

Background: People with rheumatoid arthritis (pwRA) are prone to fall short of the World Health Organization’s physical activity (PA) recommendations due to perceived fatigue and pain. Relationships between fatigue and PA are complex, as it has been suggested that symptoms can be determinants but also consequences of reduced engagement in PA. Given the high prevalence of excessive fatigue and the profound impact of fatigue on patients’ health-related quality of life and social role participation, it is of importance to further explore associations between objectively determined PA (patterns) and fatigue.
Objectives: To investigate objectively measured PA patterns and the association between PA and self-reported fatigue in people with rheumatoid arthritis (pwRA) as compared to healthy controls (HC).
Methods: In this observational cross-sectional study, pwRA (DAS28 > 2.6) and HC wore an ActiGraph wGT3X-BT tri-axial accelerometer (ActiGraph LLC) on one ankle for at least 4 days. Accelerometer-based outcomes were vector magnitude counts/min (i.e. the square root of the summed sagittal, frontal, and vertical axes’ counts/min squared – primary outcome), step count, and the amount of time that PA was exerted at moderate-to-vigorous intensity. Accelerometer data were separated according to the day and time at which they were collected (i.e., weekday and weekend; daytime and evening) to investigate the PA pattern. Fatigue severity was assessed with the Fatigue Severity Scale (FSS, 0-7 with higher scores indicating more severe fatigue). Associations between fatigue, presence of RA, and PA were examined using multilevel generalized estimating equations models, with patient and day-timing as levels in the analysis. Interactions between the presence of RA and fatigue were tested. Manual forward selection was used to explore multivariable associations while adjusting for confounders.
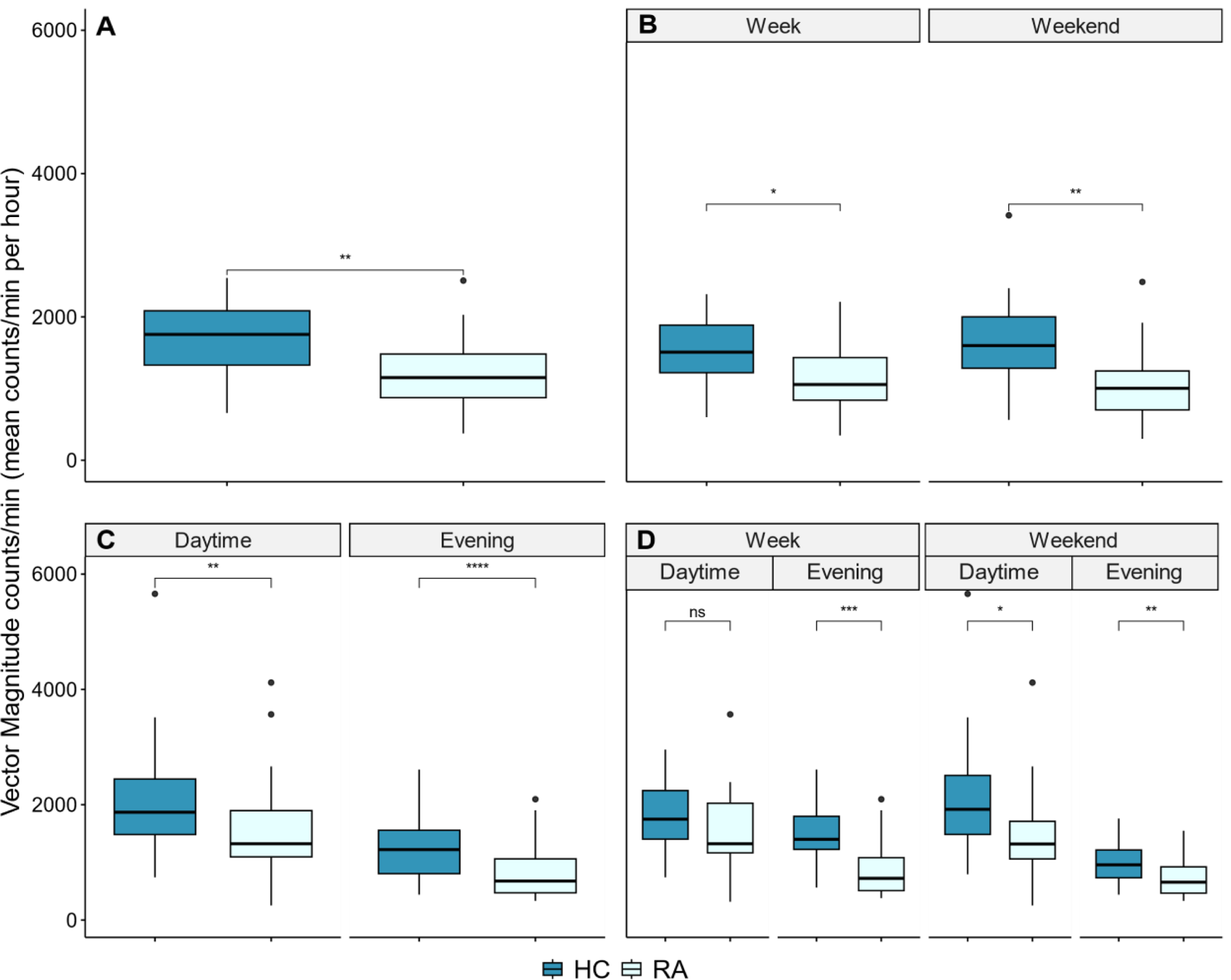
Results: Participants were 23 pwRA (20 females, age 52 (SD 13), FSS 4.7 (1.4)) and 18 HC (14 females, age 52 (11), FSS 2.1 (1.0)). The vector magnitude counts/mins was lower in pwRA than in HC at any time, with non-significant differences on weekdays during daytime (1534.3 (691.3) in pwRA vs 1802.6 (610.6) in HC) but larger discrepancies on week evenings (880.7 (491.4) in pwRA vs 1457.3 (572.7) in HC) (Figure 1). In line with the pattern of vector magnitude counts/min, the number of steps taken (587 (226) steps/h in pwRA and 724 (224) steps/h in HC) and the time that PA was exerted at a moderate-to-vigorous intensity (1.6 (1.4) min/h in pwRA and 2.7 (1.5) min/h in HC) was also reduced in patients as compared to HC. There was no interaction between fatigue and having RA, indicating that fatigue affected PA of pwRA and HC in a similar fashion. The absence of interactions between group and day-timing indicated no significant differences in the pattern of PA between pwRA and HC. Having RA was significantly and negatively related to vector magnitude counts/min after confounder adjustment (β = -330.63; 95% CI = -650.45 to -10.81; Table 1). In the multivariable model, lower vector magnitude counts/min was seen in pwRA, persons with higher fatigue severity (β = -43.89; 95% CI = -135.26 to 47.48), and in persons with higher BMI (β = -27.18; 95% CI = -50.73 to -3.62). BMI, presence of RA, and fatigue were also negatively associated with step count and the time that PA was performed at moderate-to-vigorous intensity.
Vector Magnitude counts per minute (mean counts/min per hour) measured in rheumatoid arthritis patients (RA) and healthy controls (HC) overall (A), on weekdays as compared to the weekend (B), during the day and during the evening (C), and separated by day as well as timing of the day (D). ns p >.05, * p <.05, ** p <.01, *** p <.001, **** p <.0001.
Effect of RA vs HC on the Vector Magnitude Counts per Minute in univariable and multivariable Generalized Estimating Equations analyses.
| Univariable model | Multivariable model | |
|---|---|---|
| Variables | Coefficient (95% CI) | Coefficient (95% CI) |
| Age (years) | 2.48 (-9.53; 14.50) | na |
| Male vs Female | 136.46 (-315.00; 587.91) | na |
| BMI (kg/m 2 ) | -47.14 (-78.60; -15.67) | -27.18 (-50.73; -3.62) |
| FFM (kg) | -6.20 (-24.68; 12.28) | na |
| RA vs HC | -467.72 (-768.40; -167.05) | -330.63 (-650.45; -10.81) |
| FSS (0-7 ) | -117.06 (-216.04; -18.09) | -43.89 (-135.26; 47.48) |
| Weekend vs Week | -24.48 (-301.03; 252.07) | § |
| Evening vs Daytime | -724.93 (-945.42; -504.44) | § |
| Day-Timing: | ||
| Weekend-Daytime | Reference | Reference |
| Weekday-Daytime | -123.89 (-509.31; 261.54) | -129.66 (-527.19; 267.87) |
| Weekday-Evening | -687.07 (-1059.60; -314.54) | -723.68 (-1091.19; -356.16) |
| Weekend-Evening | -942.19 (-1287.31; -597.07) | -970.77 (-1322.72; -618.82) |
§Variables Weekend vs Week and Evening vs Daytime were not considered for the multivariable model, since the variable Day-Timing combines the information from both these variables
na: variable not significant in the univariable model and not a confounder for RA vs HC and therefore not included in the multivariable model
BMI, Body Mass Index; FFM, Fat Free Mass; FSS, Fatigue Severity Scale
Conclusion: Patients with RA performed less objectively measured PA than HC. Fatigue is inversely associated with PA and this relationship does not differ between pwRA and controls. Further research is required to distinguish the effects of transient fatigue vs fatigue as a trait, employability status, inflammation, and medication usage on PA. This will help to understand which RA patients are most prone to fall short of the PA recommendations and to design effective interventions accordingly.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (