

Background: Optimizing physical activity (PA) in people with rheumatic and musculoskeletal diseases (RMDs) is a cornerstone of effective disease management [1]. Numerous studies have identified personal barriers to and facilitators for PA among patients with RMDs, often revealing similar determinants across different populations [2]. However, European countries differ significantly in many aspects such as healthcare systems, cultural norms, weather conditions, urban design, and income levels. It remains unclear what country-specific facilitators and barriers exist and how they differ.
Objectives: This study aimed to explore these differences and identify extra-personal barriers and facilitators for physical activity (PA), as well as potential variations, across Türkiye, Switzerland, France, and the Netherlands.
Methods: A questionnaire comprising 27 questions was developed to assess extra-personal barriers and facilitators of PA, through an extensive literature review, and interviews with multiple stakeholders, and experts in the field in four European countries. Following pre-testing, the questionnaire was distributed with the assistance of national patient organizations to people with rheumatoid arthritis, axial spondyloarthritis and osteoarthritis living in four European countries. The survey included items addressing social (7 items), environmental (13 items), and system factors (7 items), rated as facilitators (1 to 10), neutral (0), or barriers (-1 to -10). A global score was calculated for each item to enable cross-country comparisons (-10 to 10). One-way analysis of variance (ANOVA) was used to compare global scores across the four countries.
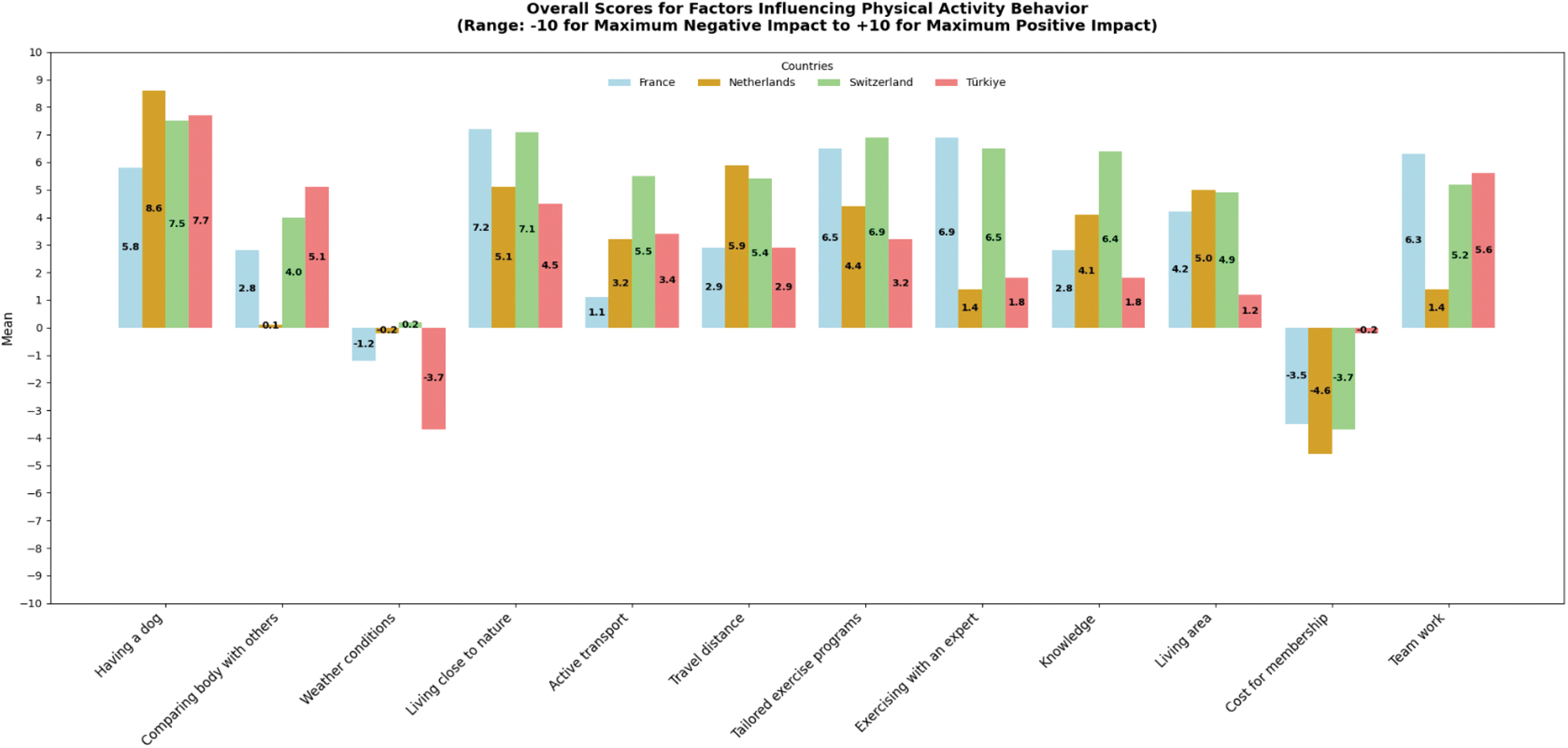
Results: A total of 602 people (France (n=224), Netherlands (n=127), Switzerland (n=129), and Türkiye (n=122)) with rheumatoid arthritis (48.2%), axial spondyloarthritis (34.1%), and osteoarthritis (17.8%) filled the questionnaire. The majority of respondents were female (79.2%) with a mean age of 57.06 years. The median weekly PA duration was 60 minutes (IQR 30;180) (Table 1). The top barriers across all patients were weather conditions (29.1%), costs for memberships to sport facilities or equipment (21.6%), and work-related duties (18.6%). The most frequently reported facilitators included scheduled exercises (57.4%), support from health professionals (52.3%), knowledge and fitness how to perform exercises or PA (52.5%), shorter travel distances to sport facilities or nature (49.0%), and living close to nature (48.5%). Cross-country comparisons revealed significant differences: weather conditions hindered PA mostly in Türkiye (p=0.003), while the cost for membership to sports facilities or equipment (p=0.017) was a greater barrier in the Netherlands. Active transport (p<0.001) and knowledge and fitness to perform exercises or PA (p<0.001) were perceived as facilitators to PA predominantly in Switzerland. People living in Türkiye considered comparing their appearance or fitness level with others (p=0.001) as a facilitator for PA. Moreover, shorter travel distances to sport facilities or nature (p=0.001) were perceived as facilitator to PA mostly in the Netherlands and health professionals working as a part of an interdisciplinary team (p<0.001) mostly among patients living in France. Additionally significant differences were observed for having a dog (p = 0.005), living close to nature (p<0.001), access to tailored exercise programs (p<0.001), guidance or supervision from experts in rheumatic diseases (p<0.001), and environmental living conditions (p<0.001) across four European countries (Figure 1).
Conclusion: This study highlights the need for tailored, country-specific interventions to address the unique barriers and facilitators influencing PA participation among patients with RMDs in different European countries. Key findings, such as the significant role of health professionals in France, the importance of active transport and knowledge in Switzerland, and the impact of cost and environmental factors in the Netherlands and Türkiye, provide valuable insights for designing effective strategies in clinical practice and future research to enhance PA engagement, improve patient outcomes and overall well-being in this population.
REFERENCES: [1] Osthoff, Anne-Kathrin Rausch, et al. “2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis.” Annals of the rheumatic diseases 77.9 (2018): 1251-1260.
[2] Metsios, George S., et al. “Barriers and facilitators for physical activity in rheumatic and musculoskeletal disease: a European-based survey.” Clinical rheumatology 42.7 (2023): 1897-1902.
Demographic characteristics of people with RMDs across four European countries
| All patients
| France
| Netherlands
| Switzerland
| Türkiye
| P | |
|---|---|---|---|---|---|---|
| Age, mean (SD) | 57.06 (12.71) | 60.72 (12.05) | 56.11 (11.71) | 55.40 (13.82) | 52.73 (11.53) | <0.001* |
| Gender, female, n (%) | 477 (79.2) | 206 (92.0) | 114 (89.8) | 64 (49.6) | 93 (76.2) | <0.001* |
| Years since diagnosis, median (IQR) | 10 (4 – 20) | 15 (6 – 26) | 8 (3 – 17.5) | 12 (4 – 24.5) | 7 (3 – 12) | <0.001 * |
| Physical activity, minutes per week, median (IQR) | 60 (30 – 180) | 60 (30 – 120) | 140 (60 – 275) | 120 (40 – 290) | 30 (0 – 92.5) | 0.003* |
| Strength training days per week | 1 (0 – 2) | 1 (0 – 2) | 1 (0 – 2) | 1 (0 – 3) | 0 (0 – 0) | <0.001* |
| Primary diagnosis, n (%) | <0.001 * | |||||
| Osteoarthritis | 107 (17.8) | 39 (17.4) | 24 (18.9) | 9 (7) | 35 (28.7) | |
| Rheumatoid Arthritis | 290 (48.2) | 147 (65.6) | 62 (48.8) | 30 (23.3) | 51 (41.8) | |
| Axial Spondyloarthritis | 205 (34.1) | 38 (17.0) | 41 (32.3) | 90 (69.8) | 36 (29.5) |
*Statistically significant
Overall Scores for Factors Influencing PA Behavior
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (