

Background: Increasing use of opioid, non-opioid and gabapentinoid analgesics has been reported in some countries, such as the United States, leading to an increase in morbidity and mortality. In France, opioid-related deaths increased from 1.3 to 3.2 per 1,000,000 population between 2004 and 2017 and opioid is used by 17% of the population (Chenaf et al. 2019). Our hypothesis is that a minority of people with musculoskeletal pain have high doses of opioids and gabapentinoids, and during the period of inclusion, there is no increase in their consumption in relation to French regulation.
Objectives: The aim of this study was to describe the use of analgesics by people with subacute or chronic musculoskeletal pain in France and to evaluate the trend of chronic use of opioids during the period of inclusion.
Methods: This study is a cross-sectional study nested in the Constances cohort, which is the largest cohort in the French general population, made up of volunteers aged 18 to 69 at inclusion, and which is linked to the French reimbursement claim database. Data from questionnaires at inclusion were used. Participants: Low back pain, neck pain, shoulder pain or knee pain lasting more than 30 days in the last 12 months were considered significant. Chronic pain syndrome was defined as permanent pain in the last 12 months in at least 4 of the 6 body regions. Participants with cancer in the last 12 months were excluded from the analysis. Missing data were managed by multiple imputation. The exposure of interest was defined on the basis of analgesic deliveries in the 12 months preceding inclusion. For opioids, an oral morphine equivalent (OME) was calculated by estimating the total dose of opioids delivered during the year. The number of days of treatment was estimated in relation to a 30-day supply of the drug, taking into account the possible overlap of supplies. The OME was calculated by dividing the total opioid dose by the number of treatment days. High or very high dose opioid use was defined as an OME > 50 or > 90/day. The duration of each delivery was calculated for an estimated duration of 30 days, and adjusted in the case of overlapping deliveries. Chronic opioid use was defined as at least 4 separate deliveries over 12 months or 3 deliveries and at least 10 boxes of opioids over 12 months. In order to assess the trend according to the year of inclusion, a Cochran-Armitage trend test of chronic opioid deliveries and gabapentinoids deliveries was calculated.
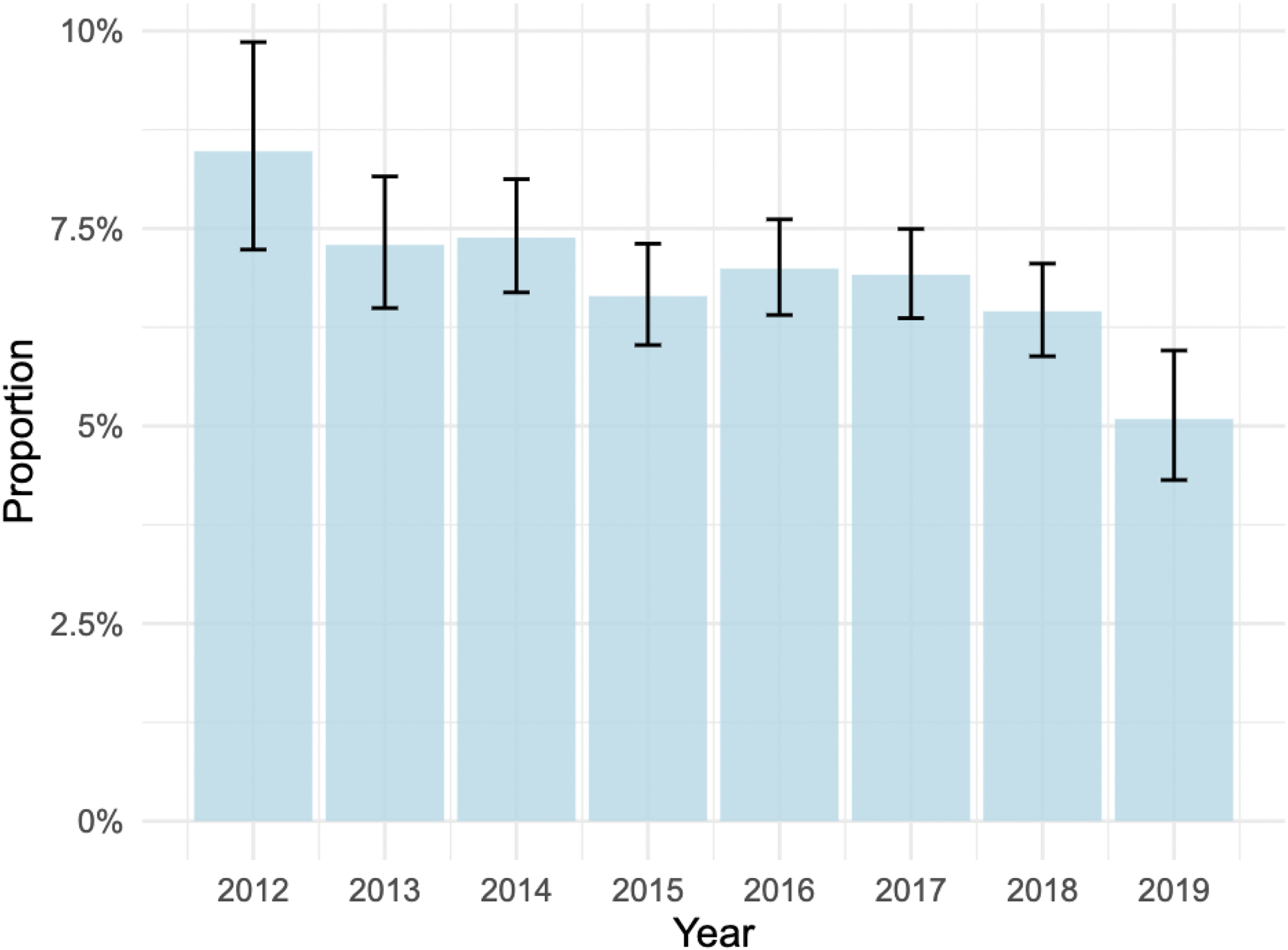
Results: 155,312 people were included in the CONSTANCES cohort, with data linked to the SNDS from 2012 to 2019. Deliveries of paracetamol, nefopam, NSAIDs, gabapentinoids, weak opioids and strong opioids were very similar regardless of pain location (Table 1) and higher than participants without musculoskeletal pain. In the whole cohort, 81% of participants did not have opioid delivery, 7.8% had opioids < 50 mg EMO/ day, 4,3% between 50 and 90mg/ day and 4.3% more than 90 mg/day. Chronic opioid use was 0.8% for participants without musculoskeletal pain, ranged from 6.3% to 6.8% for the various pain sites, and 13% for chronic pain syndrome. 8.8 to 9.1% of participants with pain had > 90 mg/ day, and 12.9% for chronic widespread pain (Table 1). For the different pain locations, there was a decrease in the chronic delivery of opioids (p<0.001) between 2012 and 2020 (Figure 1). There was no trend towards an increase or decrease in the use of gabapentinoids.
delivery of analgesics within 12 months according to pain location. Percentage (95% confidence interval). OEM = oral equivalent morphine.
| Delivery in the 12 months before inclusion | No musculoskeletal pain
| Back pain
| Neck pain
| Shoulder pain
| Knee pain
| Chronic widespread pain N=4626 |
|---|---|---|---|---|---|---|
| Paracetamol | 46.8
| 61.0
| 61.2
| 60.4
| 60.8
| 69.2
|
| NSAID | 33.5
| 52.9
| 52.5
| 53.1
| 53.2
| 59.1
|
| Nefopam | 0.5
| 1.5
| 1.5
| 1.6
| 1.4
| 2.9
|
| Gabapenti-noids | 0.6
| 3.4
| 3.5
| 3.5
| 3.6
| 8.6
|
| Weak opioids | 12.3
| 27.9
| 26.3
| 27.4
| 27.5
| 40.5
|
| Strong opioids | 0.2
| 1.5
| 1.4
| 1.6
| 1.5
| 3.3
|
| Chronic opioid use | 0.8
| 6.8
| 6.3
| 6.7
| 6.7
| 16.0
|
| Mean daily opioid use:
| 87.7
| 71.9
| 73.4
| 72.2
| 72.2
| 58.7
|
| - less than 50mg/day OME | 5.5
| 12.2
| 11.8
| 12.2
| 11.8
| 17.6
|
| - 50 à 90 mg/ day OME | 2.9
| 7.2
| 6.5
| 6.8
| 6.9
| 10.8
|
| - more than 90 mg/ day EMO | 3.9
| 8.8
| 8.4
| 8.7
| 9.1
| 12.9
|
proportion of low back pain patients with chronic opioid use between 2012 and 2019.
Conclusion: The use of opioid and gabapentinoids analgesics for musculoskeletal pain remains moderate in terms of prevalence and dosage, in line with French and international recommendations.
REFERENCES: NIL.
Acknowledgements: French Society of Rheumatology (grant for this study).
Disclosure of Interests: Florian Bailly Lilly, Grünenthal, Benjamin Granger: None declared, Violaine Foltz: None declared, Sofiane Kab: None declared, Audrey Petit: None declared, Florence Tubach: None declared, Bruno Fautrel: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (