

Background: Advanced Physiotherapist Practitioners (APPs) in Canada have provided shared care with adult and pediatric rheumatologists for more than 25 years [1]. APPs train through a 10-month post-licensure, competency-based program that develops advanced rheumatology knowledge, skills and attitudes to assume roles in shared care models [2]. APPs are capable of triaging, assessing and managing complex rheumatic musculoskeletal cases, tasks traditionally completed by physicians [1]. The implementation of APPs in the health care system has demonstrated decreased wait times, improved access to care and high patient satisfaction [1,3]. As workforce issues increase in both adult and pediatric rheumatology in Canada, there has been a call to action to develop interdisciplinary and shared-care models incorporating health professionals such as APPs [4,5]. In 2020, an APP shared-care model was implemented in a pediatric rheumatology center in Ontario, Canada. Approximately 20% of the APP’s caseload are children with a rheumatic disease diagnosis, such as Juvenile Idiopathic Arthritis (JIA), that require long-term follow up [6]. For the APP to assume the majority of the shared-care for JIA, medical directives to communicate a diagnosis, order and interpret laboratory and diagnostic imaging and provide referrals to other specialities are essential [6]. Details on the safety, quality and efficacy of long-term APP shared-care for JIA is relatively unknown. Key Performance Indicators (KPIs) for JIA care have been established through the North American Pediatric Rheumatology Care and Outcomes Improvement Network (PR-COIN) measuring patient outcomes, safety and access to care [7]. PR-COIN’s vast registry of over 5000 unique patients provides an opportunity to benchmark the KPI’s of children with JIA seen by the APP in a shared-care model to investigate the quality, safety, and efficacy of care.
Objectives: This study aimed to analyze the frequency and outcomes of KPIs documented in an APP shared-care model for JIA management, and compare these findings to the PRCOIN registry data fro the same center as well as the registry as a whole to determine quality, safety and efficacy of care.
Methods: A retrospective chart review of JIA cases managed by one APP at a tertiary care pediatric rheumatology center between June 2022 to May 2024 was conducted. Quality KPIs included active joint count, pain score, physician and patient global assessment, cJADAS, physical function and Quality of Life measures. Safety KPIs included TB and uveitis screening, and lab monitoring. Access was measured by documentation of at least one visit in 12 months [7]. Documented frequency of KPIs and their outcomes by the APP were compared with PRCOIN data from same center (SC) (3 rheumatologists) and PRCOIN (16 centers).
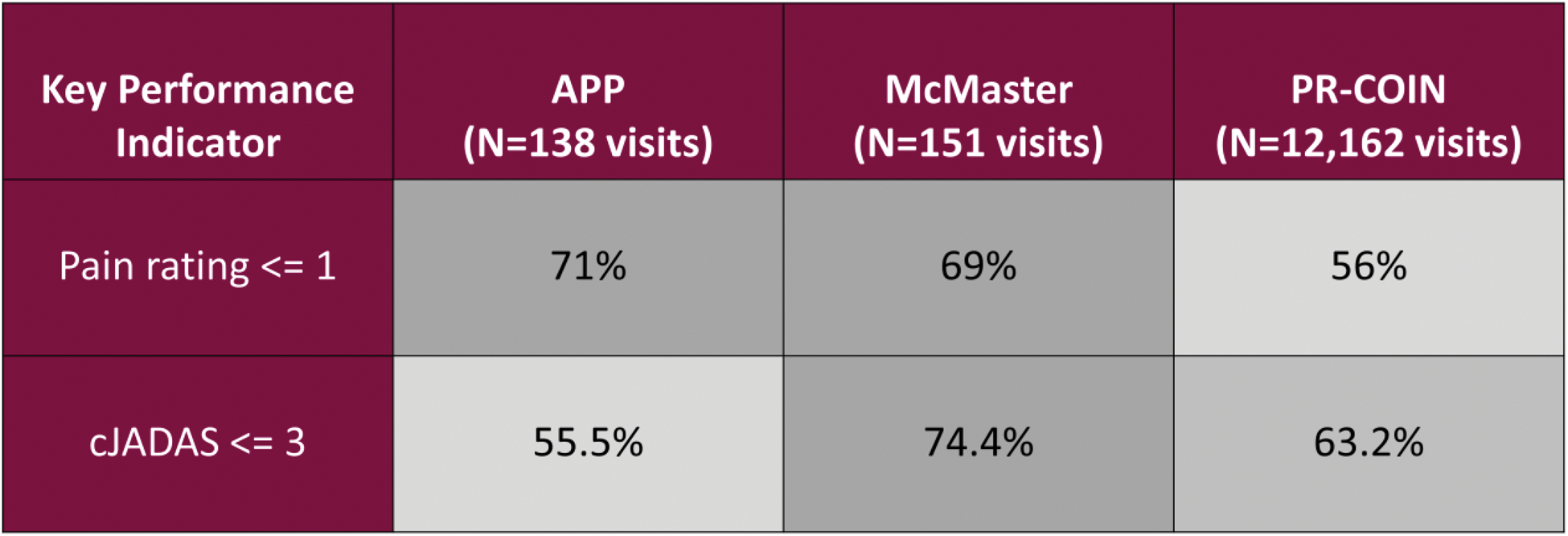
Results: The APP saw 33 unique patients with 1-8 visits each totalling 138 eligible visits. The SC saw 73 unique patients and PRCOIN saw 4,297 for a total of 151 and 12,162 eligible visits respectively. Sex (F:61–69%) was similar amongst all groups; mean (SD) age of patients followed by the APP was 9.3 years (4.7), SC 12.4 (4.5) and PRCOIN 13.3 (5.1). Most common JIA subtype for all groups was oligoarticular persistent (26 – 33%). Of patients seen by the APP, 9.1% had poly-articular RF+ JIA compared to SC and PRCOIN (1.6% and 5.0%, respectively). Eighteen percent of patients seen by the APP had Psoriatic Arthritis compared to SC and PRCOIN (1.7% and 9.2%, respectively). All KPI frequency thresholds were exceeded in the APP cohort (Table 1) and were comparable to or higher than the SC and entire PRCOIN Registry. Cases achieving low disease activity (cJADAS <3) were 55.5% for the APP, 74.4% for SC and 63.2% for PRCOIN. The APP had 71% of visits with pain rating of <1 compared to the SC (69%) and PRCOIN (56%) (Table 2).
Conclusion: The pediatric rheumatology APP shared-care model for management of children with JIA meets and exceeds quality and safety standards of care with comparable outcomes to care by pediatric rheumatologists. This further supports the implementation of APPs in the Canadian pediatric rheumatology healthcare network to mitigate growing caseloads that outpace the workforce supply. This study also contributes to the growing international body of literature demonstrating the impact physiotherapists can safely have working in advanced practice roles [8]. Limitations of this study include measurements of a single APP caseload, making this difficult to generalize. Next steps include expanding this study to other Canadian pediatric rheumatology centers for a broader investigation into the safety and efficacy of an APP shared care model.
REFERENCES: [1] Lundon K. ACR Open Rheumatol. 2020;2(4):242-250.
[2] Herrington J. Physiother Can. 2024 Mar 6;76(1):1-3.
[3] Vedanayagam M. Physiotherapy. 2021 Dec:113:116-130.
[4] Lee J. J Rheumatol. 2022 Feb;49(2):197-204.
[5] CRA. Position Statement Sustainability Ca Rheum Workforce. Rheum.ca 2022 Dec.
[6] Herrington J. Arthritis Rheumatol. 2023;75(suppl 4).
[7] Lovell DJ. Arthritis Care Res (Hoboken). 2011n;63(1):10-6.
[8] Tawiah A. Physiotherapy. 2021 Dec:113:168-176. Table 1. Frequency of Key Performance Indicators compared to the threshold set by PRCOIN, the Same Centre (3 rheumatologists) and the PRCOIN registry (16 centres).
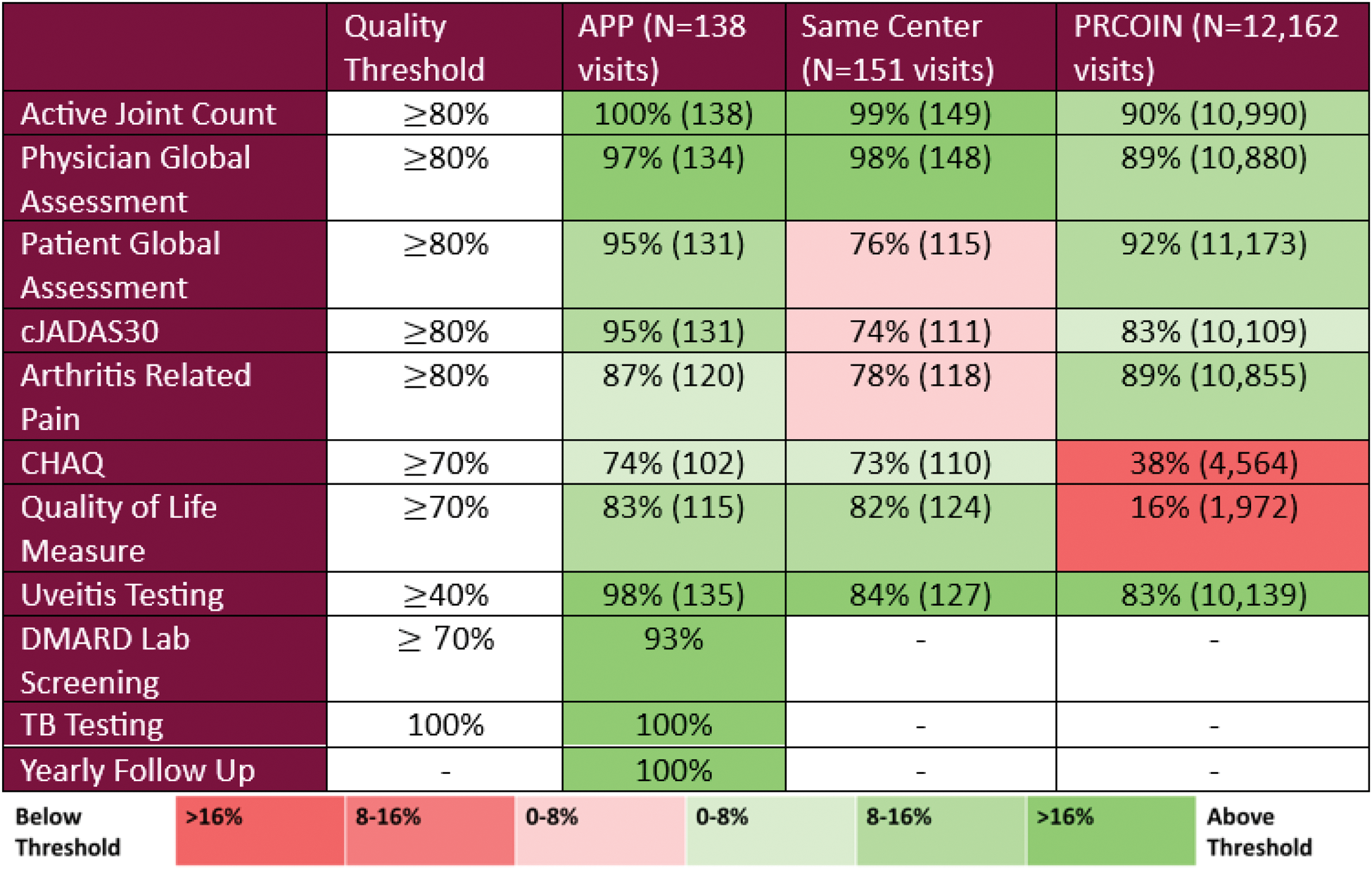
Table 2. Frequency of visits with Key Performance Indicators recorded below low disease activity thresholds. Pain scored by VAS(0-10). Sum of rheumatologic joint count (maximum 10), physician global assessment (0-10) and patient global assessment (0-10) equals cJADAS score with 0 indicating low disease activity.
Acknowledgements: We would like to acknowledge the support of Dr. Sheetal Vora and the PRCOIN Network.
Disclosure of Interests: Julie Herrington: None declared, Patrick Clarkin: None declared, Jade Singleton: None declared, Karen Beattie: None declared, Michelle Batthish Educational Grant NordicPharma 2024.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (