

Background: Axial spondyloarthritis (axSpA) is a chronic inflammatory condition primarily affecting the sacroiliac joints (SIJ) and the spine, leading to significant disability if left untreated. Early detection and intervention are crucial to prevent disease progression and improve patient outcomes. Magnetic resonance imaging (MRI) is the most sensitive imaging modality for identifying active sacroiliitis, a key feature of axSpA, as it can detect subchondral bone marrow edema (BME) before structural changes become evident. Despite standardized diagnostic criteria such as the ASAS definition of active sacroiliitis, interpretation of SIJ MRI is prone to variability even among experienced radiologists and rheumatologists. Recent advances in artificial intelligence and machine learning have demonstrated potential in improving diagnostic accuracy and efficiency, particularly for identifying inflammation-related patterns.
Objectives: This study aims to develop a deep learning model using the YOLOv7 (You Only Look Once version 7) algorithm to detect bone marrow edema on SIJ MRI scans and evaluate its performance in classifying active sacroiliitis according to the ASAS criteria. By utilizing automated image analysis, this research seeks to enhance the accuracy and consistency of MRI interpretation in patients with suspected axSpA.
Methods: This retrospective study included 124 patients who underwent SIJ MRI at our hospital between January 2020 and January 2025. The cohort was divided into three groups: 50 patients diagnosed with axSpA based on clinical and imaging findings, 50 patients without axSpA as the normal control group, and 24 patients used for independent testing of the model. All MRIs were performed using 1.5 Tesla scanner with a slice thickness of 3 mm, including fluid-sensitive sequences such as short tau inversion recovery (STIR) and T1-weighted images with fat suppression to assess for BME. The semi-coronal STIR images were exported in Portable Network Graphics format for further analysis. The ASAS definition of active sacroiliitis (the presence of at least two BME lesions on a single image slice or the detection of BME on at least two consecutive image slices) served as the gold standard for evaluating MRI findings. The dataset was annotated by a rheumatologist using Python’s labelImg.py tool to label regions of interest corresponding to subchondral BME as well as normal areas on SIJ MRI scans. These annotations served as ground truth for training the deep learning model. Data preprocessing included data augmentation techniques, such as adjustments to sharpness, brightness, blur, contrast, and the application of CLAHE, to enhance the diversity of the training and validation datasets. The training and test datasets were divided based on subjects rather than individual MR slices, and the dataset was split into training and validation in an 80:20 ratio. A test set of the same size as the validation set was created using images not included in the training or validation datasets. The YOLOv7 algorithm, a state-of-the-art object detection model, was employed to detect BME indicative of active sacroiliitis. This deep learning approach is designed for real-time object detection. Unlike traditional methods, which involve complex multi-step pipelines, YOLO reframes the task as a single regression problem. It divides the input image into a grid, with each cell responsible for predicting bounding boxes, confidence scores, and class probabilities. (doi.org: 10.48550/arXiv.1506.02640).
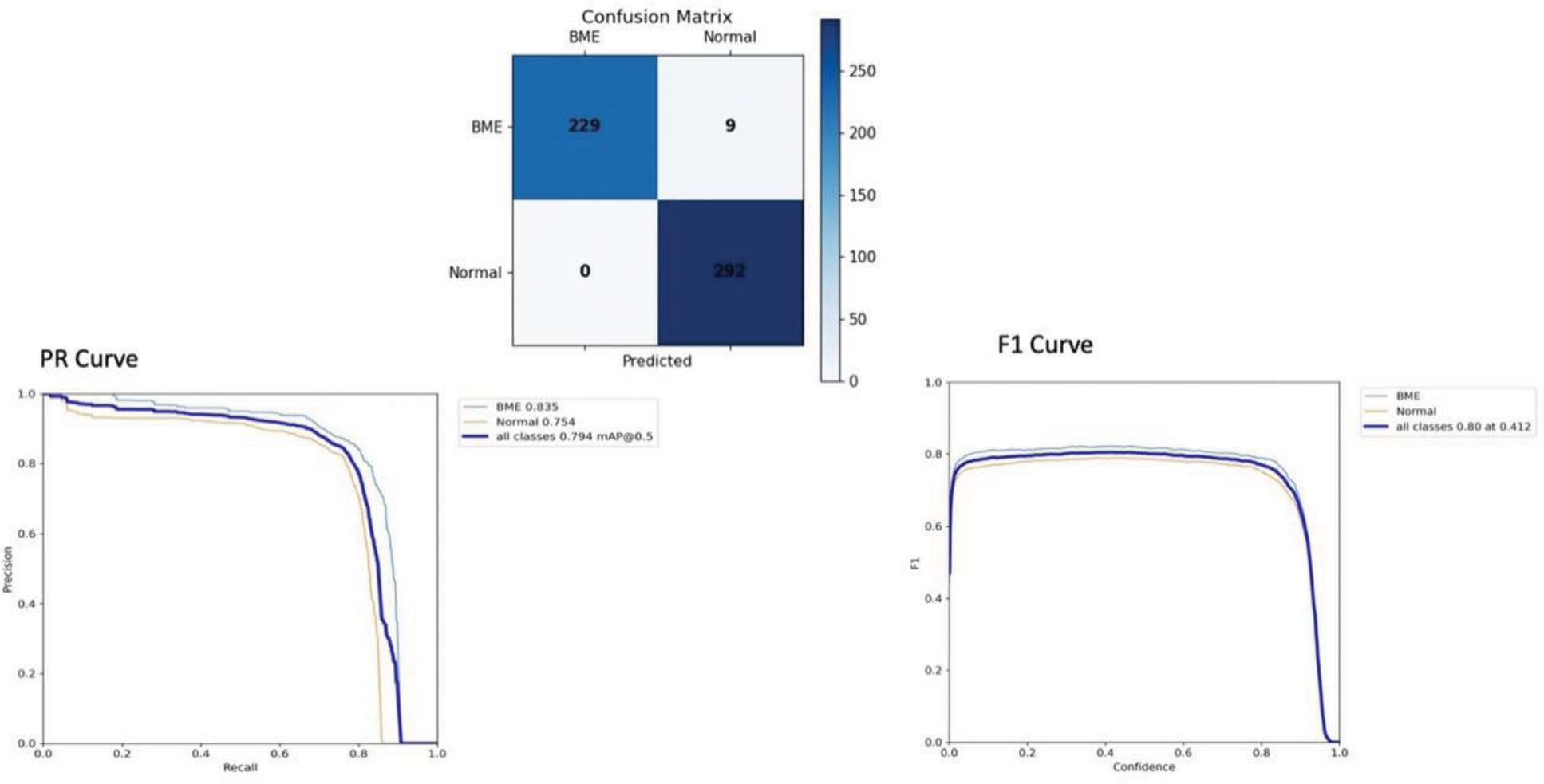
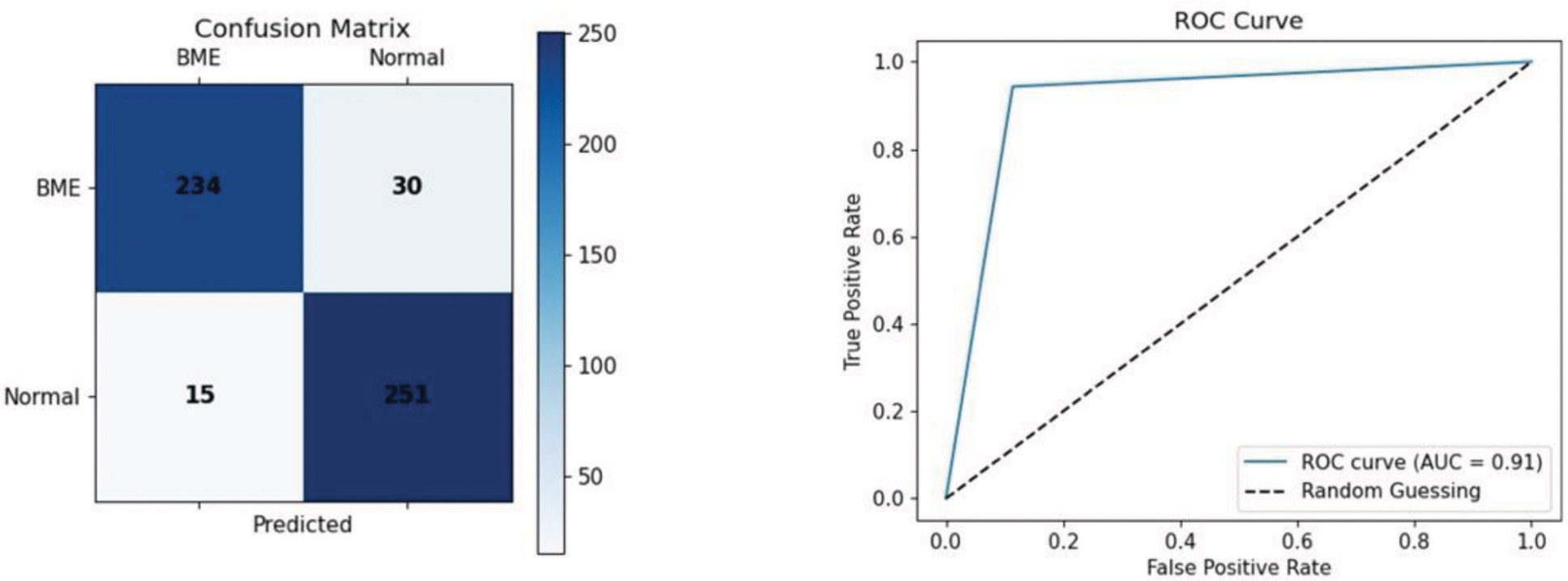
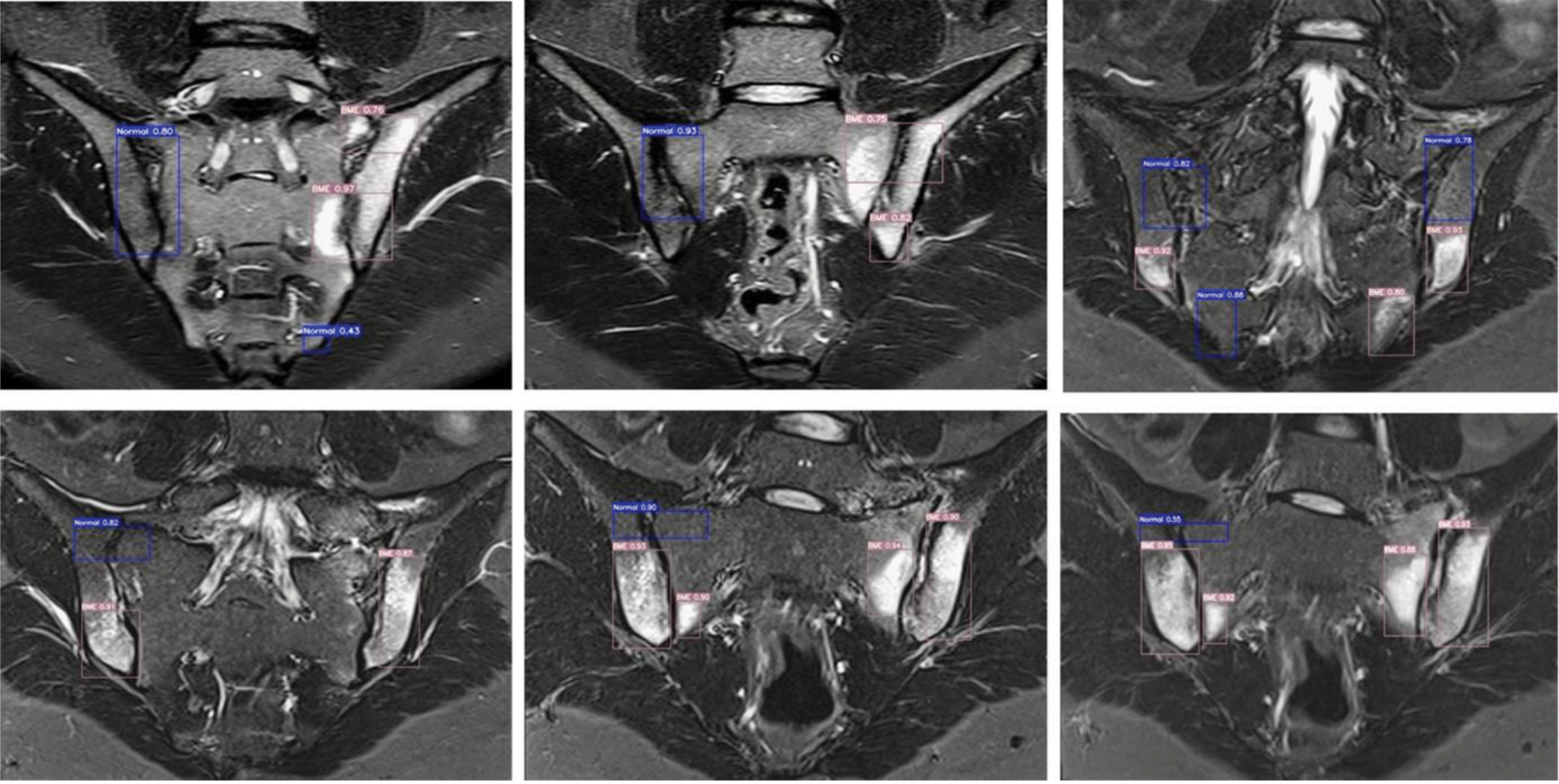
Results: The study cohort included patients with an average age of 35.05 years (Standard deviation: 7.6). There was no statistically significant difference in age or gender distribution between the SpA and normal groups (p=0.05). The original dataset consisted of 1,592 training, 530 validation, and 530 test MRI images. After applying data augmentation techniques, the dataset expanded to 3,174 training, 1,060 validation, and 530 test images. The YOLOv7 deep learning model was evaluated for detecting BME on SIJ MRI scans. In object detection tests on train and validation sets, the model achieved an accuracy of 98.3%, with a recall of 100%, a precision of 96.2%, and an F1 score of 0.80 at a confidence threshold of 0.412. PR curves showed an AUC of 0.835 for BME and 0.754 for normal cases, with a mean average precision of 0.794 (Figure 1a). For the independent sacroiliitis classification test, the model correctly classified 21 out of 24 cases (87.5% accuracy). Based on confusion matrix analysis, it demonstrated an overall accuracy of 91.6%, a recall of 94.0%, a precision of 88.6%, and an AUC-ROC of 0.91, supporting its robust performance in sacroiliitis classification (Figure 1b). Examples of the model’s test results are shown in Figure 2.
Conclusion: These results demonstrate the model’s ability to classify MRI findings based on the presence or absence of BME and its potential to support the ASAS criteria for diagnosing active sacroiliitis. YOLOv7, an object detection algorithm, offers advantages over segmentation approaches like U-Net, particularly in speed and usability. Its faster processing and high accuracy make it a practical option for real-time clinical applications. This study suggests that object detection models like YOLO could serve as reliable and efficient tools for analyzing SIJ MRIs in suspected axSpA. However, given the limited sample size of this study, further research with larger and more diverse datasets is planned to validate and generalize these findings.
REFERENCES: NIL.
Object detection test on train and validation sets.
Independent sacroiliitis classification test.
Examples of object detection and classification tests. The numbers represent the probability scores assigned to each classification decision.
Acknowledgements: The authors express their gratitude to Onurcan Koken for his invaluable contributions to this work.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (