

Background: Axial spondyloarthritis (axSpA) is often associated with persistent pain despite effective anti-inflammatory treatment, substantially impacting patients’ quality of life. Digital health applications (DiGAs) provide an innovative approach to address multidimensional aspects of chronic pain through psychological and behavioral strategies.
Objectives: To assess the impact of a DiGA utilizing the acceptance and commitment therapy (ACT) on disease outcomes, including the West Haven-Yale Multidimensional Pain Inventory (MPI), in axSpA patients experiencing chronic back pain despite stable pharmacological therapy.
Methods: This unblinded, monocentric, randomized controlled trial (1:1) compared an intervention group receiving the ACT-app with a standard of care (SOC) group. The ACT app provided behavioral therapy in seven interactive lessons. Patients were followed for 12 weeks. The primary outcome was MPI pain-related life interference; secondary outcomes included pain severity, affective distress and other patient reported outcomes (PRO). Acceptance of the DiGA was assessed using the Net promoter score (NRS 0-10). Linear models estimating the effect of the ACT-app on the change of MPI pain-related life interference (model 1) and affective distress (model 2), with adjustments made for their respective baseline values, were calculated.
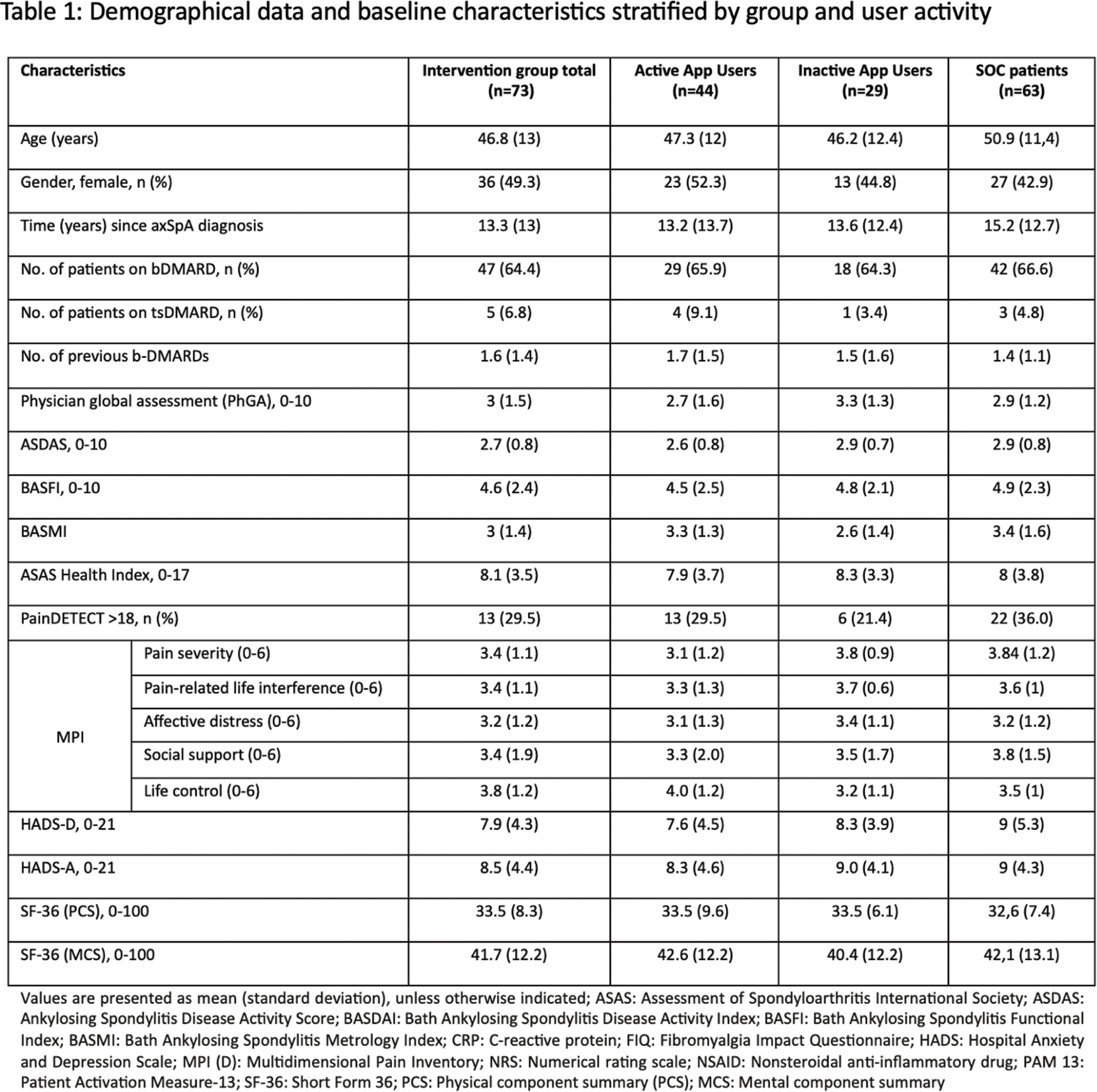
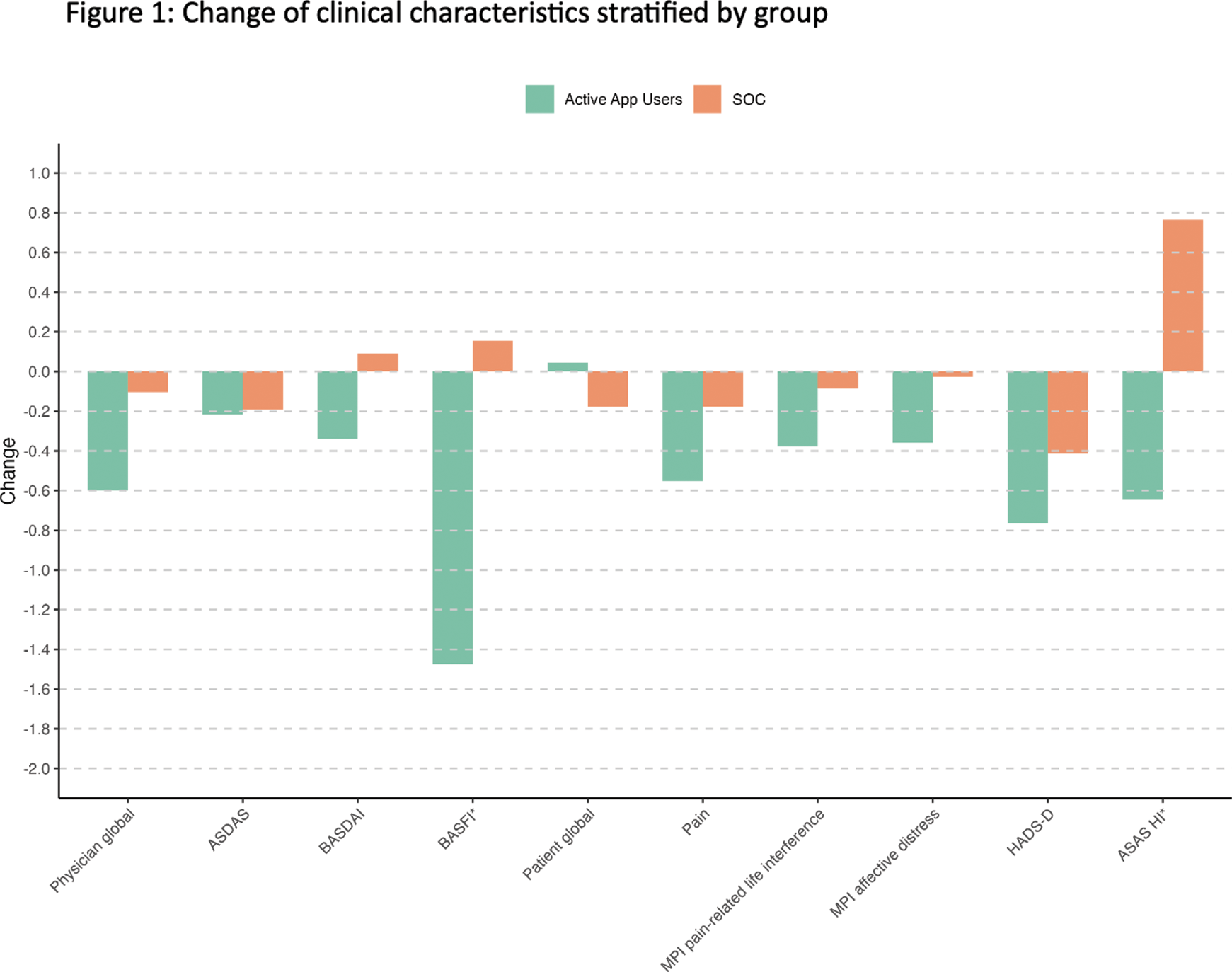
Results: A total of 136 patients were randomized to the intervention (n=73) with ACT-app and SOC group (n=63) without ACT-app (Table 1). Among intervention patients, 44 actively used ACT-app, while 29 either did not receive the app code by their health insurance company or did not use the ACT-app at all. At week 12, all lessons in the ACT-app were fully completed by 19 (43%) patients in the intervention group. Baseline characteristics, including MPI scores, were comparable between groups (Table 1). Differences in changes of the two groups are shown in Figure 1. The improvements in pain-related life interference (model1: -0.36, 95% CI: -0.73 to 0.01) and affective distress related to the disease (model 2: -0.4, 95% CI: -0.84,0.003) were greater compared to SOC patients. Overall acceptance was moderate (Net Promoter Score 5.8 (4.3)).
Conclusion: The ACT-app demonstrated a meaningful reduction in pain-related interference, supporting that the use of DIGAs might become a supplementary tool in managing pain for axSpA patients. However, a substantial number of patients experienced challenges to use the app actively.
REFERENCES: NIL.
Acknowledgements: This study was funded as part of the Research funding of the Faculty of Medicine - FoRUM program - at Ruhr-University Bochum, Germany.
Disclosure of Interests: David Kiefer: None declared, Yade Sonkaya: None declared, Dietmar Krause: None declared, Markus Voglau Abbvie, Pfizer, Novartis, Bernhard Mintrop: None declared, Imke Redeker: None declared, Xenofon Baraliakos: None declared, Uta Kiltz: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (