

Background: Gout, one of the most common inflammatory rheumatic conditions, is increasingly prevalent, adding pressure to healthcare systems. A treat-to-target (T2T) approach with urate-lowering therapy (ULT) to control serum urate levels is recommended for long-term treatment. We know that nurse-led care and self-monitoring can both support this T2T approach [1, 2]. Combining self-monitoring with nurse support during the initiation phase of ULT is a promising strategy to reduce physician visits and costs while maintaining or further improving quality of care. As large-scale trials on this combined approach are lacking, decision modeling offers a way to estimate its potential health and economic benefits.
Objectives: To estimate the cost-effectiveness of nurse-led home monitoring of serum urate (SU) compared to usual care in gout patients starting ULT in secondary care from a societal perspective using a decision modeling approach. A secondary objective was to estimate the effect of this intervention on time investments from nurses and rheumatologists.
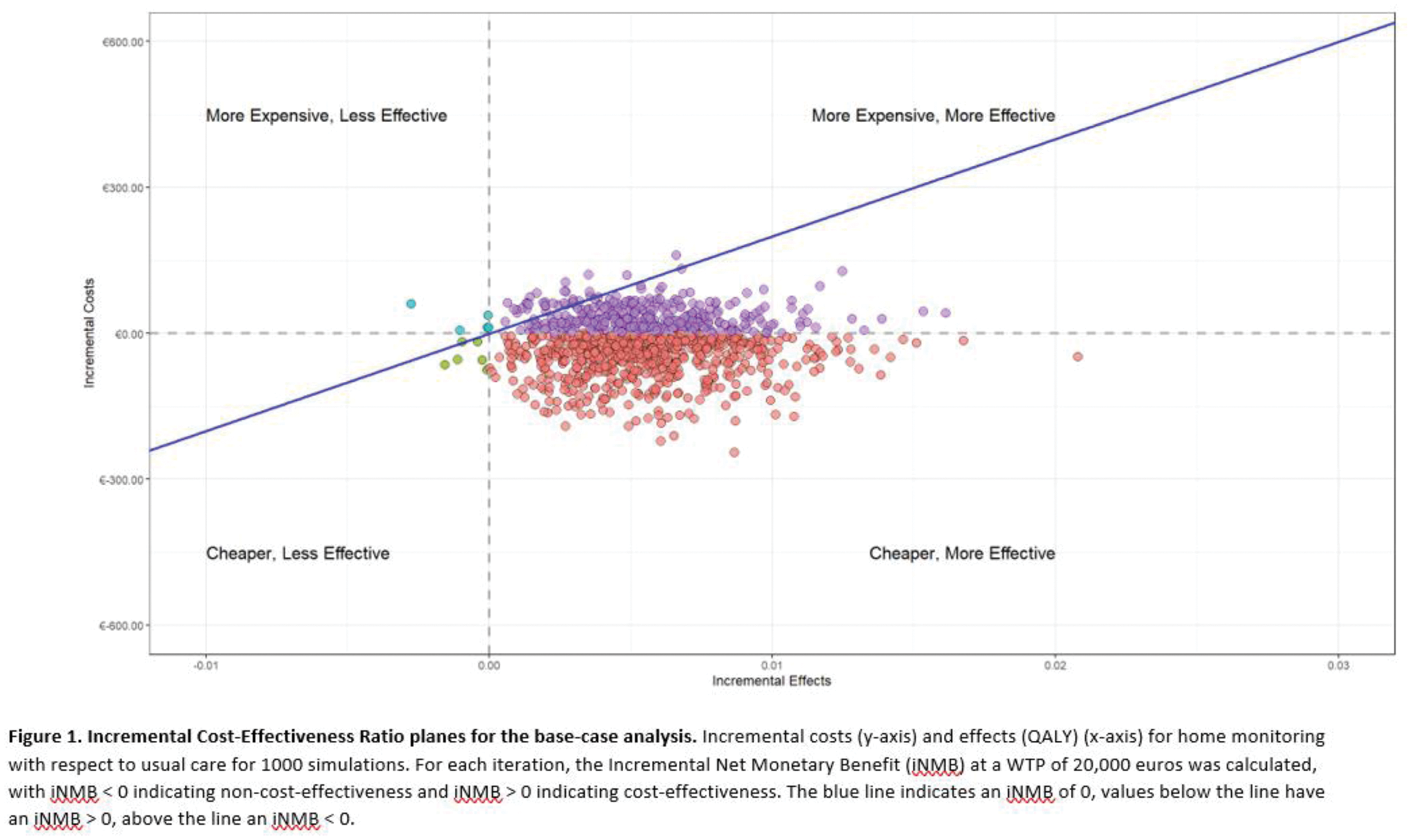
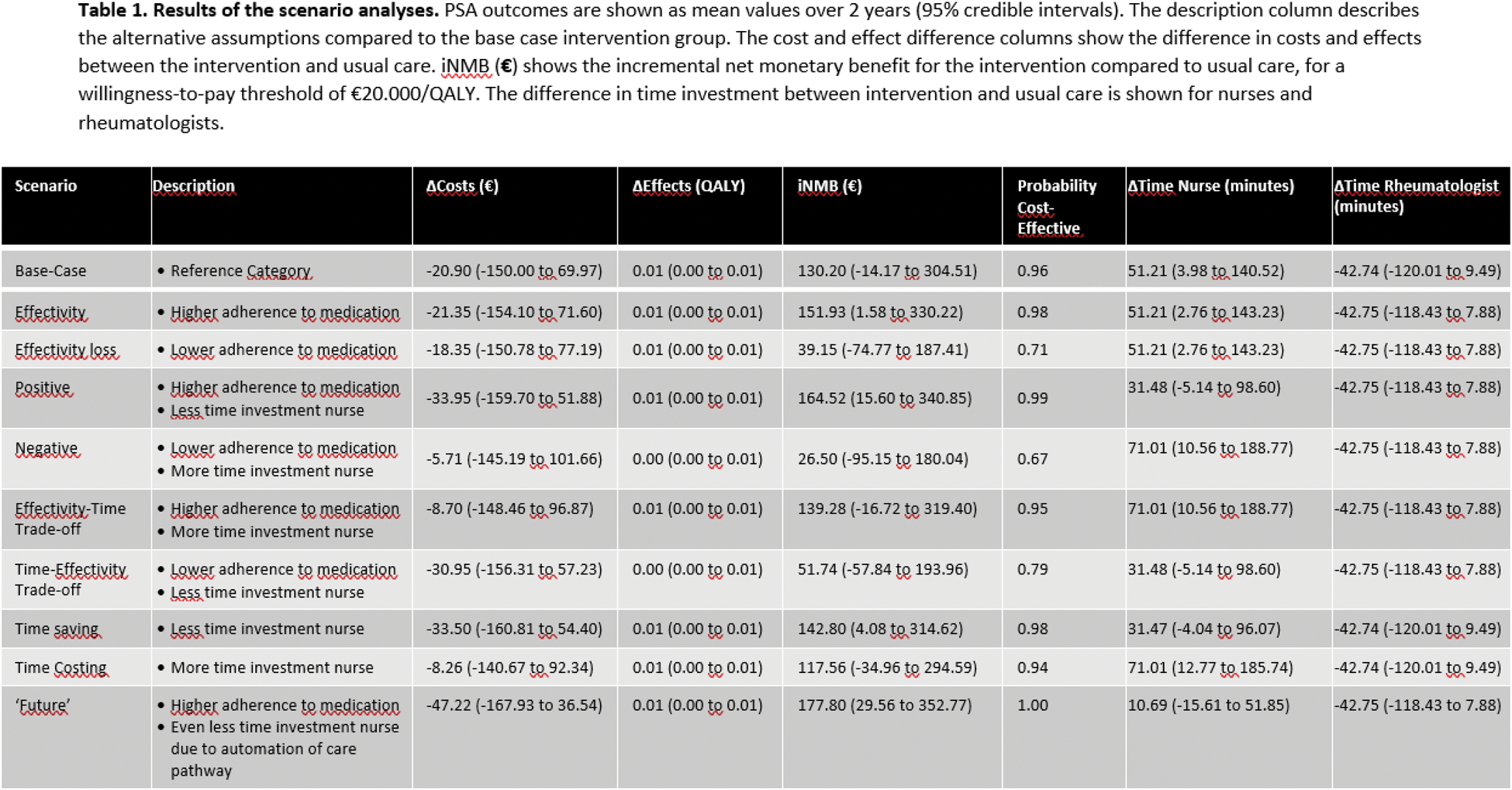
Methods: The modeled intervention involves specialized rheumatology nurses remotely supporting patients in stepwise dose adjustments of urate-lowering therapy using a T2T approach based on Point of Care Testing (POCT) for SU, which patients can perform at home. Usual care relies on the same T2T strategy with standard hospital-based laboratory measurements and routine rheumatologist visits. The model evaluates a two-year time horizon. Due to large differences in costs and clinical inputs between the initiation phase and the maintenance phase of gout treatment, the first was modeled using a decision tree (6-months), and the latter was modeled in three 6-month cycles using a Markov framework. Patients were categorized into four SU-based health states: one on-target state (SU < 0.36 mmol/L) and three off-target states, each representing incrementally higher SU levels (+0.12 mmol/L per category). Probability of medication adherence 6 months after starting ULT for usual care was based on internal hospital data. Transitions between health states in the maintenance phase in usual care were informed by gout cohort data from three Dutch hospitals. Adherence and health state transition probabilities in the intervention group were based on literature, expert opinion and discussion [2]. Probability of being on-target, or in either of the off-target states at 6 months, flare probabilities, 6-month health state utilities, and the disutility for a gout flare were derived from a cost-effectiveness study of febuxostat in chronic gout [3]. Costs were calculated using the Dutch Guideline for Economic evaluations in Healthcare, describing standardized costing methods [4]. Costs included ULT medication, healthcare provider time (rheumatologists and nurses), laboratory and home monitoring expenses, travel, work productivity losses, and flare-related care. Health outcomes were expressed as Quality-Adjusted Life Years (QALYs), derived by multiplying health state utilities by the time spent in each state. Cost-effectiveness was assessed using probabilistic sensitivity analyses (PSA). The incremental net monetary benefit (iNMB) was calculated at a €20,000 per QALY willingness-to-pay (WTP) threshold. The PSA involved Monte Carlo simulation (1,000 iterations) with parameter variability represented through assigned distributions. Results were reported as mean values with 95% credible intervals (CIs). Scenario analyses were used to explore the effect of alternative assumptions regarding the adherence rate and time investments of nurses within the intervention group, as these were the input variables with most uncertainty. These scenarios are detailed in Table 1.
Results: The probabilistic sensitivity analyses showed home monitoring was cost-effective with a mean iNMB of €130.20 (CI: -14.17 – 304.51), and resulted in a minor change in QALYs from 1.45 (CI: 1.39 – 1.52) in the usual care group to 1.46 (CI: 1.39 – 1.45) in the intervention group (2 years) (Figure 1). Rheumatologists saved 42.74 minutes (CI: -120.02, 9.49), while nurses spent 51.21 (CI: 3.98 – 140.52) minutes extra (2 years) (Table 1). The probability of being cost-effective was 0.96. Costs, QALYs, cost-effectiveness and time investment/savings for rheumatology nurses and rheumatologists under alternative scenarios are shown in Table 1.
Conclusion: Rheumatology nurse-led home monitoring of SU values for gout in secondary care can be cost-effective by reducing costs and improving health outcomes, although effects are modest. Compared to usual care, the intervention can save time for rheumatologists due to task reallocation towards rheumatology nurses. Future studies should focus on ways to reduce time needed from nurses while maintaining adherence of patients to ULT treatment. Automated feedback and risk stratification based on home monitored values can be a promising next step.
REFERENCES: [1] Doherty, M., Jenkins, W., Richardson, H., et al. (2018). Efficacy and cost-effectiveness of nurse-led care involving education and engagement of patients and a treat-to-target urate-lowering strategy versus usual care for gout: a randomised controlled trial. The Lancet, 392(10156), 1403-1412.
[2] Riches, P. L., Alexander, D., Hauser, B., et al. (2022). Evaluation of supported self-management in gout (GoutSMART): a randomised controlled feasibility trial. The Lancet Rheumatology, 4(5), e320-e328.
[3] Beard SM, von Scheele BG, Nuki G, Pearson IV. Cost-effectiveness of febuxostat in chronic gout. The European journal of health economics: HEPAC: health economics in prevention and care. 2014;15(5):453-63.
[4] Hakkaart-van Roijen L, Peeters S, Kanters T. Dutch Guideline for Economic evaluations in Healthcare. Dutch Care Institute; 2024.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (