

Background: Axial spondyloarthritis (axSpA) is a chronic inflammatory condition that mostly requires lifelong management, where exercise combined with pharmacological therapy plays a key role. Previously, supervised exercise programs have been shown to be more effective than unsupervised home-based exercises in improving outcomes for patients with axSpA [1]. Technological advancements enabled remote supervision for online exercise programs offering a practical alternative to face-to-face interventions. Recent studies investigated synchronous telerehabilitation models for yoga and core stabilization exercises for patients with axSpA, often featuring varying levels of supervision and primarily focusing on short-term outcomes [2, 3]. However, clinical Pilates exercises, whose face-to-face benefits are well-documented in axSpA, remain to be explored in the context of telerehabilitation.
Objectives: To compare the effects of clinical Pilates-based exercise programs delivered via telerehabilitation and face-to-face on patients with axSpA, including outcomes at the end of the intervention and during a six-month follow-up period.
Methods: This single-blind, randomized controlled trial involved forty-six patients with axSpA. Patients were assigned to the face-to-face exercise group (FEG) or the telerehabilitation exercise group (TEG) using randomization through opaque, sealed envelopes. This interim analysis included data from 22 patients in the FEG and 16 patients in the TEG who completed the intervention and the six-month study period (follow-up data: n= 19 in FEG, n= 13 in TEG at Week 32). At the beginning, patient education consisting of a one-hour individual session was provided to both groups by the physiotherapist in the clinic. Following this, the FEG received clinical Pilates-based exercise training in the clinic under the real-time, one-on-one supervision of a physiotherapist. Similarly, the TEG received the same training individually and in real-time via video conferencing, either through Zoom or WhatsApp, under the direct physiotherapist supervision. Both groups performed exercise sessions three times a week for 8 weeks. Outcomes included the BATH indices (BASDAI, BASFI, BASMI), Ankylosing Spondylitis Performance Index (ASPI), BETY-Biopsychosocial Questionnaire (BETY-BQ), Hospital Anxiety and Depression Scale (HADS), and Assessment of SpondyloArthritis international Society-Health Index (ASAS-HI). Measurements were taken at baseline (Week 0), after 8 weeks of intervention (Week 8), and at a 6-month follow-up (Week 32). Statistical analyses included the Wilcoxon signed-rank test for within-group comparisons and the Mann-Whitney U test for between-group differences. Effect sizes (Cohen’s r) were calculated to evaluate the magnitude of changes.
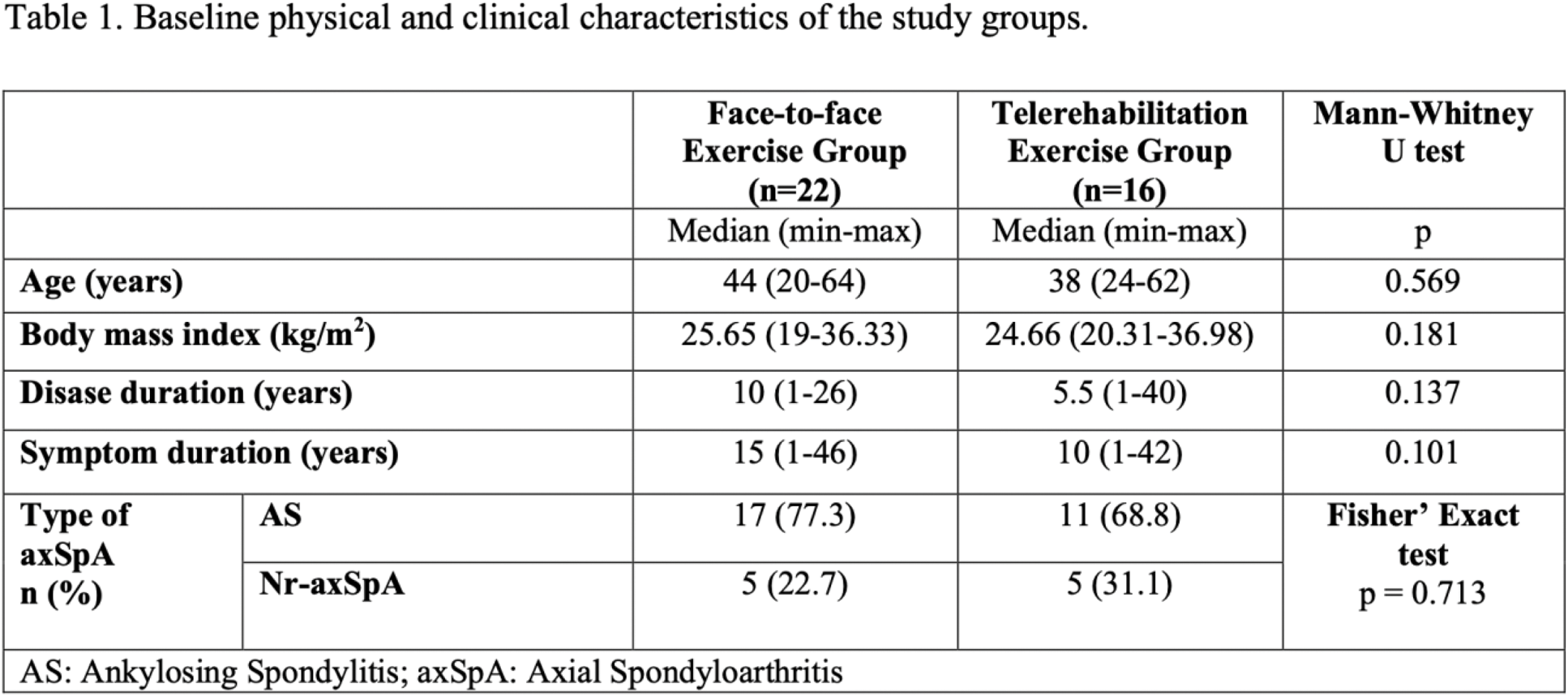
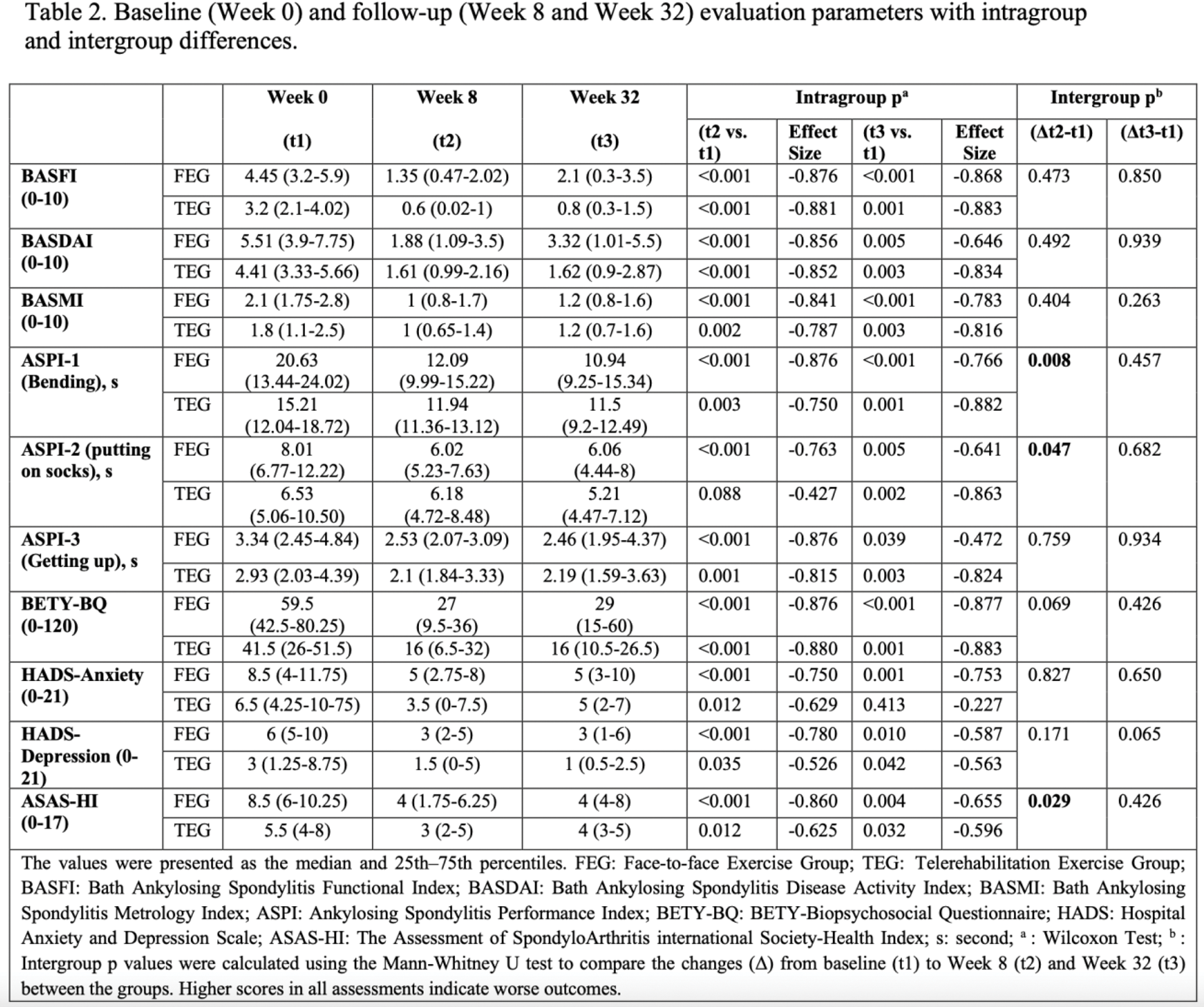
Results: Baseline physical and clinical characteristics were similar between the groups (p> 0.05) (Table 1). In the FEG, all parameters showed significant improvements at both Week 8 and Week 32 compared to baseline (p < 0.05). In the TEG, significant improvements were observed in most parameters, except for ASPI-putting on socks (Week 8 vs. baseline: p = 0.088) and HADS-anxiety (Week 32 vs. baseline: p = 0.413). Intergroup comparisons of changes (Δ) from baseline to Week 8 and Week 32 were not statistically significant for most parameters (p > 0.05), except for ASPI-bending (Δt2-t1: p = 0.008), ASPI-putting on socks (Δt2-t1: p = 0.047), and ASAS-HI (Δt2-t1: p = 0.029). No significant intergroup differences were found for changes from baseline to Week 32 (Δt3-t1: p > 0.05) in any parameter (Table 2).
Conclusion: This interim analysis demonstrated that clinical Pilates-based exercise training delivered via telerehabilitation may provide comparable improvements to face-to-face exercises in patients with axSpA. Notably, the benefits observed through telerehabilitation were maintained over a six-month follow-up period. However, participant dropout rates over time highlight the importance of addressing adherence in long-term exercise programs. Future research should focus on strategies to enhance adherence and minimize dropout rates to optimize the long-term benefits of telerehabilitation for axSpA.
REFERENCES: [1] Liang, Hui, et al. “The comparative efficacy of supervised-versus home-based exercise programs in patients with ankylosing spondylitis: a meta-analysis.” Medicine 99.8 (2020): e19229.
[2] Acar, Y., Ilçin, N., & Sari, İ. (2023). The Effects of Tele-Yoga in Ankylosing Spondylitis Patients: A Randomized Controlled Trial. Journal of Integrative and Complementary Medicine, 29(11), 727-737.
[3] Şen, E. N., Saritaş, F., & Öztürk, Ö. (2024). Synchronous and asynchronous remote core stability exercises in patients with axial spondyloarthritis: a randomized-controlled clinical trial. Irish Journal of Medical Science (1971-), 1-10.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (