

Background: Patients with inflammatory joint diseases (IJD) are known to be at greater risk of cancer compared to the general population. However, long-term prospective studies of cancer related mortality in female IJD-patients are limited.
Objectives: To compare cancer mortality in female patients with IJD versus the general population.
Methods: NOR-DMARD is a Norwegian multicenter study including patients with IJD – rheumatoid arthritis (RA), psoriatic arthritis (PsA), and spondyloarthritis (SpA) - who initiate treatment with a disease-modifying antirheumatic drug (DMARD). Females participating in NOR-DMARD and controls were linked to several national registries through their unique personal identification number, with index date being the inclusion of the patient in NOR-DMARD. Controls were matched 10:1 by age, sex and municipality of residence. Cancer diagnosis and/or cause of death were identified by ICD-10 codes retrieved from the Norwegian Cancer and Cause of Death Registry. Statistical analyses were performed to calculate incidence rate ratios (IRR) and cumulative hazards adjusted for age and cancer diagnosis.
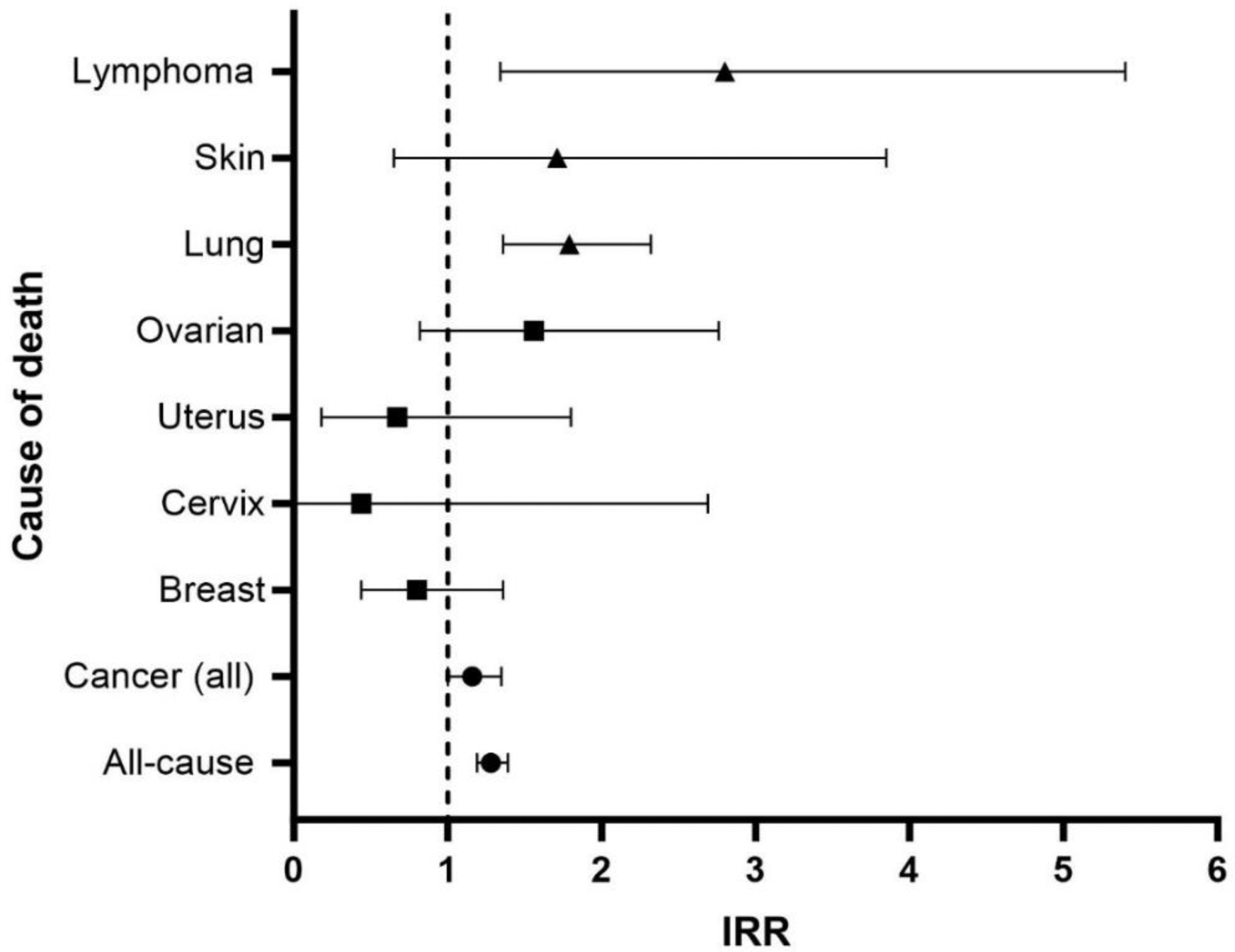
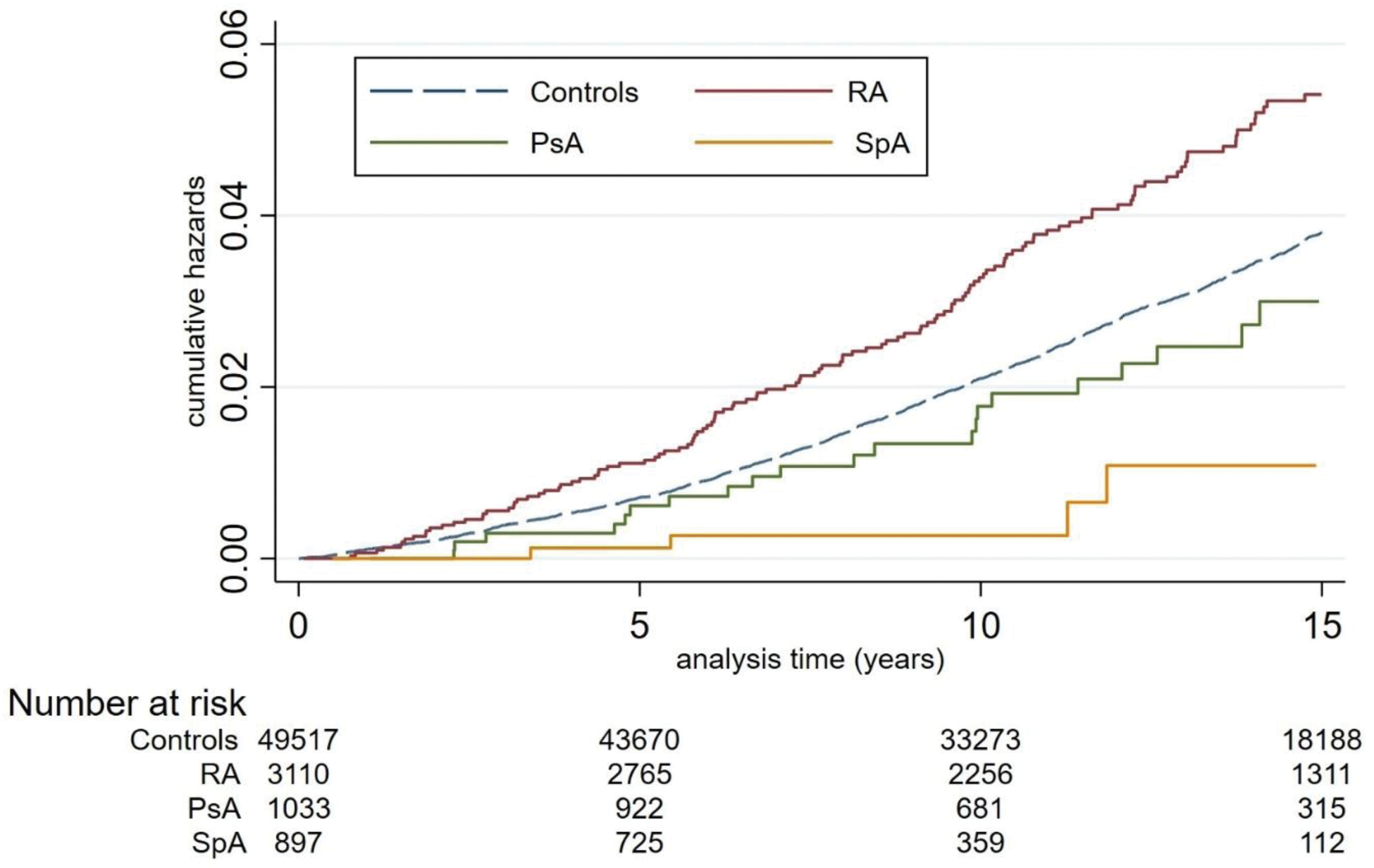
Results: From Dec 2000 to Dec 2020, a total of 5040 females with IJD (3110 RA, 1033 PsA, 897 SpA) were included (median (IQR) age 52 (39 – 62) years at baseline). The number of controls was 49,517 (median (IQR) age 51 (39-61)). Median (IQR) follow-up time was 11.9 (7.1-16.1) years. All-cause mortality during follow-up was higher in IJD patients with an IRR of 1.28 (95% CI 1.19-1.39), p<0.001 (Figure 1). For IJD vs controls, 5-year all-cause mortality per 10,000 was 67.0 (95% CI 57.3-78.3) vs 54.8 (95% CI 51.9-57.9); 10-year all-cause mortality was 93.1 (95% CI 84.3-102.8) vs 73.0 (95% CI 70.4-75.6). During follow-up a total of 541 IJD-patients developed cancer vs 4857 controls, IRR 1.12 (95% CI 1.02-1.22), p=0.02. Overall cancer mortality was also higher in IJD-patients compared to the controls (IRR 1.16 (95% CI 1.00-1.35), p=0.047). The age-adjusted hazard rate (HR) among those with a cancer diagnosis was 1.15 (95% CI 0.99-1.33), p=0.06. For IJD vs controls, 5-year cancer mortality was 20.8 (95% CI 15.7-27.5) vs 16.7 (95% CI 15.7-18.5) per 10,000; 10-year cancer mortality was 28.9 (95% CI 24.2-34.5) vs 24.4 (95% CI 22.9-26.0) per 10,000. For specific cancers, mortality was higher in IJD patients compared to controls for lymphoma (IRR 2.80 (95% CI 1.34-5.40), p=0.004). During follow-up, 0.5% IJD (n=27) and 0.4 % controls (n=185) were diagnosed with lymphoma, and of these, 44% (n=12) of IJD and 23% (n=43) of controls died of lymphoma. Age adjusted analyses remained significantly elevated for IJD patients compared to controls; given a diagnosis of lymphoma, compared to controls, HR 2.64 (95% CI 1.37-5.08) p=0.004. IJD patients experiencing non-follicular lymphomas were much more likely to die than controls, HR 3.41 (95% CI 1.37-8.47) p=0.008. Patients with IJD had a higher risk of being diagnosed with lung cancer (HR 1.85 (95% CI 1.49-2.30) p<0.001), but not a higher age-adjusted mortality upon cancer diagnosis compared to controls, HR 1.04 (95% CI 0.80-1.35) p=0.76). Patients with PsA had a higher risk of skin cancer compared to controls (HR 1.93 (95% CI 1.13-3.31) p=0.016). The incidence of melanoma was comparable in PsA vs controls (IRR 1.28 (95% CI 0.49-2.83) p=0.52), while non-melanoma was more frequent in PsA patients (IRR 3.49 (95% CI 1.43-7.73) p=0.004). However, PsA patients had comparable risk of dying after receiving a diagnosis of skin cancer (HR 0.79 (95% CI 0.08-6.50) p=0.79. Importantly, mortality due to gynecological cancers did not differ in the female IJD patients vs controls (Figure 1). By IJD diagnosis group, only patients with RA had higher cancer mortality risk compared to controls in age-adjusted analyses given a cancer diagnosis, HR 1.20 (95%CI 1.02-1.41) p=0.029 (Figure 2).
Conclusion: Females with IJD (RA, PsA, and SpA) have higher cancer rates and higher cancer mortality in general, especially given a diagnosis of lymphoma. RA patients have a 20% higher risk of dying of cancer compared to controls.
Crude incidence rate ratios (IRR) of specific cancer-related deaths in patients with inflammatory joint disease compared to controls (point estimates as triangles (non-gender specific cancers), squares (gender specific cancers) and circles (all cancers and all-cause mortality) with bars showing 95% CI).
Cumulative hazards of cancer mortality across inflammatory joint disease diagnosis groups compared to controls.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: Hilde S. Ørbo: None declared, Sho Fukui: None declared, Lene Maria Sundbakk: None declared, Sara K. Tedeschi Consulting fees from Merck, Avalo Therapeutics, Novartis, Kyowa Kirin, Fresenius Kabi, Tore K. Kvien Speakers bureaus from Grünenthal, Janssen, Sandoz, Consulting fees from AbbVie, Gilead, Janssen, Novartis, Pfizer, Sandoz, UCB, Grants from AbbVie, BMS, Galapagos, Novartis, Pfizer, Guro Løvik Goll Speakers bureaus from Novartis, Abbvie, Daniel H. Solomon Research grants from Janssen, Amgen, CorEvitas, Sella Aarrestad Provan: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (