

Background: T cells abnormal activation plays a pivotal role in the early inflammatory stages of systemic sclerosis (SSc). Compelling evidence supports that SSc has a predominant Th2 and Th17 polarization [1, 2]. Interleukin-2-inducible T cell kinase (ITK) is a tyrosine kinase that promotes T cell activation, differentiation, and receptor signaling, Studies in knockout or gene-altered mice indicated that inactivation or deletion of ITK reduces not only Th2 pathways but also Th17 pathways, with minimal inhibition of Th1 cells [3, 4]. Soquelitinib (SQL), is a highly selective, covalent, inhibitor of ITK. In vitro studies demonstrated that SQL suppresses Th2 and Th17 cytokine production preferentially and it also inhibits in vivo growth of several murine tumors through increased tumor infiltration of normal CD8+ cells [5].
Objectives: Given the immune pathogenesis of SSc with predominant Th2 and Th17 polarization, we aimed at investigating the efficacy of SQL in two mouse models of lung fibrosis, and related pulmonary hypertension (PH), mimicking lung involvement in SSc.
Methods: SQL has been evaluated in the bleomycin-induced lung fibrosis mouse model and in the Fra-2 mouse model characterized by interstitial lung disease (ILD) and pulmonary vascular remodeling leading to PH. Two doses of the drug were investigated.
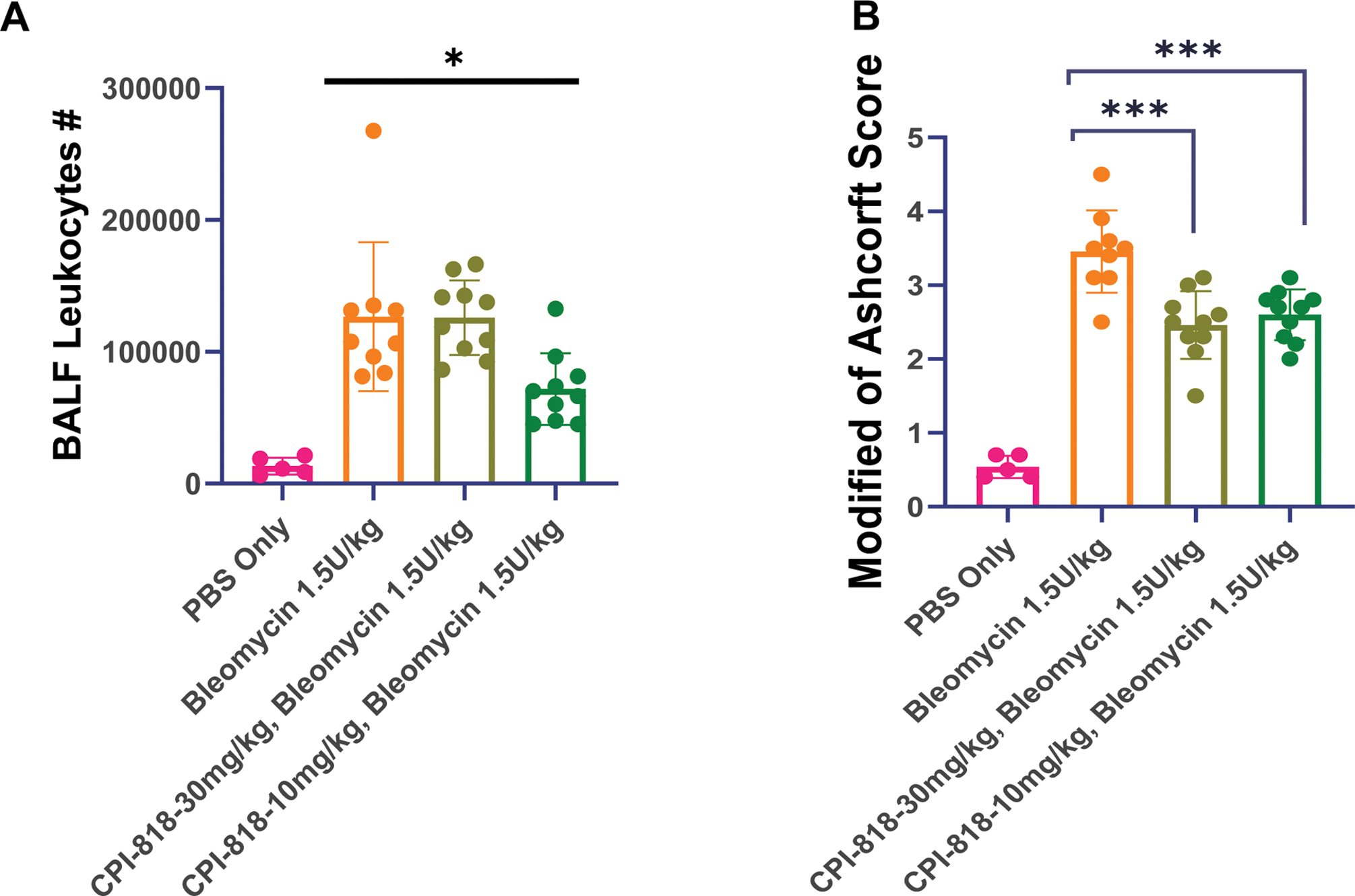
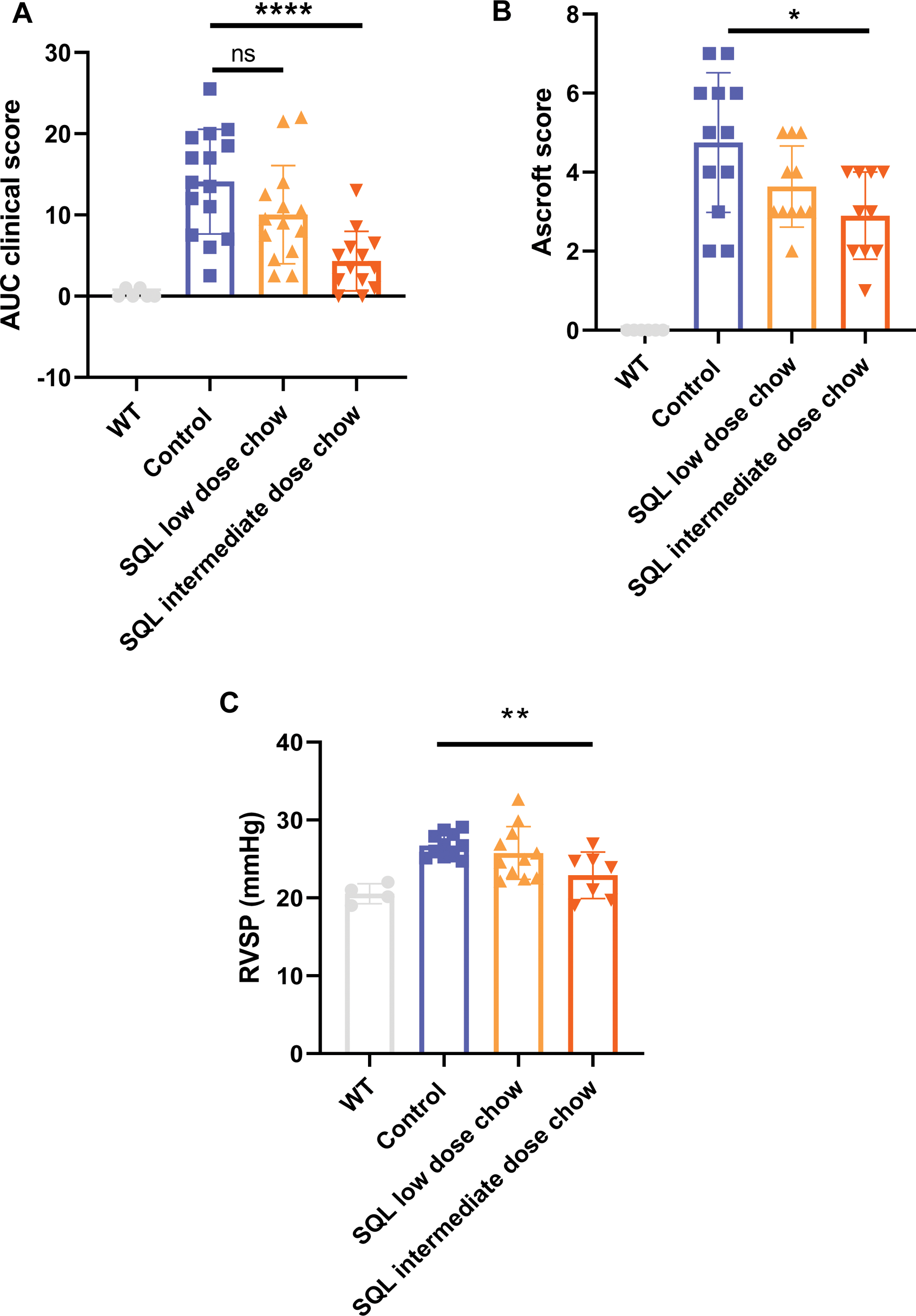
Results: In the bleomycin-induced lung fibrosis model, SQL significantly reduced the leukocytic infiltrate in the bronchoalveolar lavage fluid (p=0.013) (Figure 1A) and reduced the Ashcroft score (Figure 1B), which is indicative of structural lung damage, compared to vehicle treated mice (p<0.001). In this model, SQL reduced the expression of the major transcription factor controlling Th2 cytokine expression, GATA-3 (p=0.034), and the mRNA associated with fibrosis, MMP2 (p=0.022). In the Fra-2 model, mice treated with SQL showed better clinical outcomes (clinical score of disease manifestations) compared to untreated Fra-2 mice (p<0.0001) (Figure 2A). SQL alleviated lung fibrosis; it significantly reduced the fibrosis histological score as assessed by the Ashcroft score (p<0.05) (Figure 2B). Although there were no significant differences in lung density when assessed by chest micro-CT imaging. Cardiovascular investigations revealed a significantly reduced right ventricular systolic pressure (23.9 mmHg vs. 26.7 mmHg, p=0.004) in SQL-treated Fra-2 mice compared to untreated Fra-2 mice (Figure 2C). Investigating myocardial thickness did not reveal significant differences between SQL-treated mice and control ones. Finally, SQL reduced Th2-dependent GATA3 and Th17-dependent RORγt expression in lesional lungs of bleomycin and Fra-2 mice. A dose effect was observed in the various experiments.
Conclusion: Our findings suggest that ITK inhibition with SQL, by decreasing Th2 and Th17 activation, provides therapeutic benefits in 2 complementary models of SSc lung damage. Given the importance of T cell activation in the early stages of the disease, there is a strong rationale for the potential benefit of T cell-targeting therapy in SSc. SQL represents a promising new approach for treating lung involvement in SSc, warranting clinical trials.
Soquelitinib (SQL) treatment protected mice against bleomycin-induced lung fibrosis. (A) SQL reduced recruitment of leukocytes into the lung. Infiltrating leukocyte number collected from bronchoalveolar lavage fluid (BALF) samples is shown. (B) SQL significantly decreased lung structural damage. Modified Ashcroft scores for the severity of fibrosis are shown. Each dot in a bar graph represents one mouse. * p<0.05; *** p<0.001.
REFERENCES: [1] O’Reilly S, Hügle T, van Laar JM. T cells in systemic sclerosis: a reappraisal. Rheumatology. 2012, 51(9):1540–9.
[2] Zhou Y, Hou W, Xu K, Han D, Jiang C, Mou K, et al. The elevated expression of Th17-related cytokines and receptors is associated with skin lesion severity in early systemic sclerosis. Hum Immunol. 2015, 76(1):22–9.
[3] Prince AL, Kraus Z, Carty SA, Ng C, Yin CC, Jordan MS, et al. Development of innate CD4+ and CD8+ T cells in Itk-deficient mice is regulated by distinct pathways. J Immunol Baltim Md 1950. 2014;193(2):688–99.
[4] Deakin A, Duddy G, Wilson S, Harrison S, Latcham J, Fulleylove M, et al. Characterisation of a K390R ITK kinase dead transgenic mouse--implications for ITK as a therapeutic target. PloS One. 2014;9(9):e107490.
[5] Hsu LY, Rosenbaum JT, Verner E, Jones WB, Hill CM, Janc JW, et al. Selective Inhibition of Interleukin-2 Inducible T Cell Kinase (ITK) Enhances Anti-Tumor Immunity in Association with Th1-skewing, Cytotoxic T cell Activation, and Reduced T Cell Exhaustion [Internet]. bioRxiv; p. 2023.07.05.547822.
Soquelitinib (SQL) reduced disease in the Fra-2 model. (A) The clinical score was improved by SQL treatment compared to vehicle treated controls. (B) The Ashcroft score is improved by SQL intermediate dose and as illustrated by the representative histology. (C) The right ventricular systolic pressure (RVSP) was lowered by SQL treatment at the intermediate dose.* p<0.05, ** p<0.01, **** p<0.0001.
Acknowledgements: NIL.
Disclosure of Interests: Gonçalo Boleto: None declared, Anne Cauvet: None declared, Lih-Yun Hsu Corvus Pharmaceuticals, Corvus Pharmaceuticals, Corvus Pharmaceuticals, James T. Rosenbaum Corvus Pharmaceuticals, Corvus Pharmaceuticals, Corvus Pharmaceuticals, Richard A. Miller Corvus Pharmaceuticals, Corvus Pharmaceuticals, Corvus Pharmaceuticals, Yannick Allanore: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (