

Background: The World Health Organization (WHO) 2020 guidelines on physical activity (PA) and sedentary behavior (SB) reaffirm messages that more moderate or vigorous intensity physical activity (MVPA) is better for optimal health outcomes, that some physical activity is better than none, and now, specifically recommends reducing SB [1]. SB is defined as waking behavior characterized by an energy expenditure of ≤1.5 metabolic equivalents (e.g. laying, sitting) [2]. Although there is extensive evidence on the benefits and safety of exercise and interventions promoting PA in people with inflammatory arthritis (IA) or osteoarthritis (OA), the evidence regarding interventions that explicitly include the reduction of SB, is scarce.
Objectives: To investigate the effectiveness of interventions of SB or PA interventions aiming to reduce SB in people with IA or OA.
Methods: A systematic review and a meta-analysis (MA) were conducted related to the 2025 update of the EULAR Recommendations on physical activity in people with IA and OA. The databases Medline, CENTRAL, Embase, Web of Science, Emcare and PsycInfo were searched up to August 2024 to identify randomized controlled trials (RCTs) in adults (≥18 years) with rheumatoid arthritis (RA), spondyloarthritis (SpA) or hip/knee osteoarthritis (HOA/KOA), investigating the effects of SB or PA interventions on SB reduction. From the selected studies, the number of study participants, characteristics of the intervention and the outcomes (SB measured in minutes per day) were extracted. The time point of interest was the first assessment after the intervention period. Data on change in SD from baseline were pooled using a random-effects model (REML) presented as minutes per day. The Cochrane risk of bias assessment was applied.
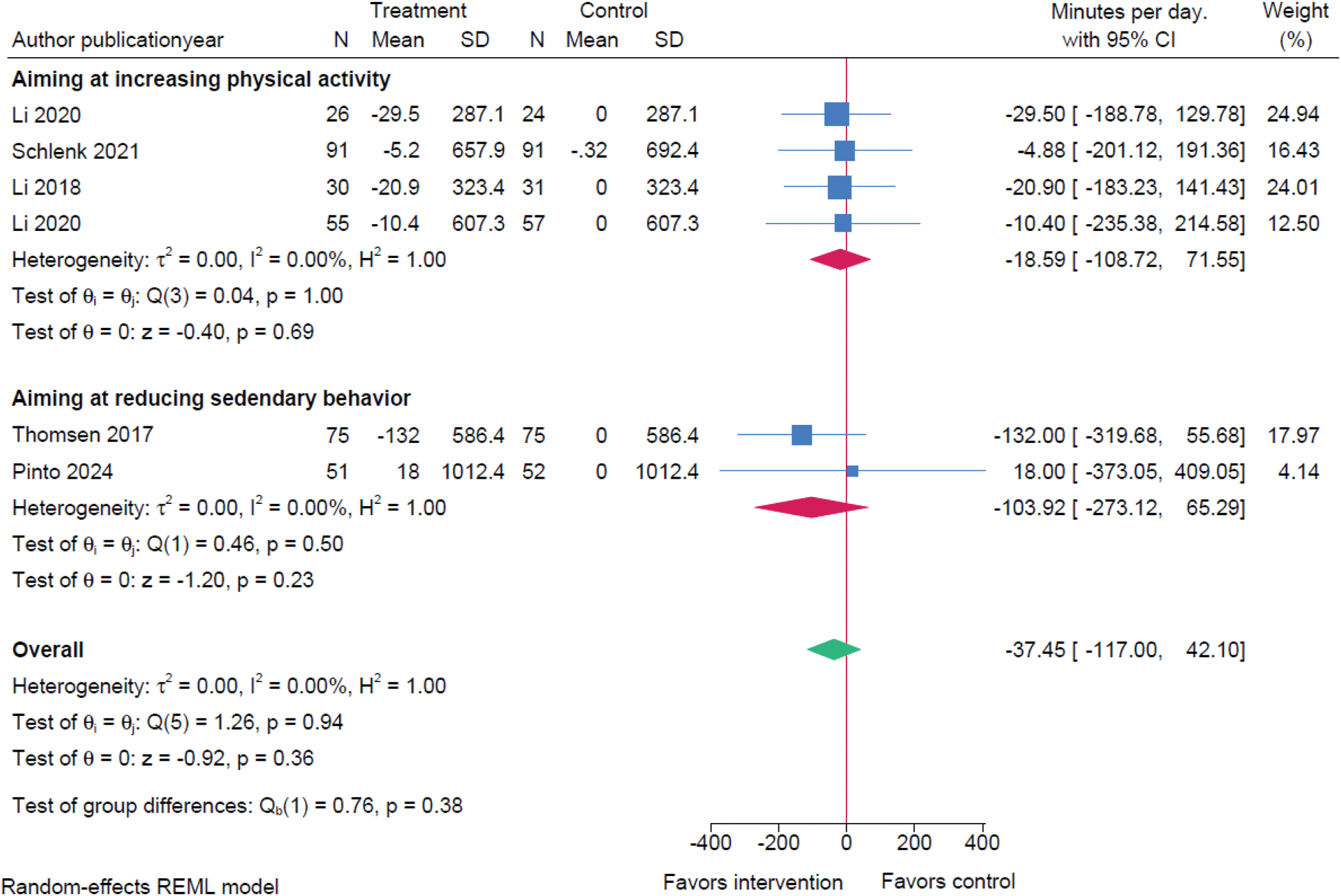
Results: Six RCTs [8-13] measuring SB as an outcome were analyzed, including a total of 294 people with OA and 371 with RA. Participants with axSpA were not included in any of the eligible studies. Two studies pertained to interventions aiming to reduce SB [12, 13], whereas four studies evaluated the effect of an intervention to increase PA participation [8-11]. Studies reported individuals as eligible if not participating in structured exercise programs [9, 13], having a sedentary lifestyle [12], or no previous use of fitness wearables [8, 11]. All interventions included counselling sessions and behavior change techniques, while participants in the control groups received either attention-control interventions or a delayed onset of the same investigated intervention. SB was measured in time using accelerometers. The overall risk of bias was appraised as moderate (Figure 1). The MA showed no effect of the studied interventions on SB (difference in change -37.45 (95%CI -117.00 to 42.10) minutes/day), neither in the studies focusing on reducing SB (difference in change -103.59 (95%CI -273.12 to 65.29) minutes/day) nor on the ones increasing PA (difference in change -18.59 (95%CI -108.72 to 71.55) minutes/day) (Figure 2).
Conclusion: Studies with interventions aiming at reducing SB specifically are scarce and the effect of interventions included in this MA seemed uncertain. More targeted studies in long-term changes of SB in people with RA and OA are needed.
Cochrane risk of bias assessment of included studies

Effect of SB or PA interventions on sedentary time in people with IA or OA.
REFERENCES: [1] Bull FC, et al; DOI: 10.1136/bjsports-2020-102955
[2] Tremblay MS, et al; DOI: 10.1186/s12966-017-0525-8
[3] Li LC, et al; DOI: 10.2196/19116
[4] Schlenk EA, et al; DOI: 10.1123/japa.2019-0498
[5] Li LC, et al; DOI: 10.2196/jmir.8514
[6] Li LC, et al; DOI: 10.1002/acr.24199
[7] Thomsen T, et al; DOI: 10.1136/annrheumdis-2016-210953
[8] Pinto AJ, et al; DOI: 10.1249/MSS.0000000000003546
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (