

Background: Systemic sclerosis (SSc) is associated with microvascular and macrovascular damage, leading to an increased cardiovascular risk. Findings in nailfold capillaroscopy (NFC) have been linked to vascular damage. The Systematic Coronary Risk Assessment (SCORE2) algorithm estimates the probability of suffering a cardiovascular event in the general population but underestimate the risk in SSc.
Objectives: To evaluate the predictive capabilities of NFC for atheroma plaques, major cardiovascular events (MCE), and mortality due to MCE in SSc. To determine if the use of incorporating NFC findings into the SCORE2 and SCORE2-OP models may improve stratification of cardiovascular risk in SSc.
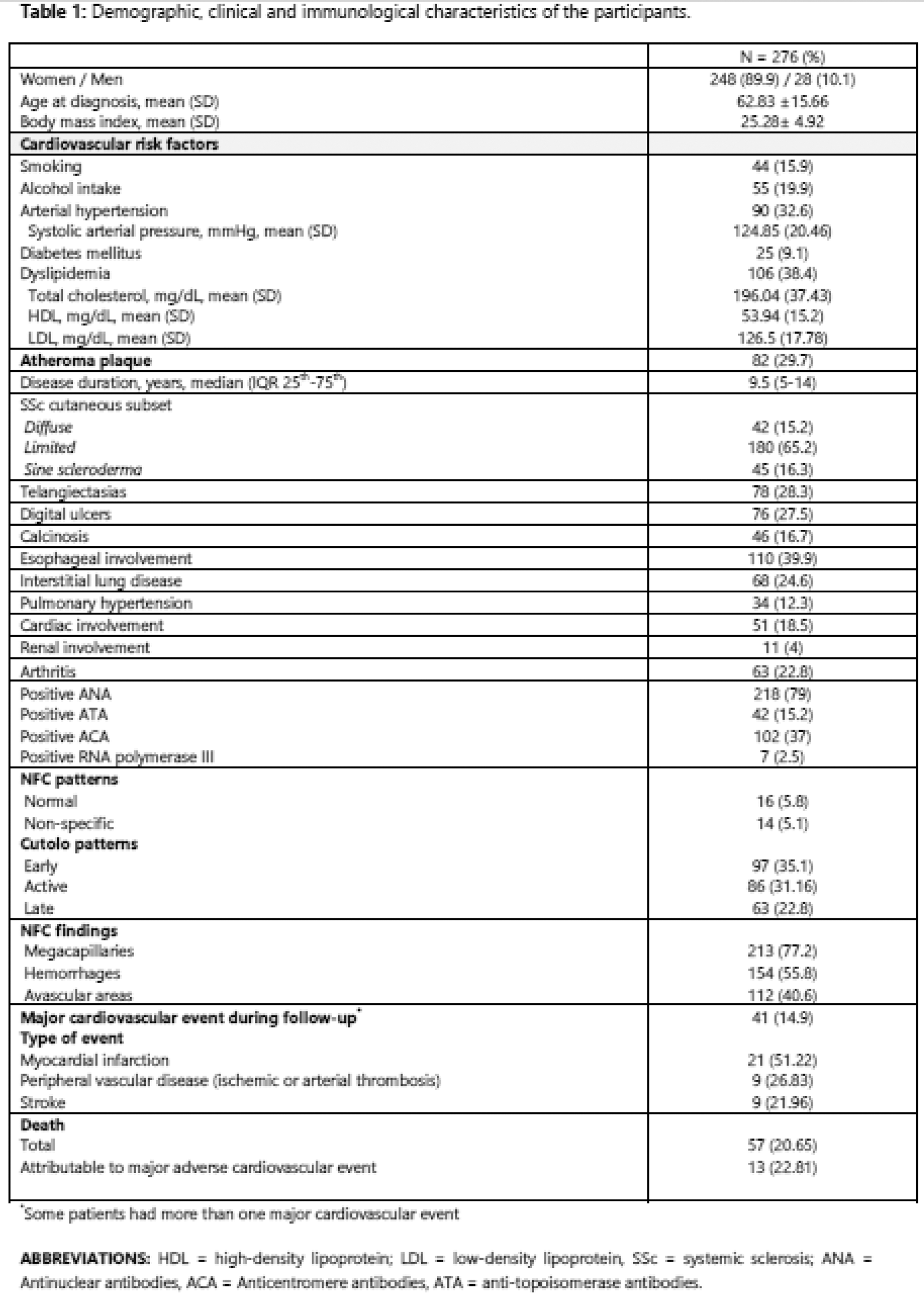
Methods: This is a multicenter retrospective study which included 276 SSc patients diagnosed per the 2013 ACR/EULAR criteria and without prior cardiovascular events. Patients under 40 years of age or with severe chronic kidney disease or previous cardiovascular events were excluded. The SCORE2 risk was calculated for patients between 40 to 69 years of age and the SCORE2-OP for patients of 70 years of older. All patients underwent a NFC within one month of diagnosis. Atheroma plaques were assessed by carotid ultrasound and/or retrospective imaging analysis. Multivariate logistic regression identified predictors of atheroma plaques, MCEs and MCE-related mortality. SCORE2 and SCORE2-OP models were adjusted using NFC finding, and their discriminative performance was evaluated through ROC curves.
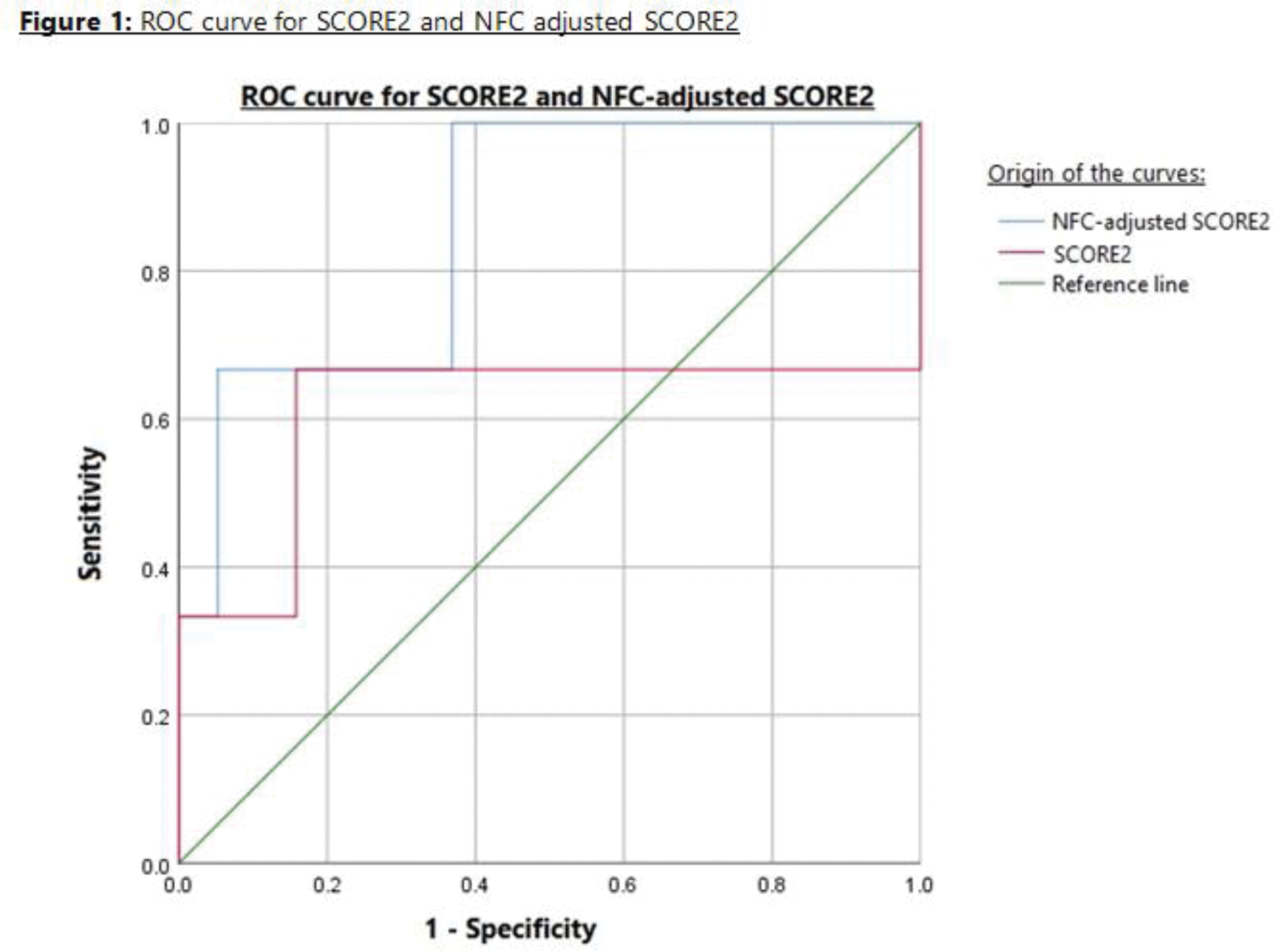
Results: At baseline, 89% of patients presented a scleroderma NFC pattern (35.1% early, 31.16% active, and 22.8% late). Megacapillaries were found in 77.2%, haemorrhages in 55.8%, and avascular areas in 40.6% of patients. During a median follow-up of 9.5 years, 41 patients (17.8%) experienced a MCE. The overall mortality rate was 20.7% (57 patients), with 22.81% of deaths attributed to MCEs. The demographic, clinical and immunological characteristics are presented in Table 1. Avascular areas in NFC were independently associated with MCE (OR = 5.983, p = 0.008), whereas hemorrhages were found to be a protective factor (OR = 0.313, p = 0.007). NFC did not predict avascular areas nor mortality by MCEs in the multivariate model. The mean value of the SCORE2 algorithm was 2.89 and of SCORE2-OP was 19.94. The SCORE2 values were adjusted by multiplying the original risk estimates by the odds ratios for avascular areas (5.983) and hemorrhages (0.313), derived from multivariate analysis, to reflect their independent impact on cardiovascular events. For patients between 40 to 69 years, the SCORE2 classified 87% as low-to-moderate and 13% as high risk. The NCF-adjusted SCORE2 reclassified 34.78% of patients: 8.7% from low-to-moderate to high risk, 21.74% from low-to-moderate to very high risk and 4.35% from high to very high risk. For patients ≥70 years old, the SCORE2-OP classified 7.2% as low-to-moderate, 31.2% as high risk and 61.6% as very high risk. The NFC-adjusted SCORE2 reclassified 30.77% of patients. 15.2% decreased from high to low-to-moderate risk, 8% from very high to a high risk. 9.6% increased from low-to-moderate to very high risk and 10.4% from high to very high risk. The performance of the NFC-adjusted SCORE2 and SCORE2-OP was evaluated using receiver operating characteristic (ROC) curves. In the SCORE2 group, the AUC improved significantly from 0.614 (95% CI: 0.211–0.764) to 0.860 (95% CI: 0.646–0.913) with NFC adjustment, demonstrating superior discrimination (Figure 1). The greatest improvement was in the specificity, increasing with the NFC adjustment from 78.9% to 89.5%. The sensitivity however, increased from 65.6% to 68.7%. For SCORE2-OP (patients ≥ 70 years), neither version proved to be deterministic in our sample (AUC = 0.500).
Conclusion: Avascular areas in NFC at the time of diagnosis are an independent cardiovascular risk factor in SSc, whereas hemorrhages are an independent protective factor. Adjustment of the SCORE2 model by NCF findings increases its predictive accuracy for cardiovascular events, making NFC a robust cardiovascular risk predictor in SSc.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (