

Background: Juvenile arthritis (JA) is the most common pediatric rheumatic disease worldwide. It is characterized by joint pain, stiffness, and decreased mobility, which can impact daily activities and participation in physical activity (PA). The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) recommend that children engage in at least 60 minutes of PA daily. Regular PA during childhood has well-documented benefits, including improved muscular fitness, cardiovascular health, cognitive function, and behavioral outcomes. While research in PA level and JIA has been conducted in European countries like Germany and The Netherlands, limited data exists in the United States (U.S.) regarding PA levels among children with arthritis. It remains unclear whether children with arthritis in the U.S. meet PA guidelines or how achieving these recommendations impacts their overall health and quality of life.
Objectives: Our aim was to investigate if having a current diagnosis of arthritis during childhood and adolescence is associated with lower PA levels among a nationally representative sample of pediatric population living in the United States.
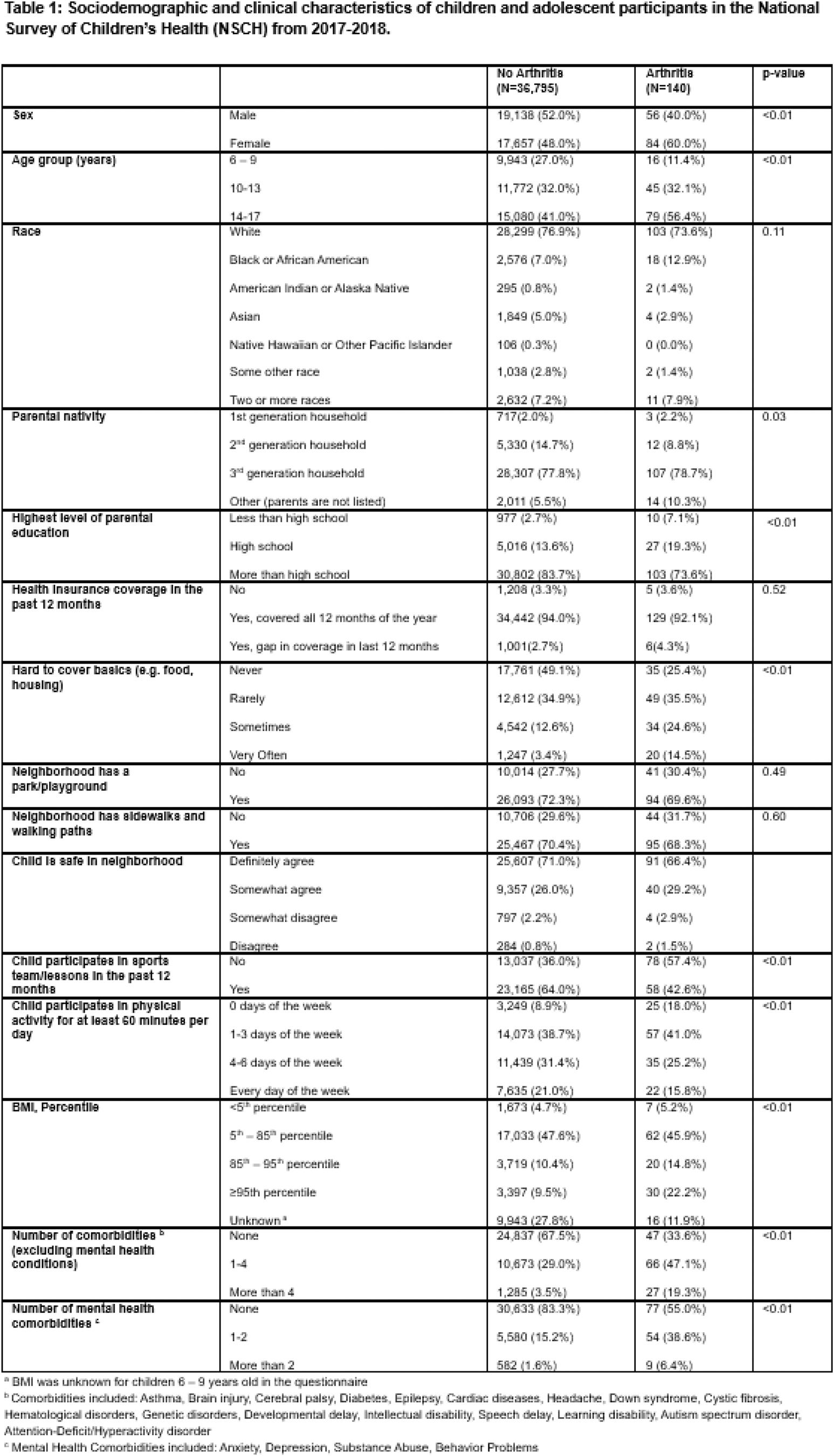
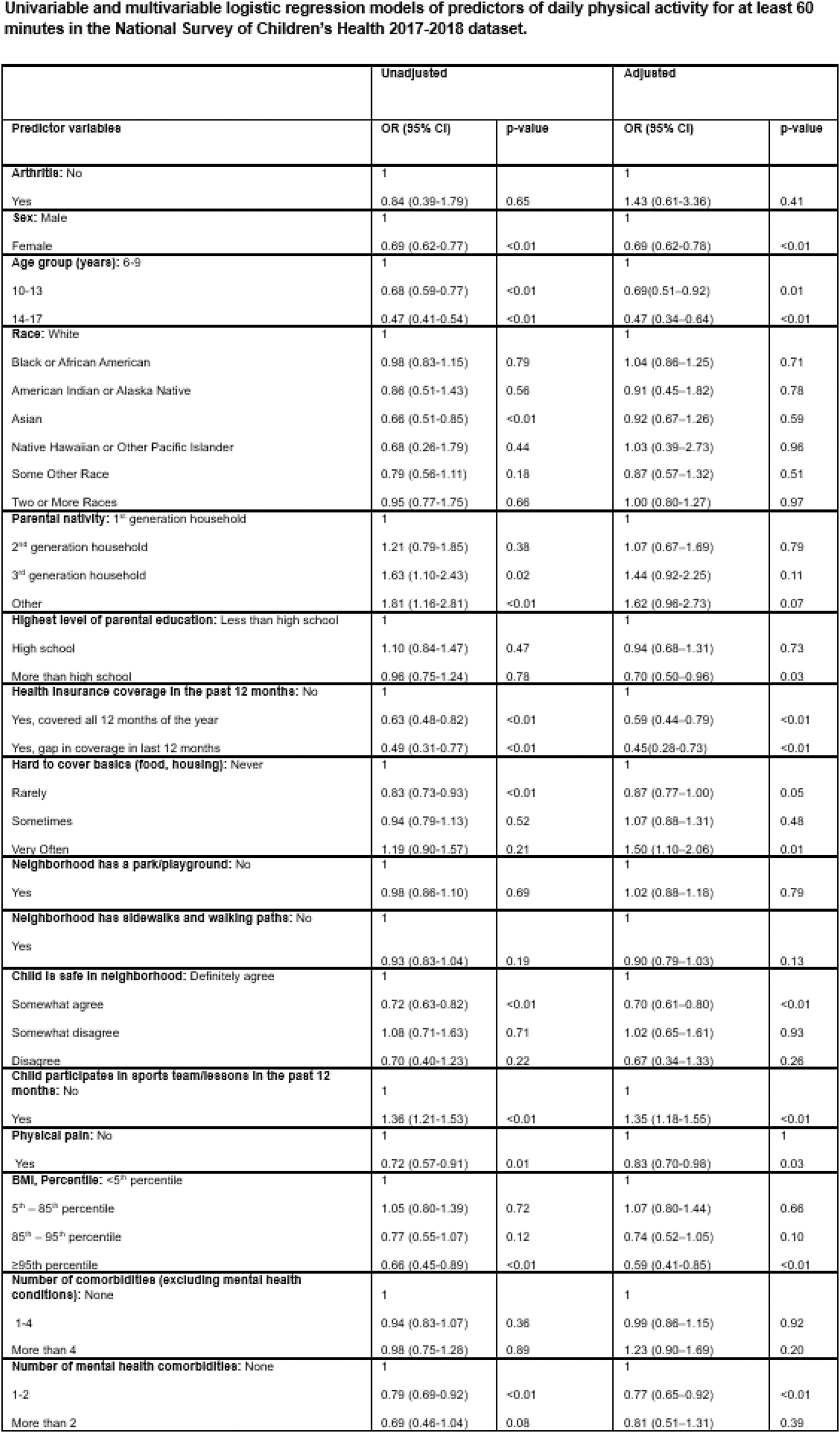
Methods: This is a cross-sectional study that assessed adherence to the recommended level of daily PA among pediatric with JA as compared to their peers without JA in the U.S. Data was sourced from 2017 and 2018 National Survey of Children’s Health (NSCH), a nationally representative survey that investigates overall health and well-being of children and adolescents in the U.S. Participants younger than 6 years of age were excluded since questions regarding exercise participation were only administered to those aged 6 years and older. Additionally, participants with missing data were excluded from the analysis. The cohort was defined by the presence or absence of arthritis, and descriptive statistics were performed, as appropriate. We then generated univariable and multivariable logistic regression models to investigate the association between an arthritis diagnosis and meeting the daily PA recommendation of at least 60 minutes. Additionally, we investigated exercise levels categorized by the practice of PA for at least 60 minutes “0 days per week”, “1-3 days per week”, “4-6 days per week”, or “daily” using ordinal logistic regression as a sensitivity analysis. Models were adjusted for potential confounders, including age, sex, socioeconomic status, and presence of other comorbidities.
Results: Data from 36,935 children and adolescents were analyzed with 140 participants reporting a diagnosis of arthritis with appropriate survey weights representing a population estimate of 33,946 children with arthritis (total population estimate = 44,067,458 individuals). Children with arthritis were less likely to engage in at least 60 minutes of daily exercise activity compared to children without arthritis (15.8% vs 21.0%; p<0.01) and exhibited higher rates of obesity (≥95th percentile; 22.2% vs 9.5%; p<0.01) compared to those without arthritis. Children with arthritis had higher rates of comorbidities, with 47.1% reporting 1-4 comorbidities and 19.3% reporting more than 4, compared to 29% and 3.5%, respectively, among those without arthritis (p<0.01). Mental health conditions were also more prevalent in children with arthritis, with 6.4% reporting more than two mental health conditions compared to 1.6% of children without arthritis (p<0.01). In unadjusted and adjusted analyses, the presence of arthritis was not statistically significant associated with meeting the WHO and CDC recommended 60 minutes of daily PA (Adjusted OR = 1.43; 95% CI: 0.61–3.36; p = 0.41). Girls and older children were significantly less likely to meet the PA recommendation. Other factors negatively associated with meeting PA guidelines included obesity (adjusted OR for ≥95th percentile = 0.59; 95% CI: 0.41–0.85; p<0.01), lack of neighborhood safety, and mental health conditions. Sports participation (adjusted OR = 1.35; 95% CI: 1.18–1.55; p<0.01) was strongly associated with higher odds of achieving daily PA. As a sensitivity analysis, we also analyzed PA levels categorized as 0, 1–3, or 4–6 days/week or daily. In our multivariable ordinal logistic regression models, arthritis was also not significantly associated with PA level (adjusted OR = 1.56; 95% CI: 0.81–2.30; p = 0.18).
Conclusion: Children and adolescents with and without arthritis demonstrated low adherence to CDC and WHO recommended PA levels. Overall, arthritis was not found to be a statistically significant predictor of exercise levels, in unadjusted or adjusted analyses. These findings might suggest that children with arthritis are at least as likely to achieve PA levels as their peers without arthritis, though PA levels were low among American children in general. Therefore, interventions aimed at increasing exercise participation in the American pediatric population may also increase PA levels in children with arthritis. Interventions to increase PA levels should address barriers such as mental health challenges, obesity, and neighborhood safety. In particular, encouragement in sports participation in pediatric rheumatology care, especially as children get older, may be a simple but effective intervention that could increase PA levels for children with JA.
REFERENCES: NIL.
Acknowledgements: NIL .
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (