

Background: Suboptimal adherence to disease-modifying antirheumatic drugs (DMARDs) remains a significant challenge in managing rheumatoid arthritis (RA), with only 20-70% of patients adhering to their prescribed regimens. Adherence is influenced by a complex interplay of macro-, meso-, and micro-level contextual factors, requiring a comprehensive understanding to address this problem effectively. The SQUEEZE project aims at developing, implementing and evaluating an eHealth facilitated innovative care model to improve DMARDs outcomes (e.g. adherence). Contextual analysis is the basis of intervention development, implementation strategies and informs evaluation.
Objectives: As a subproject of the SQUEEZE project, the aim of this study is a contextual analysis in 2 Swiss RA centres where we will implement the SQUEEZE care model. The contextual analysis will focus on multi-level contextual factors (i.e. barriers, and facilitators) and practice patterns related to chronic illness management and adherence management.
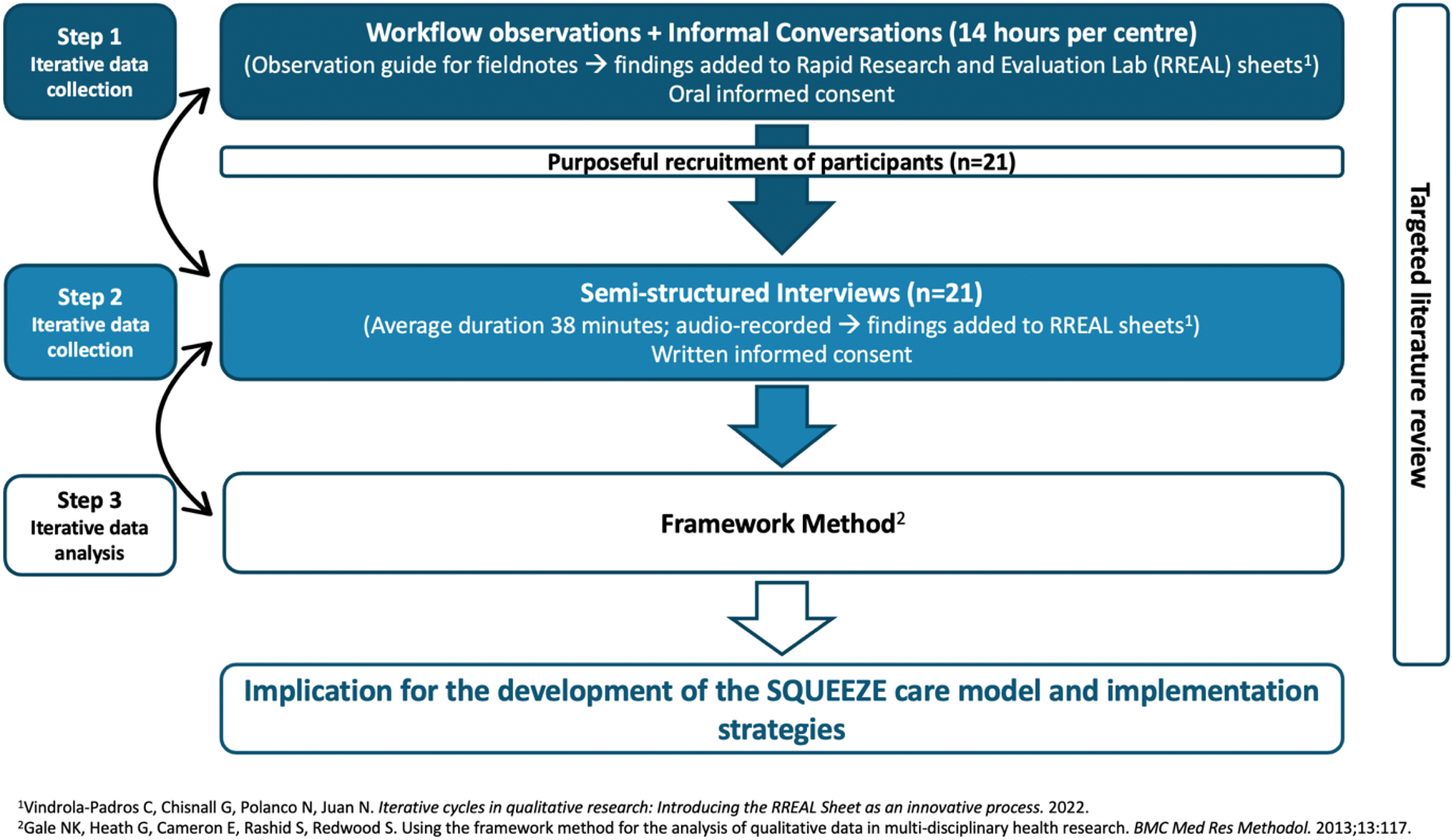
Methods: The contextual analysis was guided by the Basel Approach for coNtextual ANAlysis (BANANA) (i.e. component (COMP) 1-5). A combination of models and frameworks were selected: the Context and Implementation of Complex Interventions (CICI) framework to understand the interplay between context, implementation and interventions, complemented by the eHealth Enhanced Chronic Care Model (eCCM) to explore context in view of eHealth tools and chronic illness management principles (COMP 1). We used a rapid qualitative approach for data collection and analysis, engaging in iterative and focused efforts to investigate the factors influencing DMARDs adherence (Figure 1). Purposeful recruitment was used to ensure the inclusion of participants with specific knowledge, experience or characteristics that are crucial for addressing the objectives. Data were collected through clinical observations and semi-structured interviews with healthcare professionals (HCPs) (n=9) and patients (n=7) from the 2 Swiss rheumatology centres (Table 1), and other stakeholders (n=5) (COMP 4). In addition, a targeted literature review was conducted (COMP 2). The framework method was used to analyse and synthesise the data, informing the development of the SQUEEZE care model (COMP 4 and 5).
Results: Centres: Both centres are located in urban Switzerland. Centre 1, a private clinic staffed with 2 rheumatologists and 4 medical assistants, operated in a stable environment with clearly established roles, supporting care continuity and patient management. Centre 2, a university hospital clinic with 20 rheumatologists and 3 nurses, faced rapid organizational changes, including a new leadership structure. Practice patterns: Current practice in both centres focused on high-quality care delivered by well-educated HCPs, with a strong commitment on patient-centred care. Shortcomings included fragmented care due to poor coordination, lack of tools to monitor medication adherence and to support clinical decision-making, and variability in patient digital and health literacy. Key differences were observed in self-management support and delivery system design: Centre 1 employed a comprehensive self-management approach with active patient engagement, tailored interventions and educational sessions. In contrast, Centre 2 faced challenges in delivering comparable support due to time constraints and heavy staff workloads. Centre 1 used text messages to remind patients of appointments and ensure that they saw the same rheumatologist. In contrast, Centre 2 relied on informal methods leading to planning challenges. They also experienced high turnover among junior physicians disrupting continuity and affecting patient experience. Both centres used the Swiss Clinical Quality Management (SCQM) registry and its mobile application, but levels of engagement differ. Contextual barriers and facilitators: Socio-economically, limited reimbursement options for nurse-/medical assistant-led and eHealth interventions may hinder the implementation of new care models. Socio-culturally, 38.5% of the region’s population has migration background, and 65% of those over 65 years old are non-German speaking facing language barrier. In addition, rheumatologists expressed concern about a deterioration in the care quality if they delegate tasks to other HCP groups. Epidemiologically, a growing aging population with comorbidities complicates treatment. Legally, concerns about digital tool regulations, data security and misinformation were raised. However, both centres were open to change and use technology.
Conclusion: Findings revealed contextual similarities and differences between the two centres, requiring the SQUEEZE care model to be tailored to each to enhance its implementation and sustainability. Identified barriers, such as fragmented care and limited patient support, contrast with facilitators like availability of robust digital tools and openness to innovation.
Steps of the rapid qualitative data collection and analysis
Demographic data of the included patients and healthcare professionals.
| Sex (f) | Age in years
| RA duration in years
| Number of comorbidities
| Years of experience
|
|
|---|---|---|---|---|---|
| Patients (n=7) | 6 | 61.4; ± 12.2 | 12.6
| 3
| N/A |
| HCP (n=9) | 6 | 46.3; ± 12.1 | N/A | N/A | 14.3
|
Abbreviations: f: female; HCP: healthcare professionals; min: minimum; max: maximum; N/A: not applicable; RA: rheumatoid arthritis; SD: standard deviation.
REFERENCES: NIL.
Acknowledgements: The authors thank Centre 1, Centre 2 and Norha Vera San Juan for their (methodological) support, the research team for their dedication and the participants for sharing their experiences, which were essential to the success of this study.
Disclosure of Interests: Christina Wettengl: None declared, Sofia Calado: None declared, Simone Brand: None declared, Mary Louise Daly: None declared, Sabina De Geest Novartis course implementation science, Astellas adherence in transplantation, Sanofi, Pfizer, Novartis, Sanofi behavioral and implementation science, Erik Deman: None declared, Diego Kyburz UCB, Abbvie, UCB, Sanofi, Novartis, Pfizer, Roche, Abbvie, Chrysoula Manolaraki: None declared, Janette Ribaut Kantonsspital Winterthur, Berner Fachhochschule, Ines von Mühlenen Pfizer AG, Novartis, Roche Pharma AG, Celgene, Pfizer AG, Novartis, Roche Pharma AG, Celgene, UCB Pharma GmbH, Eli Lily SA, Pfizer AG, Abbvie, Agnes Kocher Abbvie, Boehringer Ingelheim, Pfizer, Boehringer Ingelheim, Swiss Nursing Science Foundation, the SQUEEZE project has received funding from the European Union’s Horizon Europe research and innovation programme under grant agreement no. 101095052, by UK Research and Innovation (UKRI) under the UK government’s Horizon Europe funding guarantee grant number 10055567 as well as the Swiss State Secretariat for Education, Research and Innovation (SERI).
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (