

Background: Patients with psoriatic arthritis (PsA) have a well-known increased cardiometabolic risk. The beneficial effect of physical fitness on cardiometabolic and general health in the general population is generally known. However, data on cardiorespiratory fitness (CRF) in patients with PsA and its association with disease parameters and cardiometabolic risk are currently scarce.
Objectives: This study aimed to determine the level of CRF in patients with PsA compared to the general population and to explore the relation between the CRF level of patients with PsA and disease related parameters, cardiometabolic risk profile as well as patient-reported outcome measures (PROMs).
Methods: In this cross-sectional study, CRF was measured as peak oxygen uptake (VO 2 peak) during an incremental maximal cardiopulmonary exercise test on a cycle ergometer. VO 2 peak was compared to two different reference populations: a sedentary general population (Wasserman 2005) [1] and a Dutch Flemish physically active population (Lowlands Fitness registry 2021) [2]. VO 2 peak below 80% predicted following the Wasserman 2005 equation and/or below the lower limit of normal following the LowLands Fitness registry 2021 was considered as impaired CRF. The one-sided Wilcoxon rank-sum test was used to examine if CRF of patients was significantly decreased compared to the reference population. Spearman’s rank correlation coefficients (r S ) adjusted for age and sex were calculated to evaluate the relation between VO 2 peak in ml/min/kg and disease parameters, cardiometabolic risk parameters (additionally adjusted for BMI) as well as PROMs (additionally adjusted for PASDAS and BMI). Multivariable linear regression models with VO 2 peak expressed in ml/min/kg (log-transformed) as dependent variable were analysed. Using forward stepwise regression, disease and cardiometabolic risk parameters as well as PROMs were added to the basic model consisting of independent variables age and sex. Statistical significance was defined as p<.05.
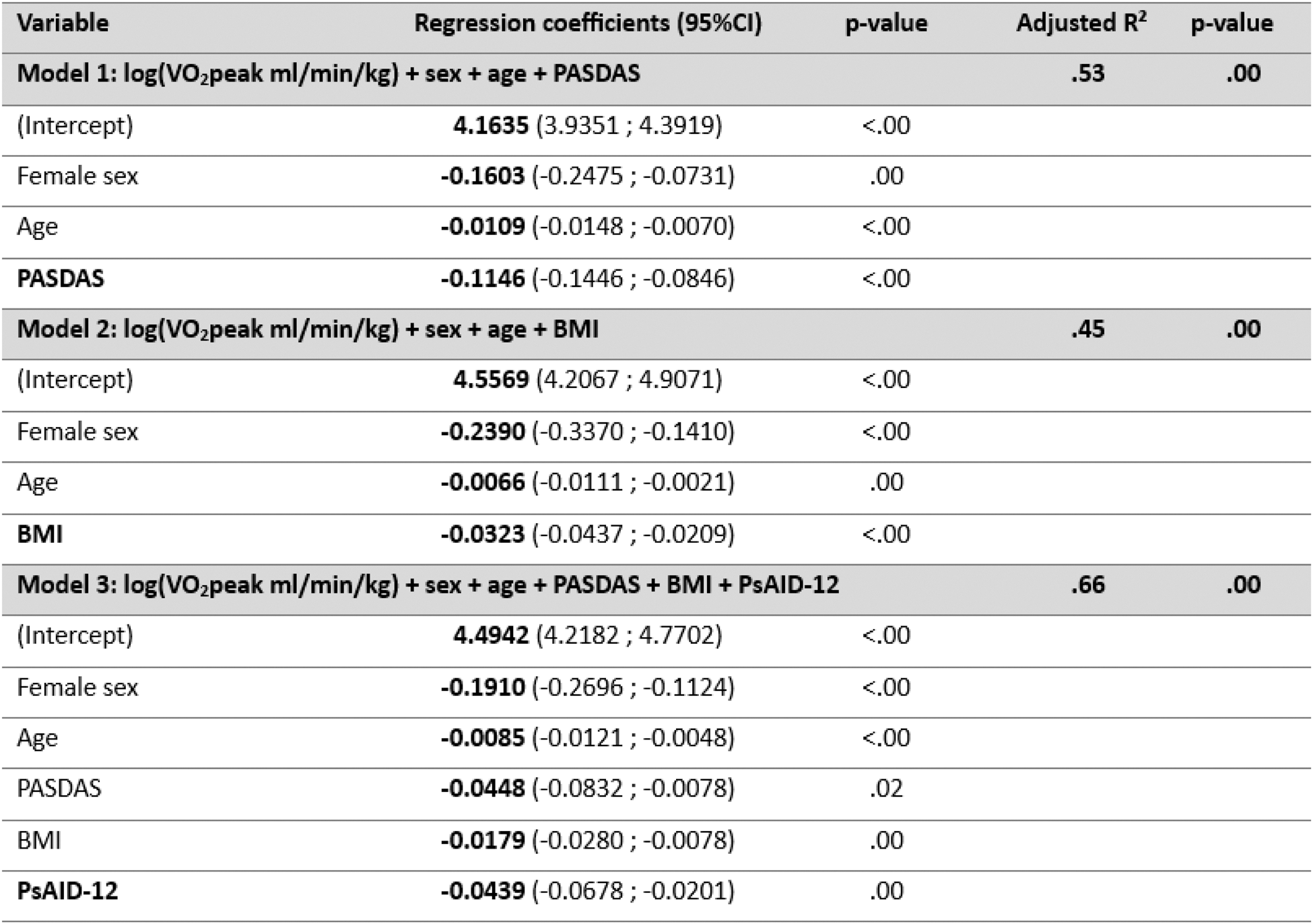
Results: Eighty patients with PsA were included. Demographic characteristics and CRF level are presented in Table 1. VO 2 peak of the patients with PsA was comparable to a sedentary reference population (median 102.00% (Q1-Q3 84.00%–116.20%), p>.05), but remarkably decreased compared to an active reference population (median 73.86% (Q1- Q3 60.99%–87.05%), p<.05). Overall, female patients presented a relatively higher CRF than male patients. An impaired CRF according to the physically active reference population was observed in 41% of the patients. The disease activity was inversely related with VO 2 peak (PASDAS r S =-0.66 p=.00; multivariable linear regression model in Table 2, p<.05). Analysis of individual disease activity components revealed a significant association of physician-reported parameters (SJC r S = -0.40 p=.00; TJC r S = -0.49 p=.00; physician global r S = -0.36 p=.00) and patient-reported parameters (patient-reported disease activity r S = -0.56 p=.00; patient-reported joint pain r S = -0.57 p=.00) as well as CRP-level (r S = -0.33 p=.00) with VO 2 peak. Disease duration, enthesitis, dactylitis, and presence of psoriasis were not associated. Regarding cardiometabolic risk parameters, a higher BMI was significantly associated with lower VO 2 peak (r S = -0.53 p=.00; multivariable linear regression model in Table 2, p<.05). When adjusted for age, sex, and BMI, lower VO 2 peak was significantly associated with lower HDL-cholesterol (r S = 0.25 p=.03), impaired HbA1c level (r S = -0.30 p=.01), the very high SCORE2 risk category (multivariable linear regression model β -0.29 (95%CI -0.56;-0.01) p=.04), and diagnosis of hypertension (r S =-0.26 p=.02) or diabetes mellitus type II (r S = -0.31 p=.01). No associations were noted for smoking, alcohol use, blood pressure, remaining cholesterol parameters, and other comorbidities. VO 2 peak, adjusted for age, sex, PASDAS, and BMI, was significantly associated with PsAID-12 (r S = -0.41 p=.00), FACIT-fatigue (r S = 0.26 p=.03), physical function (HAQ r S = -0.28 p=.01; SF-36 physical component summary r S = 0.25 p=.03; SF-36 role physical r S = 0.23 p=.04), SF-36 pain (r S = 0.23 p=.04), and SF-36 emotional wellbeing (r S = 0.24 p=.04). The most optimal regression model including sex, age, PASDAS, BMI, and PsAID-12 explained 66% of the variance in VO 2 peak (Table 2). No significant association was observed for working status and other SF-36 sub scores.
Conclusion: The CRF level of patients with PsA was significantly decreased compared to an active general population with 41% of the patients having an impaired CRF. A lower CRF level was substantially associated with impaired disease control, an unfavourable body composition and cardiometabolic risk profile, as well as with higher patient-reported disease impact. Although further research is needed to establish the causality and direction of these relations, improving CRF in patients with PsA can become a crucial target to reduce disease impact and cardiometabolic risk in PsA.
Table 1. Demographic characteristics and cardiorespiratory fitness level of included patients with PsA
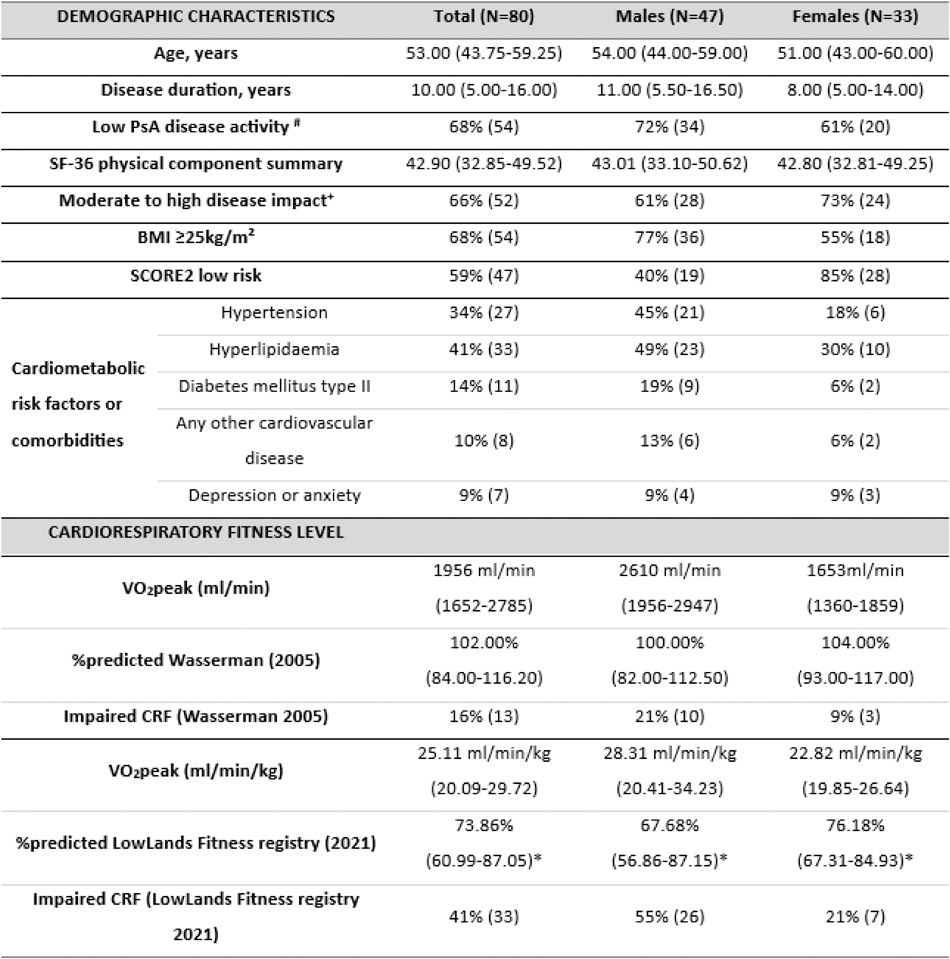
Results presented as median (Q1-Q3) or percentage (N). # PASDAS≤3.2; + PsAID12 >1.95 SCORE2: Systematic COronary Risk Estimation 2. *One-sided Wilcoxon rank-sum test: p<.05.
Table 2. Multivariable linear regression models: relation between log (VO 2 peak) and disease activity (1), cardiometabolic risk parameters (2), and PROMs (3)
REFERENCES: [1] Wasserman K. Principles of Exercise Testing and Interpretation: Including Pathophysiology and Clinical Applications: Lippincott Williams & Wilkins, 2005.
[2] van der Steeg GE, Takken T. Reference values for maximum oxygen uptake relative to body mass in Dutch/Flemish subjects aged 6-65 years: the LowLands Fitness Registry. Eur J Appl Physiol 2021;121:1189-96.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (