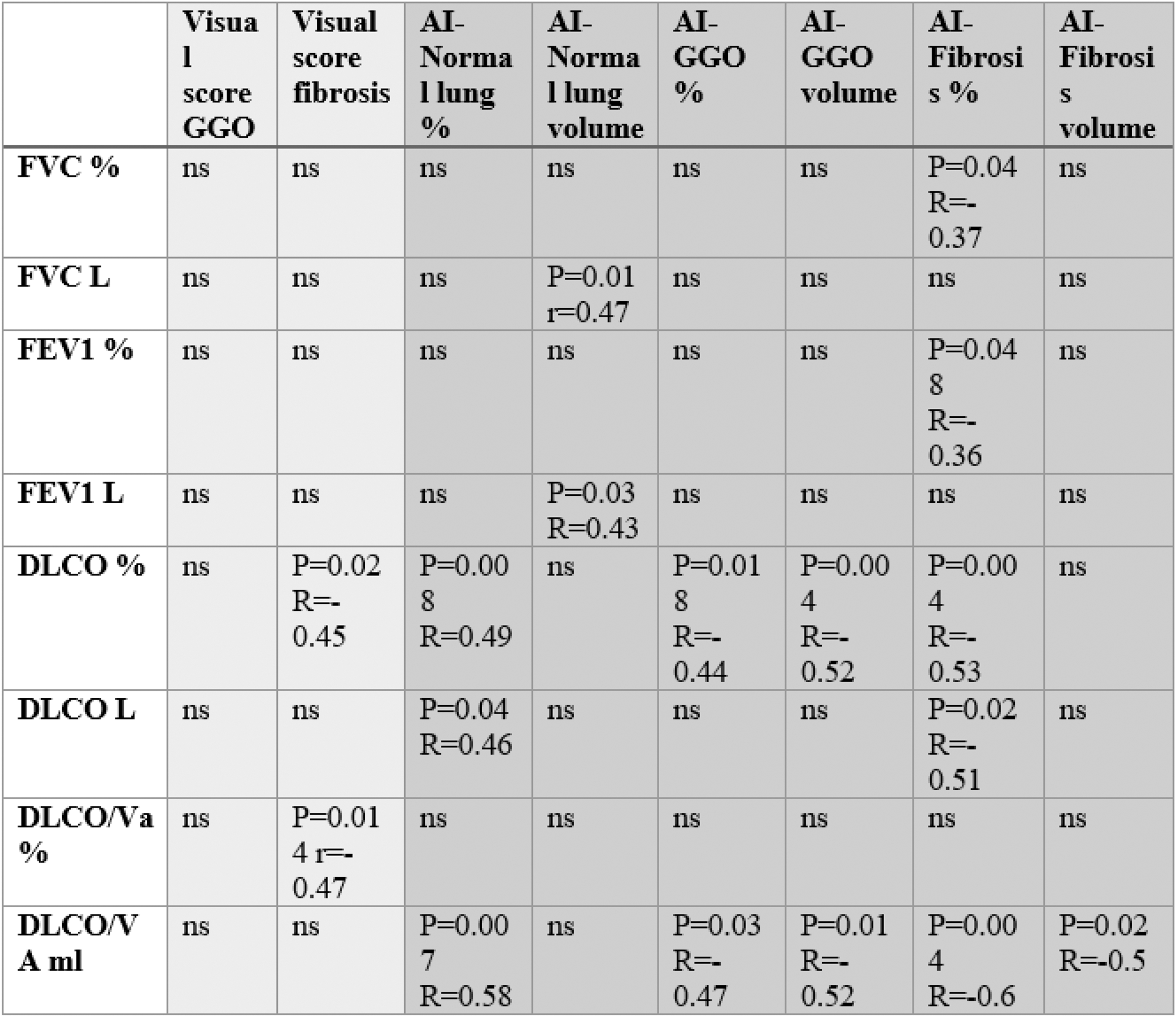
Table 2. Correlations between PFTs and visual score or AI interpretation of HRCT at timepoint 2.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (