

Background: AxSpA is a chronic inflammatory condition primarily affecting the sacroiliac joints and spine impacting trunk strength and mobility but also cardiorespiratory fitness [1]. Although exercise is considered as a pilar of treatment [2], there is paucity of research examining the effect of an exercise program incorporating training for trunk strength/mobility in combination with cardiorespiratory fitness.
Objectives: The aim of this prospective interventional study was to assess the potential benefits for axSpA patients of a combined cardiorespiratory and trunk strength/mobility exercise program, based on individual baseline physical test results.
Methods: AxSpA patients fulfilling the ASAS classification criteria performed a baseline maximal Cardiopulmonary Exercise Test (CPET) and trunk strength/mobility tests on the David Back Concept (DBC) devices. For strength and mobility deficits were calculated as (Reference value – Patient value) x100/ Reference value). Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and Bath Ankylosing Spondylitis Functional Index (BASFI) were collected pre and post intervention. In addition, the Tampa scale for kinesiophobia (TSK) and the modified Short QUestionnaire to ASsess Health enhancing physical activity (mSQUASH) questionnaire were evaluated at baseline as well. The Bath Ankylosing Spondylitis Metrology Index (BASMI) as well as the chest expansion (CE) was measured pre and post intervention. Subsequently, patients participated in an eight-week exercise program, with two sessions per week. Each session entailed two intervals of ten minutes of cardiorespiratory training at a set heartrate (HR), followed by exercises on the DBC devices. Training thresholds were determined based on their individual test results. The intensity for the cardiorespiratory training was monitored by HR, based on their first ventilatory threshold (VT1), using a Polar device. The three sets of repetitions of exercises on the four DBC devices focused on mobility and resistance training for the trunk and were tailored to progressively enhance strength and endurance throughout the intervention period. The program was individualized based on the ‘one repetition maximum’ and the maximal range of motion at baseline. During all training sessions, supervision and assistance was provided to make sure participants performed the exercises correctly, while ensuring safety and effectiveness. Finally, after the intervention period participants performed again a maximal CPET and trunk mobility and strength tests on DBC devices. Linear mixed models were used to examine the effect over time.
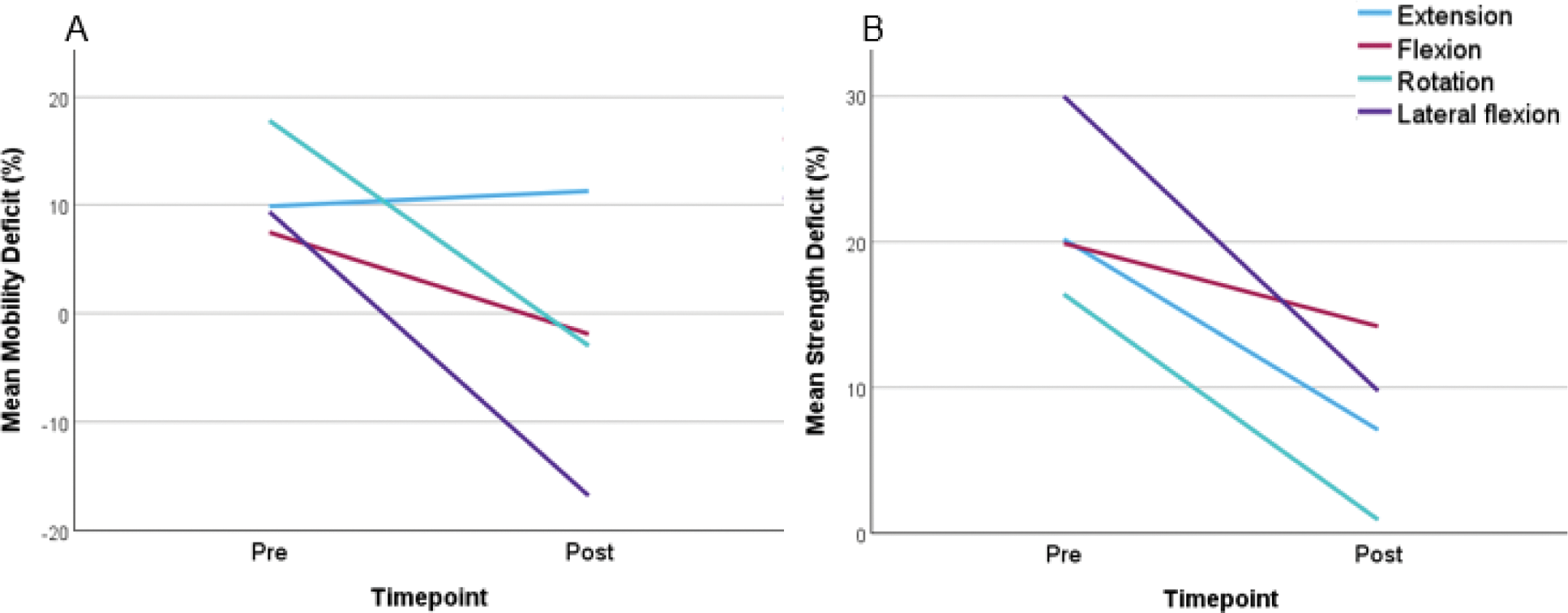
Results: 30 axSpA patients (14 M/16 F, 42±11,2 years, BASDAI 3.5±2.1, BASFI 2.8±2.2 BASMI 2.0±1.1, CE 4.5±2.0cm) participated. The mean score for the TSK was 39.13 (range 28-49), with 16 patients scoring above 37 indicating kinesiophobia. The activity score of the mSQUASH ranged between 1425 and 16 680 with an average of 8460, with a higher score indicating a higher physical activity level. Two patients were lost to follow-up and did not attend the posttest (1: flare, 2: personal reasons). Significant improvement was observed for both strength and mobility (Figure 1). A significant effect was observed for time (p<0.001) on strength with a mean decrease in deficit of 14.1% after the training program. For mobility, the interaction between time and direction and the main effects of time and direction were all significant (all p<0.001) with a mean decrease in mobility deficit of 14.9%.
Mean mobility (A) and strength (B) deficits before and after the training program for the different directions measured by the David Back Concept Devices.
Regarding cardiorespiratory parameters, a significant effect of time was shown for oxygen pulse (p=0.004), ventilatory efficiency (p<0.001), anaerobic threshold (p=0.002) and mechanical efficiency (p=0.021). No effect of time could be determined for mechanical efficiency slope (p=0.888) (Table 1).
Deficit = (Reference value – Patient value) x100/ Reference value
Cardiorespiratory parameters before and after the training program
| Pre | Post | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| anaerobic threshold, % | 58.1 | 17.7 | 72.2 | 21.6 |
| (VO2VT1/VO2pred) | ||||
| oxygen pulse, % | 12.9 | 3.5 | 14.4 | 3.4 |
| (VO2/HR) | ||||
| ventilatory efficiency | 24.7 | 2.5 | 26.4 | 2.5 |
| (VE/VCO2) | ||||
| respiratory condition, % | 94.8 | 22.2 | 103 | 25.7 |
| (PeakVO2/VO2pred) | ||||
| mechanical efficiency | 25.9 | 3.5 | 25.5 | 13.6 |
| (T2VE-T1VE)/(T2VCO2-T1VCO2) | ||||
SD: standard deviation, VO 2: rate of oxygen consumption, VT: ventilatory threshold, pred: predicted, HR: heartrate, VE: minute ventilation, VCO 2 : carbon dioxide production
In addition, we found a significant decrease in BASDAI after the training program (2.9±2.2, p=0.021), as for BASFI (2.4±2.1, p=0.092). A borderline significant decrease could be shown for the BASMI (1.8±1.0, p=0.053) and a significant increase was observed on chest expansion (5.0±2.1cm, p=0.020).
Conclusion: This is the first study evaluating an exercise program in axSpA patients using a standardized yet individually adjusted protocol to train trunk strength/mobility and cardiorespiratory endurance. We found that cardiorespiratory endurance, trunk strength and mobility were significantly improved when combining these in one exercise program, tailored to the individual. These findings underline the importance of individualized exercise interventions in axSpA management to improve patient’s outcomes and reduce functional limitations.
REFERENCES: [1] De Mits S, et al. Maximal Exercise Tolerance, Objective Trunk Strength, and Mobility Measurements in Axial Spondyloarthritis. J Rheumatol. 2024 Jun 1;51(6):596-602.
[2] Ramiro S, et al. ASAS-EULAR recommendations for the management of axial spondyloarthritis: 2022 update. Ann Rheum Dis. 2023 Jan;82(1):19-34.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (