

Background: Rituximab (RTX) has been used to treat SLE for 20 years but efficacy is limited by inadequate B-cell depletion. Emerging therapies such as CD19 CAR-T-cells have been reported to induce deeper B-cell depletion and thereby drug-free remission up to 18 months. However, with RTX, we showed that depth of depletion and rate of repopulation were highly variable, and related to patient factors e.g. complement levels and FCGR genotype. Using highly sensitive flow cytometry, plasmablast repopulation ≤0.0008 x 10 9 /L predicted longer response [1]. Anecdotally, we have observed “RTX super-responders” with sustained remission after one cycle of therapy.
Objectives: To assess a) incidence of RTX-super-response, with or without concomitant immunosuppressant; and b) factors associated with long-response after the first RTX cycle, with a view to personalise anti-CD20 antibodies in SLE.
Methods: We conducted an observational study of consecutive RTX-treated SLE patients in a single centre over 20 years who had followed an on-demand retreatment strategy. Usual practice was to continue concomitant immunosuppressants but taper glucocorticoids. Univariable and multivariable logistic regression analyses were performed to identify factors associated with RTX long-response, with p<0.1 associated with the deviance used for inclusion into the model.
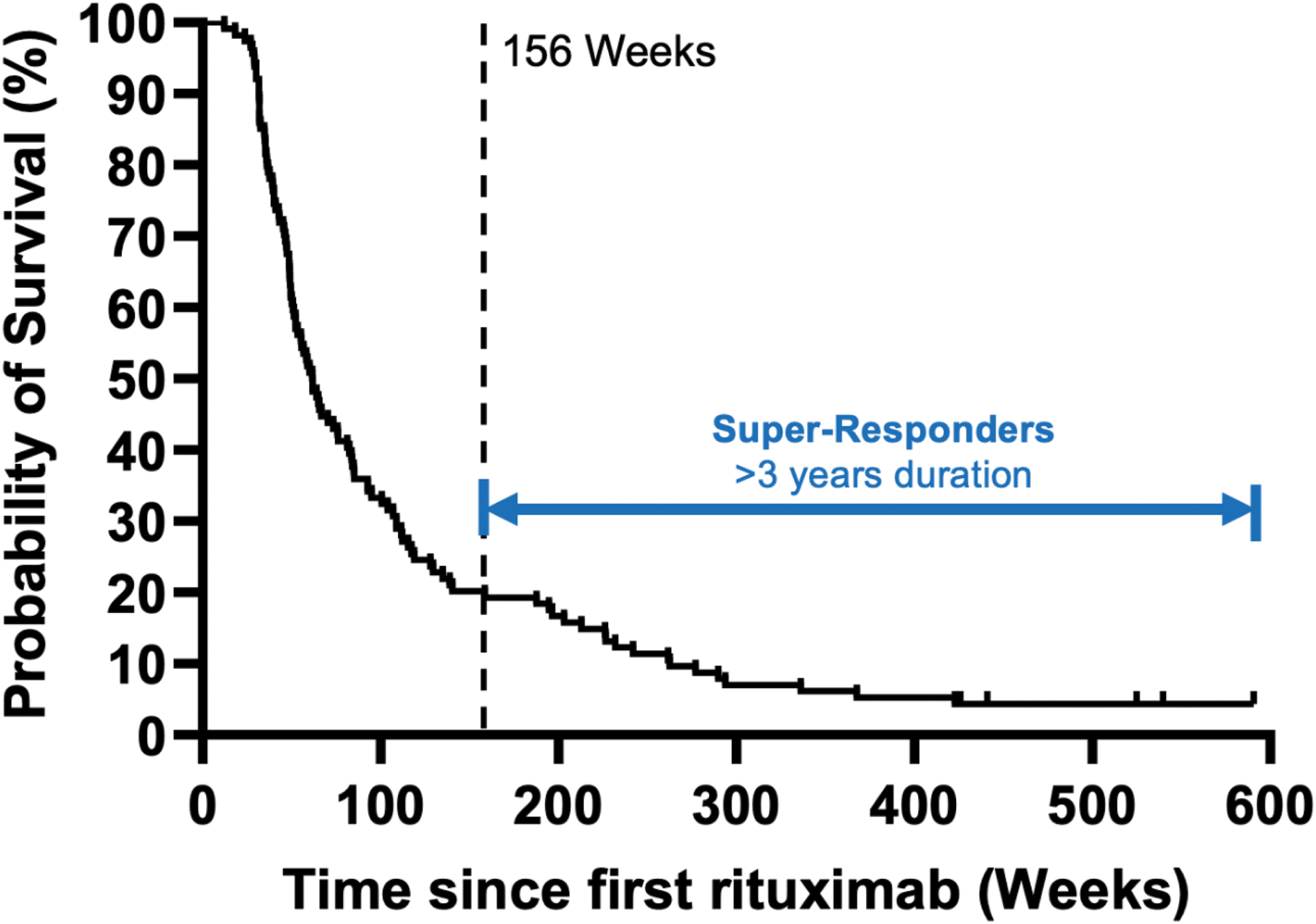
Results: Of 149 RTX-treated patients in Cycle 1, 114 were included in the study [excluded due to non-response in Cycle 1 = 17; received fixed retreatment at 6-9 months = 15; deaths within the first 3 years = 2; and discontinued RTX due to psoriasis = 1]. Based on survival curve, we defined RTX super-responders as >3 years (Figure 1). This occurred in 23/114 patients (20%) with median (IQR) duration of response of 263 (212, 423) weeks. At baseline, RTX-super-responders had: mean (SD) age 35 (14) years, 20/23 (87%) female, ancestry European=9/23 (39%); South Asian=6/23 (26%), Chinese/SE Asian=2/23 (9%); African=5/23 (22%); and Mixed=1/23 (4%)], concurrent APS 6/23 (26%), median (IQR) disease duration 2.8 (1, 5) years, median (IQR) SLEDAI-2K 11 (7, 15), and median (IQR) numeric BILAG score 21 (13, 25). Details of disease activity and B-cells over 3 years are provided in Table 1. Sustained suppression of plasmablasts was observed at 3 years: median (IQR) 0.0008 (0.0005, 0.0034). 8/23 RTX-super-responders (34.8%) were not prescribed immunosuppressants or withdrew them during follow up (drug free remission). In multivariable analysis of 114 patients, factors associated with duration of response >3 years were non-European ancestry (OR 4.6, 95% CI 1.6-12.7)) and concurrent APS, (3.2, 0.99-10.35), while longer disease duration (0.89, 0.80-0.99 per year) was associated with lower odds of rituximab-super-response. No other factors (age, sex, anti-dsDNA+, low C3/C4, number of antibodies, concomitant immunosuppressant, disease activity score, and active BILAG A/B in 5 most frequent domains) were predictive.
Conclusion: Sustained drug-free remission is not confined to patients who have received CAR-T CD19 but may be observed following RTX. One in five RTX-treated patients had >3 years response to their first cycle, and 1 in 12 had sustained, immunosuppressant-free remission. RTX-super-response is associated with patient characteristics typically denoting disease severity (early disease, non-European ancestry and APS), as well as marked suppression of plasmablast repopulation. This suggests that sustained drug-free remission is a feature of the overall immune environment rather than the modality of B-cell killing. Given their safety and low cost, anti-CD20 monoclonal antibodies in early poor-prognosis SLE may be preferable to intensive therapy in refractory disease.
REFERENCES: [1] Md Yusof MY et al, Ann Rheum Dis. 2017 Nov;76(11):1829-1836
Kaplan-Meier plot of relapse-free survival after a first cycle of rituximab.
SLEDAI-2K and B-cells data for Rituximab Super-Responders over 3 years
| Baseline median (IQR) SLEDAI-2K | 6-Month median (IQR) SLEDAI-2K | 2-Year
| 3-Year
| Baseline median (IQR) Plasmablast
| 6-Month median (IQR)
| 3-Year
|
|
|---|---|---|---|---|---|---|---|
| Immunosuppressant-Free RTX
| 9 (6-13) | 1 (0-2) | 1 (0-2) | 1 (0-2) | 0.0048 (0.0035-0.0092) | 0 (0 – 0.0001) | 0.0023 (0.0007-0.0051) |
| RTX
| 10 (8-14) | 3 (2-4) | 2 (1-3) | 2 (0-2) | 0.0062 | 0.0002 (0 – 0.0003) | 0.0007 (0.0003-0.0012) |
Acknowledgements: This Article presents independent research funded and supported by the National Institute for Health and Care Research (NIHR) Leeds Biomedical Research Centre. The views expressed are those of the author(s) and not necessarily those of the NIHR or the UK Department of Health and Social Care.
Disclosure of Interests: Junaid Patel: None declared. Paul Emery Roche, Edward M. Vital Roche, Roche, Roche, Sandoz, Md Yuzaiful Md Yusof Roche.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (