

Background: Fibromyalgia (FM) is a debilitating condition affecting about 2% of the global population. It is marked by chronic, widespread musculoskeletal pain, fatigue, sleep disturbances, and mood disorders, severely impacting quality of life. Current multimodal treatments, combining pharmacological and non-pharmacological approaches, often provide only partial relief, leading to the inappropriate use of opioids and NSAIDs. This highlights the urgent need for novel therapeutic strategies targeting the underlying mechanisms of FM. One promising approach is biofeedback (BF), which has shown potential in enhancing stress coping—a key factor in nociplastic pain. However, current EULAR recommendations do not endorse BF due to limited evidence and low patient engagement. Integrating BF with Immersive Virtual Reality (IVR) could enhance its efficacy, as IVR has shown promise in managing pain, anxiety, and stress. Nevertheless, the role of IVR in FM treatment remains largely unexplored.
Objectives: This study aims to evaluate, for the first time, the efficacy of a treatment combining IVR with multi-sensor biofeedback (IVR-BF) in reducing chronic pain intensity, modulating sensory and emotional pain perception, and improving the overall impact of FM on daily functioning. Additionally, the study seeks to assess the effects of IVR-BF on physiological parameters associated with sympathetic hyperactivation, stress, and pain, including heart rate variability (HRV), respiratory rate (RR), and skin conductance levels (SCL).
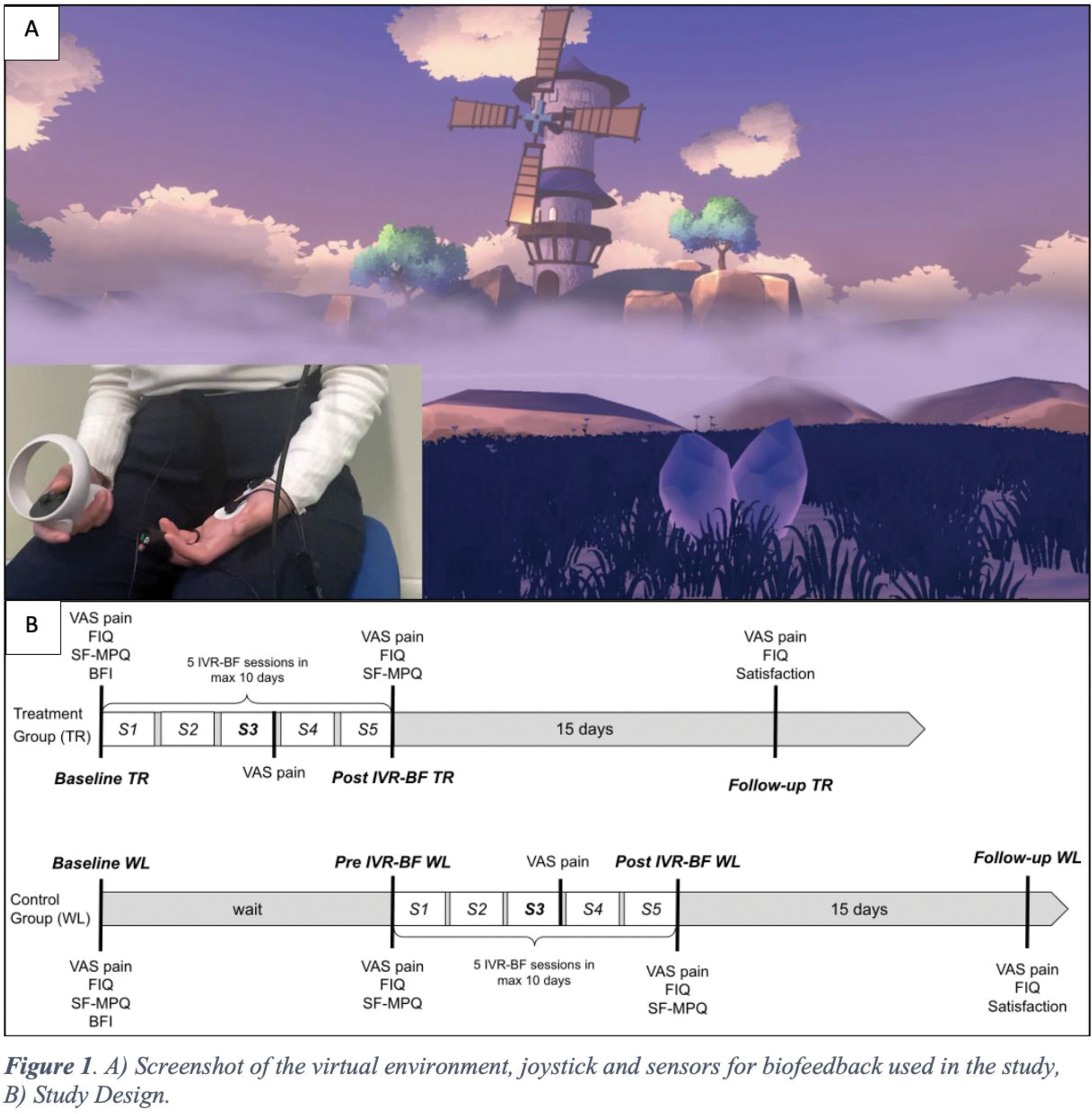
Methods: This single-center, open-label, pilot randomized controlled trial (NCT06100926) included patients meeting the 2016 ACR Revised Diagnostic Criteria for FM. Participants were randomly assigned (1:1) to a treatment group (TR), which received five IVR-BF sessions over 10 days, or to a wait-list control group (WL), which received the same intervention only when the TR group completed it. During the sessions, participants were immersed in a soothing virtual environment (Figure 1A) for 15 minutes while performing breathing and relaxation exercises. Questionnaires were administered at specific time points (Figure 1B) to assess pain intensity, subjective pain perception, overall FM impact, and personality traits, using the Visual Analog Scale (VAS), Short Form McGill Pain Questionnaire (SF-MPQ), Fibromyalgia Impact Questionnaire (FIQ), and Big Five Inventory (BFI), respectively. The primary outcome was a reduction in VAS pain scores in the TR group after five IVR-BF sessions compared to the WL group after the waiting period. Secondary outcome included improvement in FIQ in the TR group after five IVR-BF sessions compared to the WL group after the waiting period. In addition, a longitudinal analysis was conducted across all patients (TR+WL group) to assess trends in VAS pain, SF-MPQ, and FIQ scores throughout the trial. Physiological data were also recorded during the breathing and relaxation exercises conducted in each session to evaluate changes in HRV, RR, and SCL over time. Statistical analysis included ANOVA 2x2 mixed group and ANOVA repeated measures.
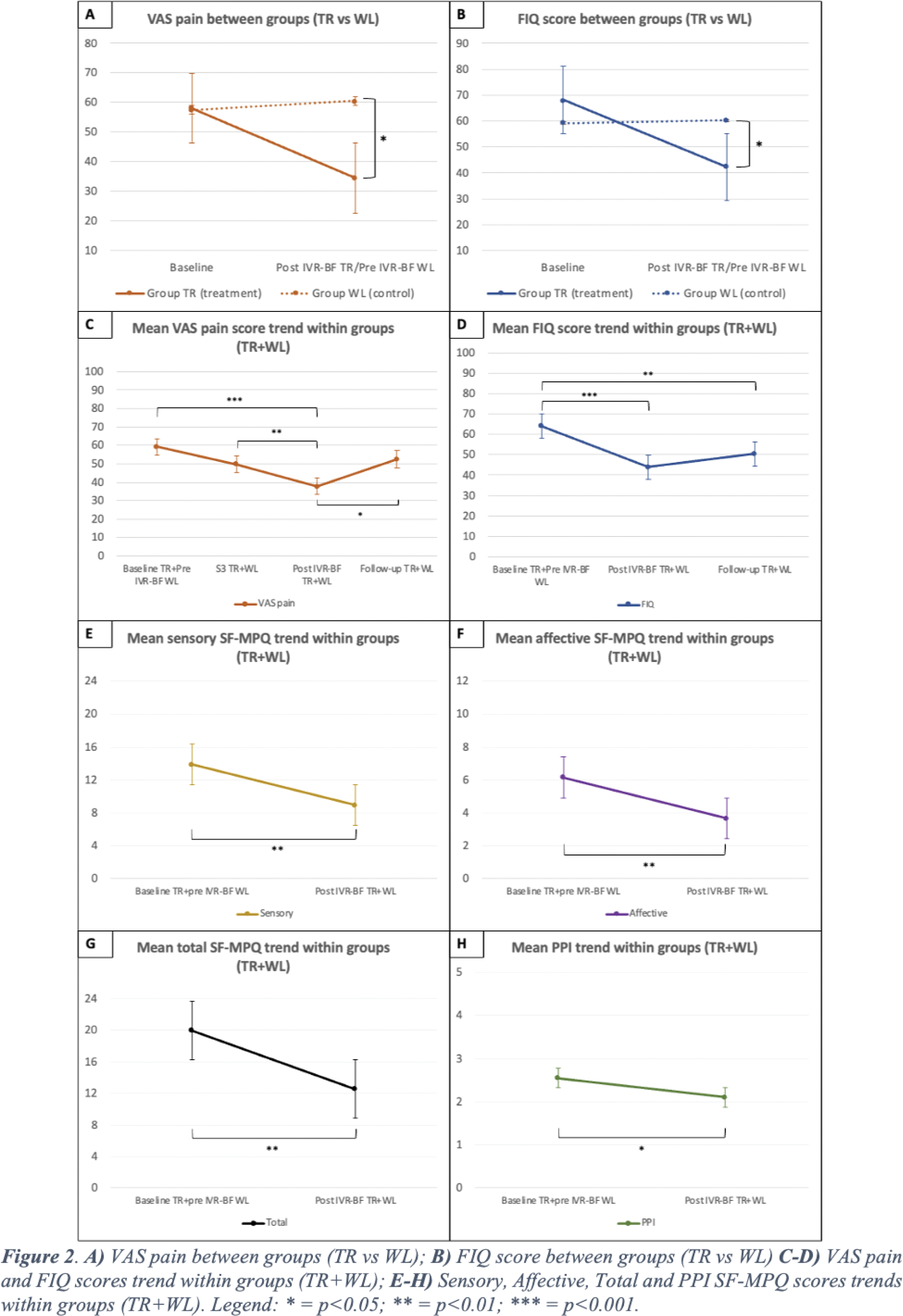
Results: A total of 20 female FM patients were enrolled and randomly assigned to either the TR group (10 patients) or the WL group (10 patient). Both groups were comparable at baseline. After five sessions of IVR-BF treatment, the TR group showed a significant reduction in VAS pain scores compared to the WL group after their waiting period (mean ΔVAS -26.00, 95% CI [-45.17; -6.83], p=0.011) (Figure 2A). The TR group also showed a significant improvement in FIQ scores compared to the WL group (mean ΔFIQ -17.90, 95% CI [-32.37; -3.43], p=0.018) (Figure 2B). A longitudinal analysis conducted across all patients (TR+WL) showed a rapid improvement in VAS pain score from the first to the last IVR-BF session, with significance reached after the final session (p<0.001). However, at the follow-up visit, VAS pain scores increased significantly, returning to pre-treatment levels (p=0.42). A significant reduction in FIQ scores was also noted after IVR-BF (p<0.001), with a mild, non-significant increase at follow-up (Figure 2C-D). Significant improvements in sensory, affective, total, and present pain index domains of the SF-MPQ were observed post-IVR-BF compared to baseline (p=0.002, p<0.001, p<0.001, p=0.03, respectively) (Figure 2E-H). No correlations were found between VAS pain, FIQ, SF-MPQ scores, and BFI personality traits (p>0.05). Regarding physiological data, statistically significant reductions in mean RR were observed across all sessions (p<0.001 for S1, S2, S3, S4, and S5), along with significant changes in SCL from the third session onward (S3: p=0.042; S4: p=0.018; S5: p=0.048). Improvements in HRV data were noted in Root Mean Square of Successive Differences (RMSSD) during the final two sessions (S4: p=0.018; S5: p=0.039), and in NN50 and pNN50 measures in sessions two, four, and five (S2: p=0.002 for NN50 and pNN50; S4: p=0.032 for NN50 and p=0.026 for pNN50; S5: p=0.010 for NN50 and p=0.017 for pNN50). No major adverse events were reported.
Conclusion: Multi-sensor IVR-BF emerges as a promising and effective non-pharmacological treatment for FM, considerably improving pain intensity, pain perception, and daily functioning. These improvements align with progressive enhancements in physiological parameters throughout the trial, suggesting better parasympathetic regulation and stress management. While IVR-BF leads to rapid improvements in FM-related pain and functioning, its efficacy may diminish once treatment is discontinued, highlighting the potential need for periodic re-treatment. Our preliminary findings support the recent growing recognition of immersive therapeutics by the FDA and advocate for the use of IVR in managing chronic musculoskeletal pain conditions like FM.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (