

Background: Axial spondyloarthritis (axSpA) is a chronic inflammatory rheumatic disease primarily affecting the sacroiliac joints (SIJs) and spine, and with time irreversible structural damage can develop with an impact on function. Assessment of new bone formation (NBF) in the spine, and progression therein, is crucial for long-term management. This assessment still relies on radiography which is known to have limited sensitivity to change. However, novel imaging techniques, such as MRI-based synthetic CT (sCT) and low-dose CT (ldCT) have been shown to perform better than radiography in detecting NBF in the spine in patients with axSpA. Psoriatic arthritis (PsA), a related condition in the spondyloarthritis spectrum, shares similarities with axSpA but is also described to exhibit distinct axial joint manifestations. Nonetheless, data on these patterns of axial involvement in PsA remains scarce, particularly regarding imaging findings from ldCT. Additionally, the potential of sCT to visualize these structural axial lesions without radiation exposure, as accurately as ldCT, has yet to be explored.
Objectives: This study aims to 1) describe the occurrence of different types of NBF in the spine in patients with axSpA, PsA, and rheumatoid arthritis (RA), and in healthy controls (HC) using ldCT, and 2) determine the sensitivity and specificity of sCT to detect NBF with ldCT as the reference standard.
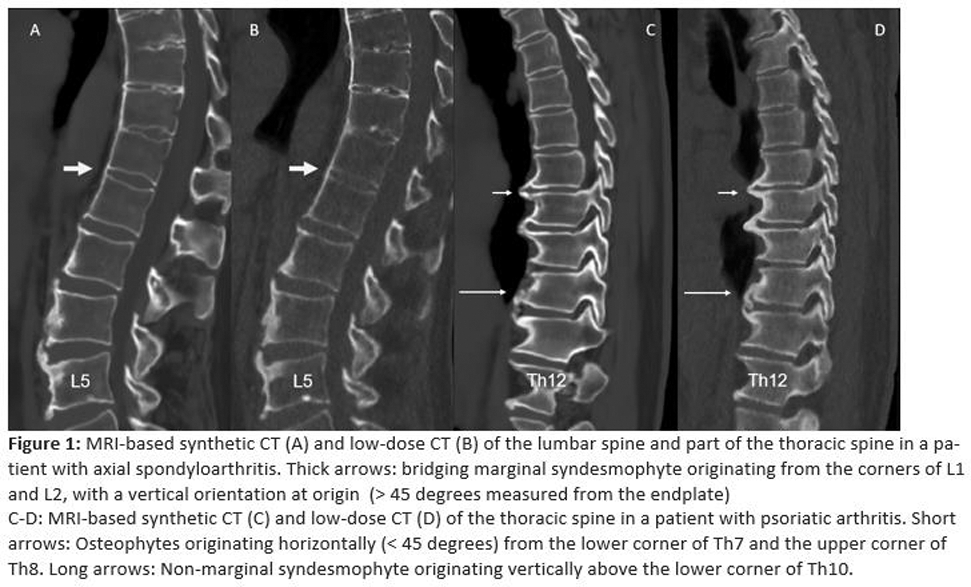
Methods: Patients who fulfilled the Assessment of Axial Spondyloarthritis International Society (ASAS) classification criteria for axSpA, or the ClASsification criteria for Psoriatic Arthritis (CASPAR) for PsA or the EULAR/ACR 2010 criteria for RA were included. Furthermore, HC who did not have a history of chronic back pain were included. All participants underwent ldCT and MRI of the entire spine. sCT was reconstructed using the BoneMRI v 1.8 application. BoneMRI or “synthetic CT” is a quantitative 3D MRI technique, based on a multiple gradient-echo sequence and a machine learning processing pipeline, which generates CT-like MR images. Images were pseudonymized and scored separately for ldCT and sCT by a reader blinded to all other clinical and diagnostic information. The types of NBF for scoring were defined prior to image evaluation. The following definitions were used; 1) Marginal syndesmophyte: Slim NBF originating from the margin/corner of the vertebra with a vertical (> 45 degrees compared with the endplate) direction at origin, 2) Non-marginal syndesmophyte: Non-slim NBF that arises away from the margin/corner of the vertebra, with a vertical (> 45 degrees) direction at origin, and 3) Osteophyte: NBF originating from the corner of the vertebrae with a horizontal (< 45 degrees) orientation at origin. Marginal syndesmophytes, non-marginal syndesmophytes, and osteophytes (bridging and non-bridging) were assessed on sagittal spinal images at each disco-vertebral unit (23 units in total) (see Figure 1), including anterior corners, central locations and posterior corners. If a bridging lesion was scored, non-bridging lesions could not be scored, and vice versa. Sum scores for each type of NBF across all spinal locations were calculated for each diagnosis group. The sensitivity, specificity and accuracy of sCT were determined using ldCT as the reference standard.
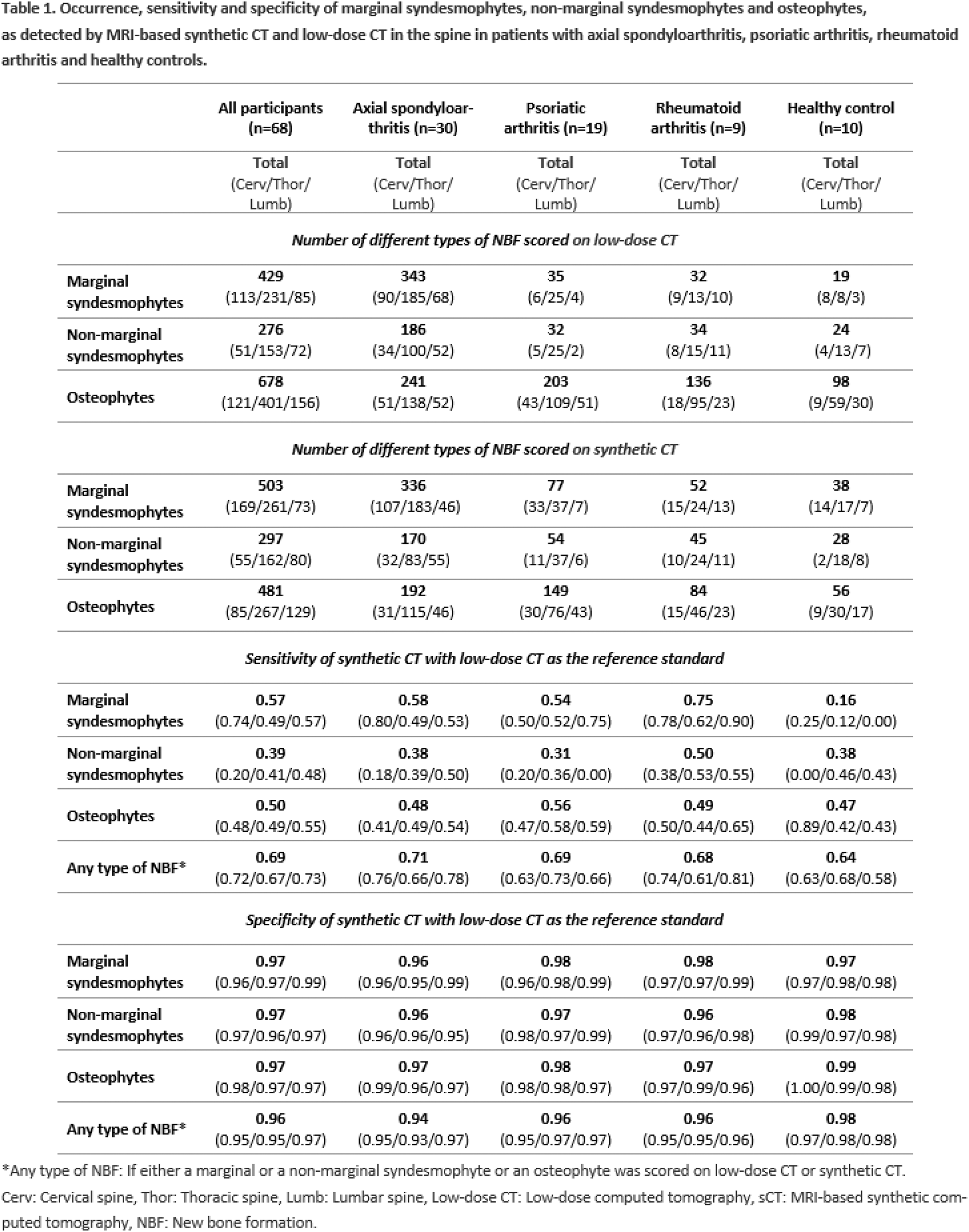
Results: A total of 68 participants (33 women, mean (± SD) age 52 (± 13,8)) were included: 30 with axSpA, 19 with PsA, 9 with RA and 10 HC. On ldCT, marginal syndesmophytes were most frequently scored in the axSpA group, with 343 lesions scored out of 4,140 possible (8.3%), predominantly located at the anterior corners and in the thoracic spine (see Table 1). In contrast, the prevalence of marginal syndesmophytes in the PsA, RA and HC groups ranged from 1.3% (PsA and HC) to 2.5% (RA). For non-marginal syndesmophytes, the highest score on ldCT was also found in patients with axSpA with a total score of 186 out of 2,760 (6.7%) compared to 1.8% in the PsA group, 4.1% in the RA group and 2.6% in HC. Osteophytes were the most frequently scored type of NBF on ldCT in all groups with the highest prevalence in the RA group (16.4%) and the lowest in the axSpA group (8.7%). Across all groups, the thoracic spinal segment had the highest sum scores for the three types of NBF with the lesions primarily located at the anterior corners. On sCT, the distribution and pattern of scored NBF closely resembled those on ldCT (Table 1). Using ldCT as the reference standard the sensitivity of sCT to detect any type of NBF in the spine in all groups together was 0.69 with a specificity of 0.96 and an accuracy of 0.92. The sensitivity of sCT to detect marginal syndesmophytes was 0.57, with a specificity of 0.97 and an accuracy of 0.95. For non-marginal syndesmophytes, sCT demonstrated a sensitivity of 0.39, a specificity of 0.97 and an accuracy of 0.94, and for the detection of osteophytes, the sensitivity of sCT was 0.50, the specificity 0.97 and the accuracy 0.92.
Conclusion: Marginal and non-marginal syndemophytes were more frequently observed in patients with axSpA compared to the other diagnosis groups on both ldCT and sCT. However, no pathognomonic pattern emerged to differentiate participants with PsA, RA and HC. Osteophytes were the most commonly scored type of NBF across all diagnosis groups, predominantly located in the thoracic spine. sCT demonstrated excellent specificity (≥ 0.94) and accuracy in detecting the individual types of NBF when using ldCT as the reference standard, and a moderate sensitivity. However, the sensitivity to detect any type of NBF was good (0.69, specificity 0.96), highlighting the large potential of this innovative sCT imaging technique for future assessment of NBF in the spine, and changes therein over time, in clinical trials and practice of patients with spondyloarthritis.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: Simone Tromborg Willesen: None declared, Jakob Møllenbach Møller: None declared, Kasper K Gosvig: None declared, Anna Enevold Fløistrup Hadsbjerg Novartis, Stylianos Georgiadis Novartis, UCB, Susanne Juhl Pedersen AbbVie, Novartis, MSD, Pfizer, and UCB, AbbVie, Novartis, MSD, Pfizer, and UCB, Novartis, Mikkel Østergaard Abbvie, BMS, Celgene, Eli-Lilly, Galapagos, Gilead, Janssen, MEDAC, Merck, Novartis, Pfizer, Sandoz, and UCB, Abbvie, BMS, Celgene, Eli-Lilly, Galapagos, Gilead, Janssen, MEDAC, Merck, Novartis, Pfizer, Sandoz, and UCB, Abbvie, BMS, Merck, Novartis and UCB.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (