

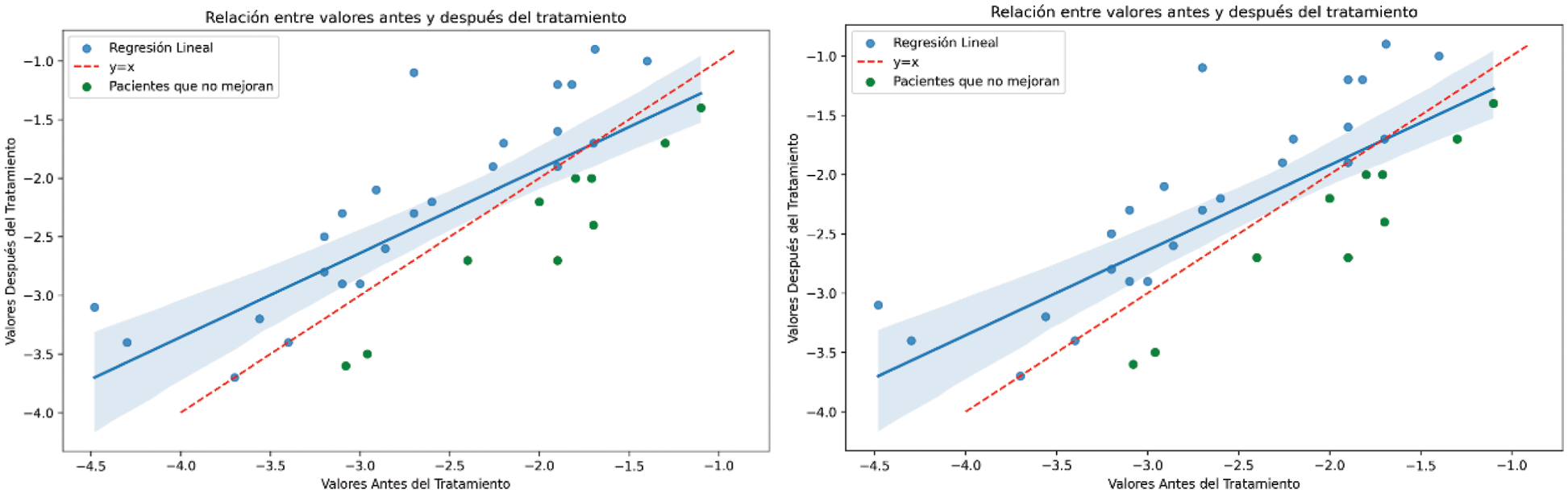
Background: Romosozumab is a drug with a dual mechanism of action on bone remodeling, increasing bone matrix production and decreasing bone resorption. Numerous studies statistically demonstrate the efficacy of the treatment in patients with severe osteoporosis and/or high fracture risk. However, in a very small number of patients, bone mineral density (BMD) levels worsen (Figure 1). In this study, we aim to elucidate which factors and models may explain this worsening.
Objectives: Analyze cofactors and imbalanced machine learning models to explain cases of patients in whom total hip and femoral neck BMD levels do not improve after one year of treatment with romosozumab.
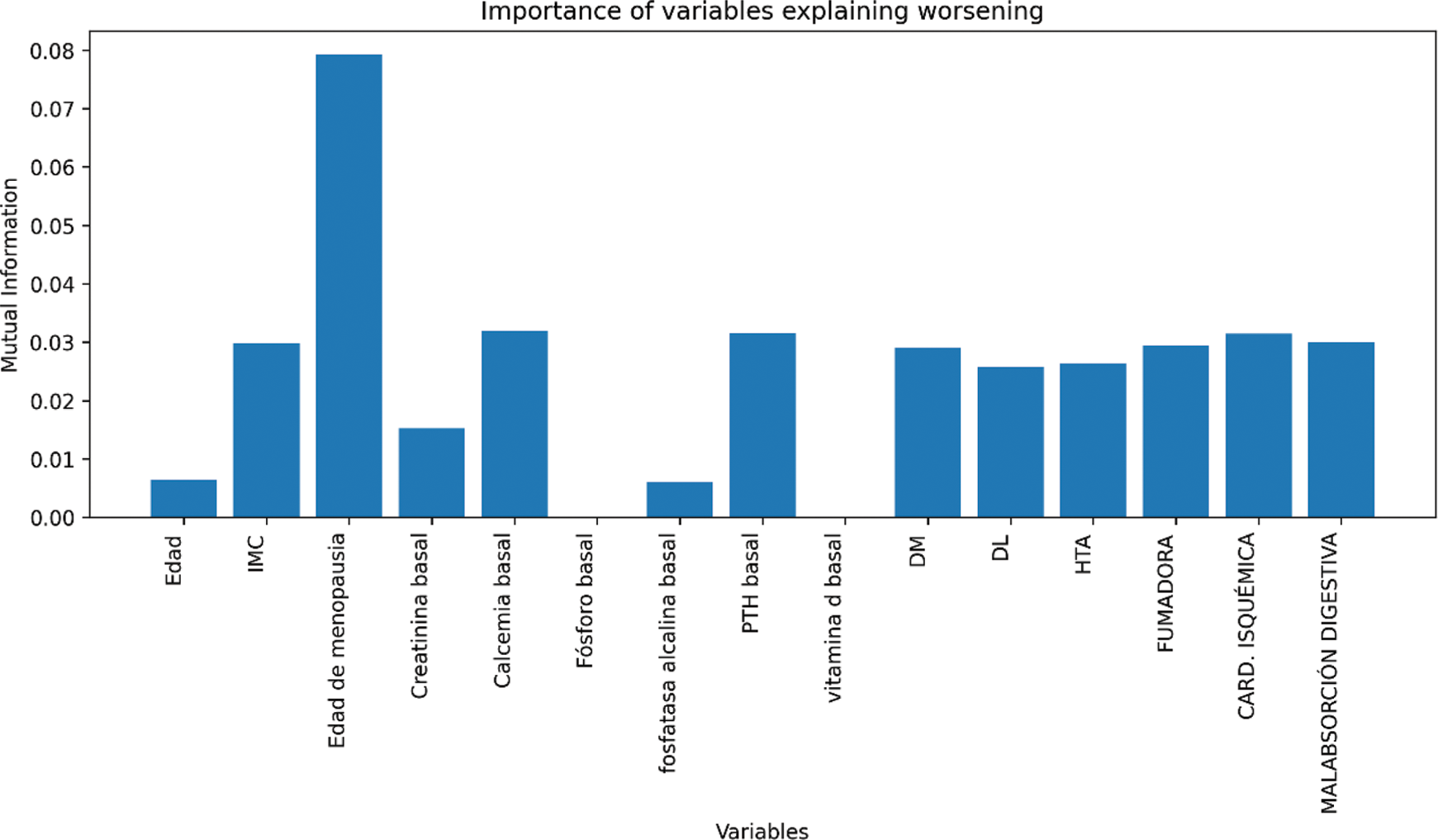
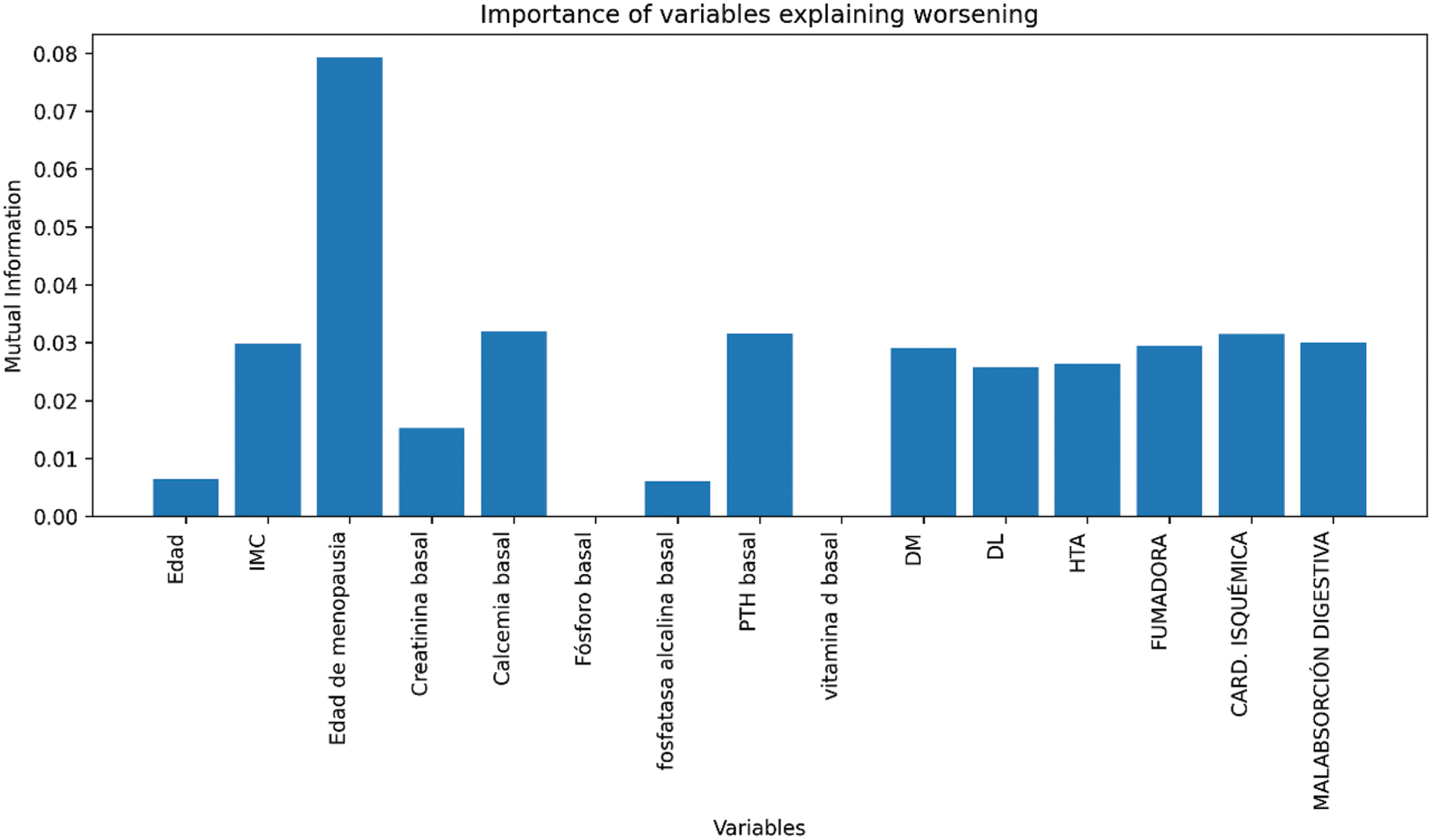
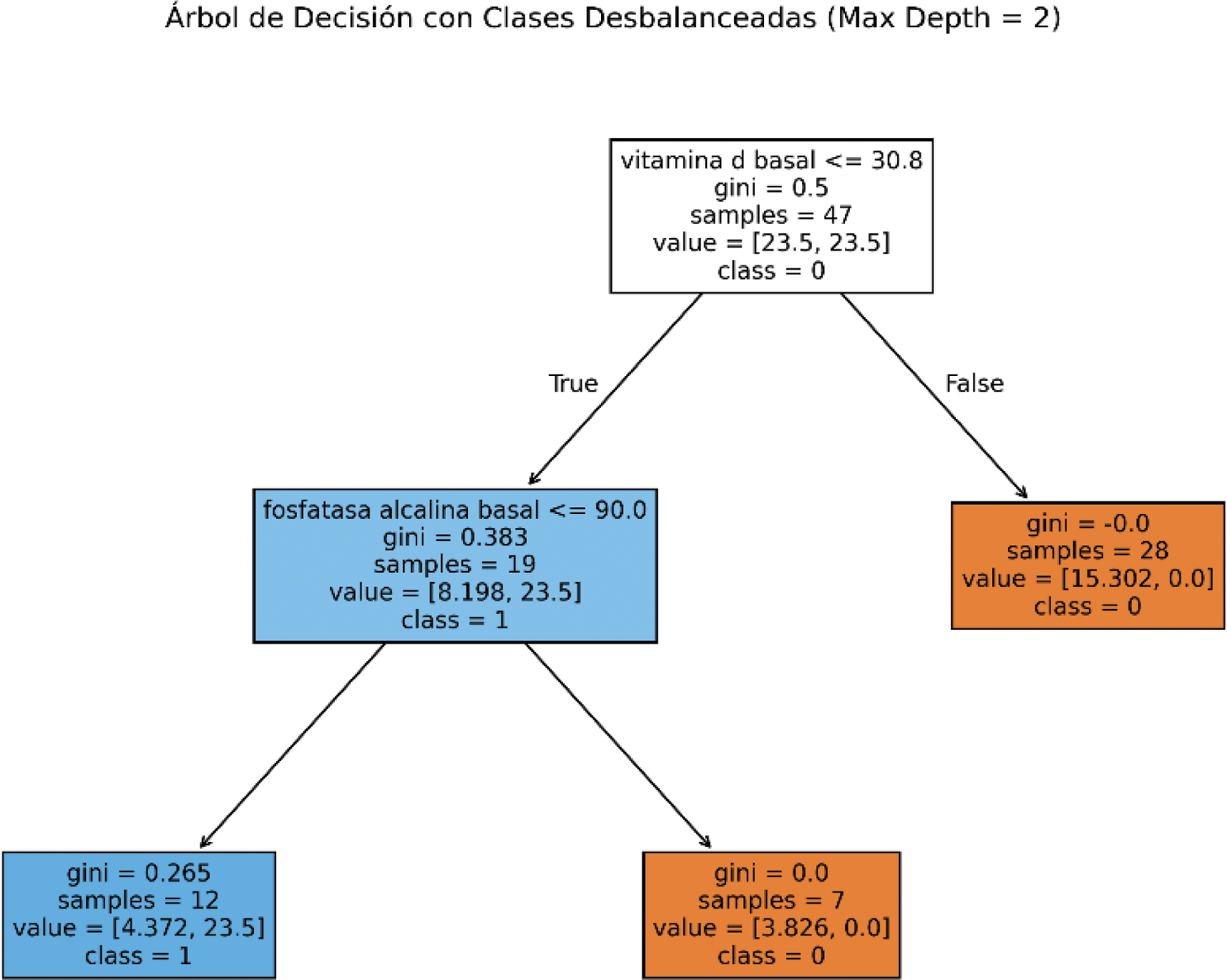
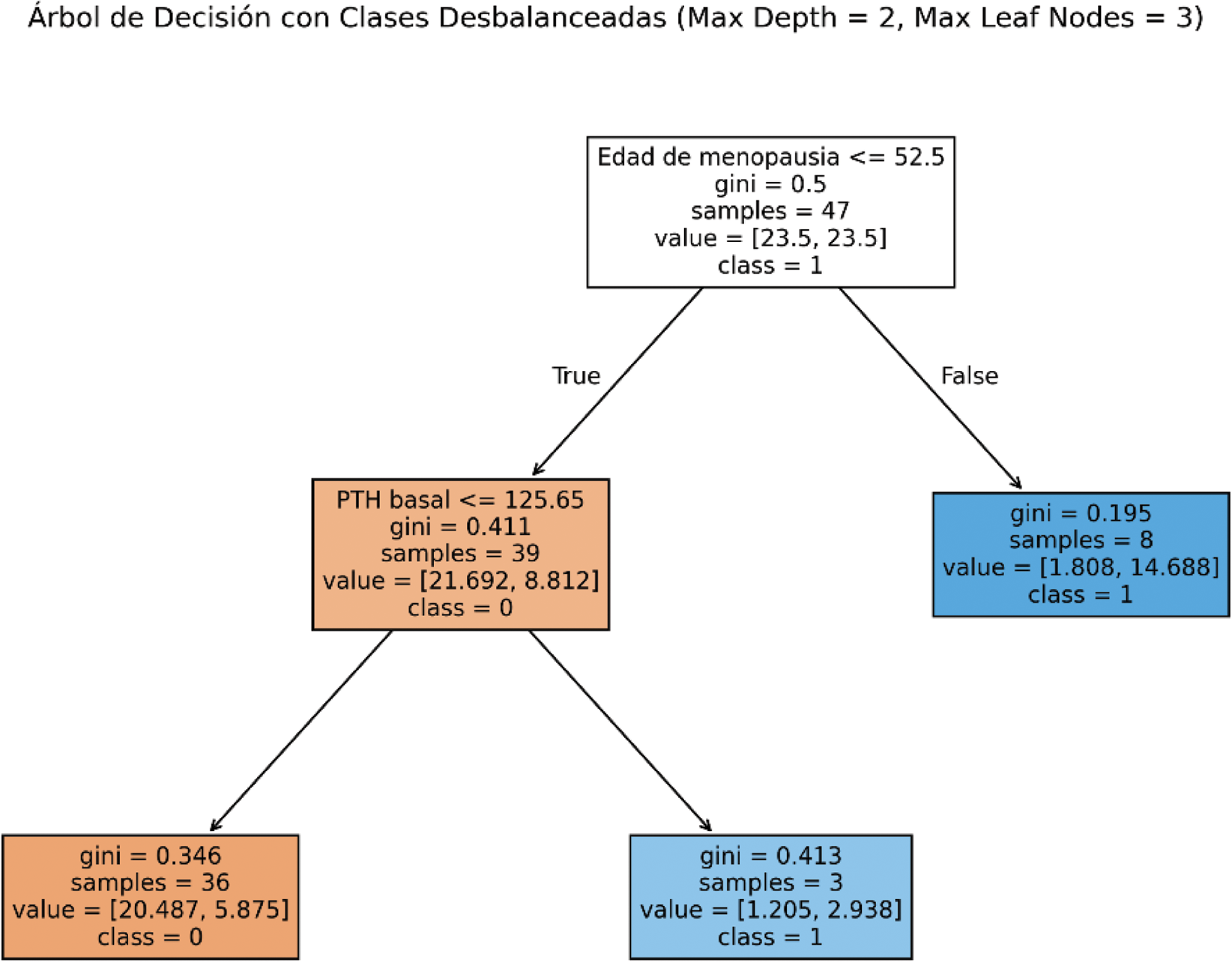
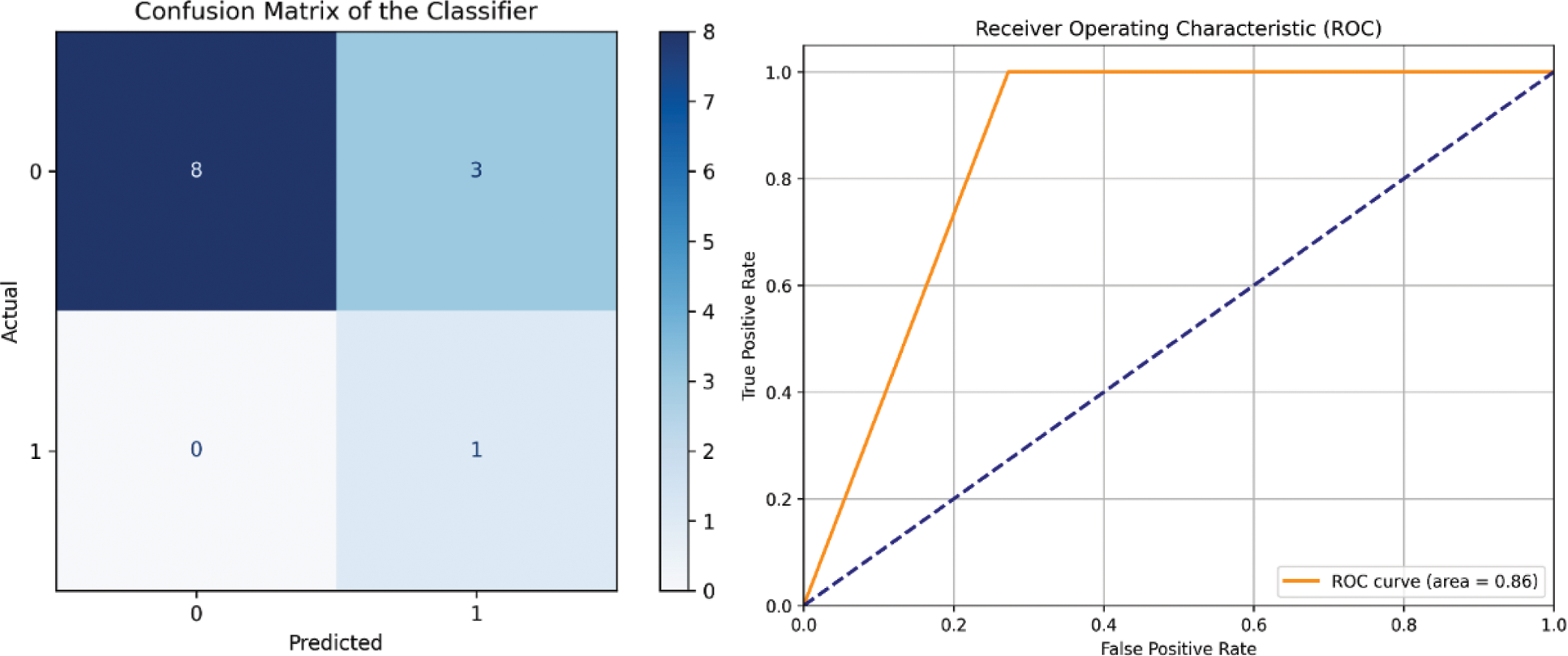
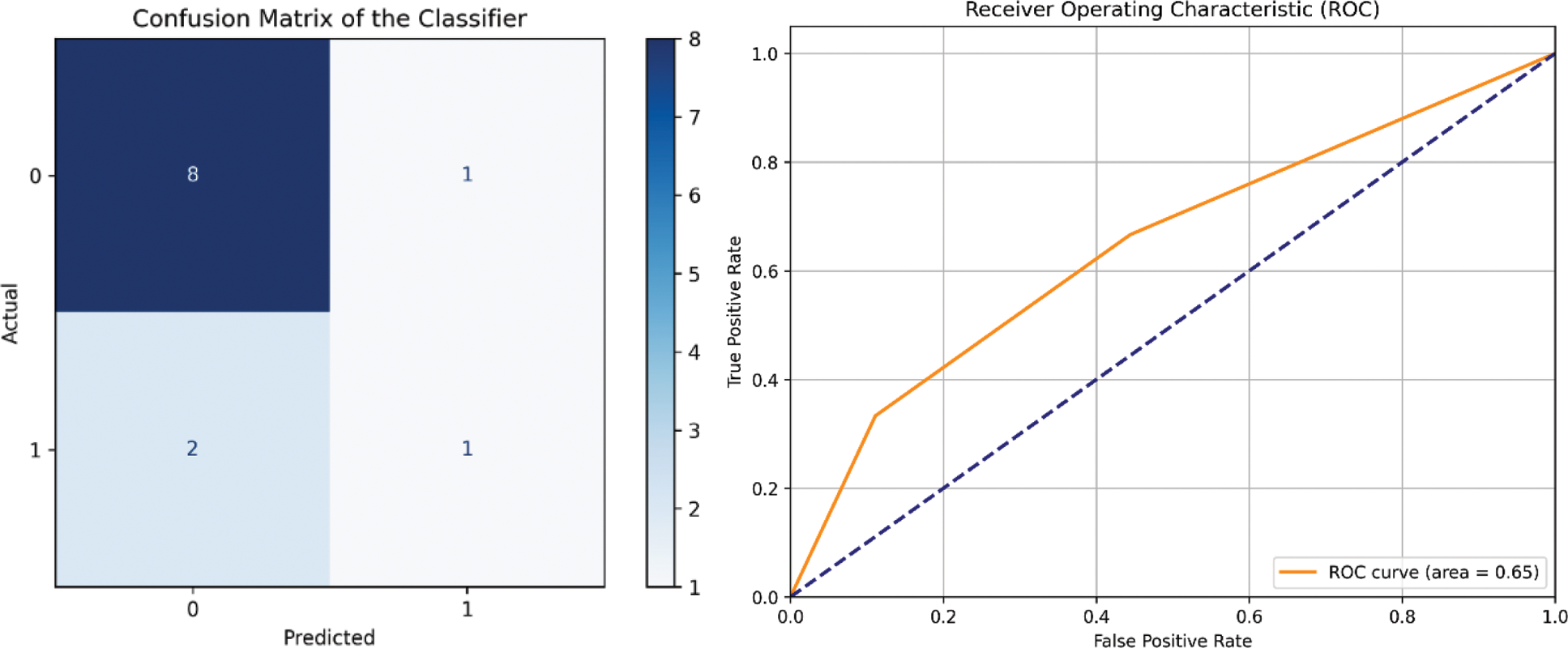
Methods: A multicenter, multidisciplinary study involving the Rheumatology and Endocrinology departments of different hospitals in Castilla-La Mancha. This is an observational, retrospective cohort study evaluating patients from May 2023 to November 2024. Data on BMD levels (T-Score) and analytical results of the mineral and bone metabolism profile were collected. First, patients whose BMD levels in the total hip and femoral neck did not improve were identified (Figure 1). Subsequently, a mutual information analysis (Figure 2) was performed with 1000 repetitions to increase robustness, aiming to identify the most important cofactors in this loss of efficacy. Using these cofactors, an explicit decision tree (Figure 3) was constructed, and its performance was assessed with a confusion matrix (Figure 4).
Results: Sixty patients were included, with a mean age of 71.8 years (± 9.28). In the linear regression for total hip, we observed that five patients, equally distributed across all levels, worsened despite receiving treatment for 12 months. Regarding the linear regression for femoral neck, it was noted that the medication was less effective in patients with higher baseline BMD levels, leading to worsening of densitometry in certain analyzed patients (Figure 1). The variables that most influenced this loss of efficacy in total hip were baseline vitamin D, baseline alkaline phosphatase, and comorbidities such as hypertension. For femoral neck, the age at menopause was the most significant factor in the absence of response to romosozumab (Figures 2 and 3). The decision tree model is interpreted by understanding that if the aforementioned cofactors were low and/or present, the treatment efficacy was reduced (Figures 4 and 5). The confusion matrix and ROC curve for this tree show that this model has a high accuracy rate for both efficacy and non-efficacy outcomes (Figures 6 and 7).
Conclusion: Although romosozumab is a drug that significantly increases BMD in patients with osteoporosis, there is a small number of cases where this gain does not occur. In our study, we have identified that low levels of vitamin D and baseline alkaline phosphatase, along with cofactors such as hypertension, influence the lack of improvement in total hip BMD. The age of menopause is the most important factor in the worsening of BMD in the femoral neck.
REFERENCES: [1] Singh S, Dutta S, Khasbage S, Kumar T, Sachin J, Sharma J, Varthya SB. A systematic review and meta-analysis of efficacy and safety of Romosozumab in postmenopausal osteoporosis. Osteoporos Int. 2022 Jan;33(1):1-12. doi: 10.1007/s00198-021-06095-y. Epub 2021 Aug 25. PMID: 34432115; PMCID: PMC9003152.
[2] Mäkinen VN, Sølling AS, McClung M, Langdahl BL. Romosozumab for the treatment of osteoporosis - a systematic review. J Endocrinol Invest. 2024 Nov 2. doi: 10.1007/s40618-024-02469-1. Epub ahead of print. PMID: 39487940.
Linear regression model of bone densitometries of the femoral neck (left) and total hip (right), at baseline and after 12 months of treatment.
Mutual information of the most relevant cofactors in the lack of efficacy of romosozumab on total hip BMD.
Mutual information of the most relevant cofactors in the lack of efficacy of romosozumab on femoral neck BMD.
Decision tree of the cofactors selected by mutual information for total hip.
Decision tree of the cofactors selected by mutual information for femoral neck.
Confusion matrix and ROC curve of the decision tree for our total hip model.
Confusion matrix and ROC curve of the decision tree for our femoral neck model.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (