

Background: Psoriatic arthritis (PsA) is a chronic inflammatory arthritis linked to high cardiovascular (CV) risk. Despite improved CV risk from biologic therapy, CV morbidity persists, with higher rates of hypertension (HT), diabetes mellitus type 2 (DM2), dyslipidemia and obesity. These factors are linked to the pathophysiology of PsA. Physical activity in PsA patients promotes a healthy BMI, lowers blood pressure, improves self‐confidence, and reduces stress, lowering CV risk.
Objectives: This study aimed to investigate: (1) PA levels in PsA patients, (2) the presence of other CV risk factors (HT, DM2, smoking, dyslipidemia, obesity, and disease activity), (3) demographic, clinical, and behavioral characteristics of patients with specific PA levels, and (4) latent subpopulations with similar characteristics.
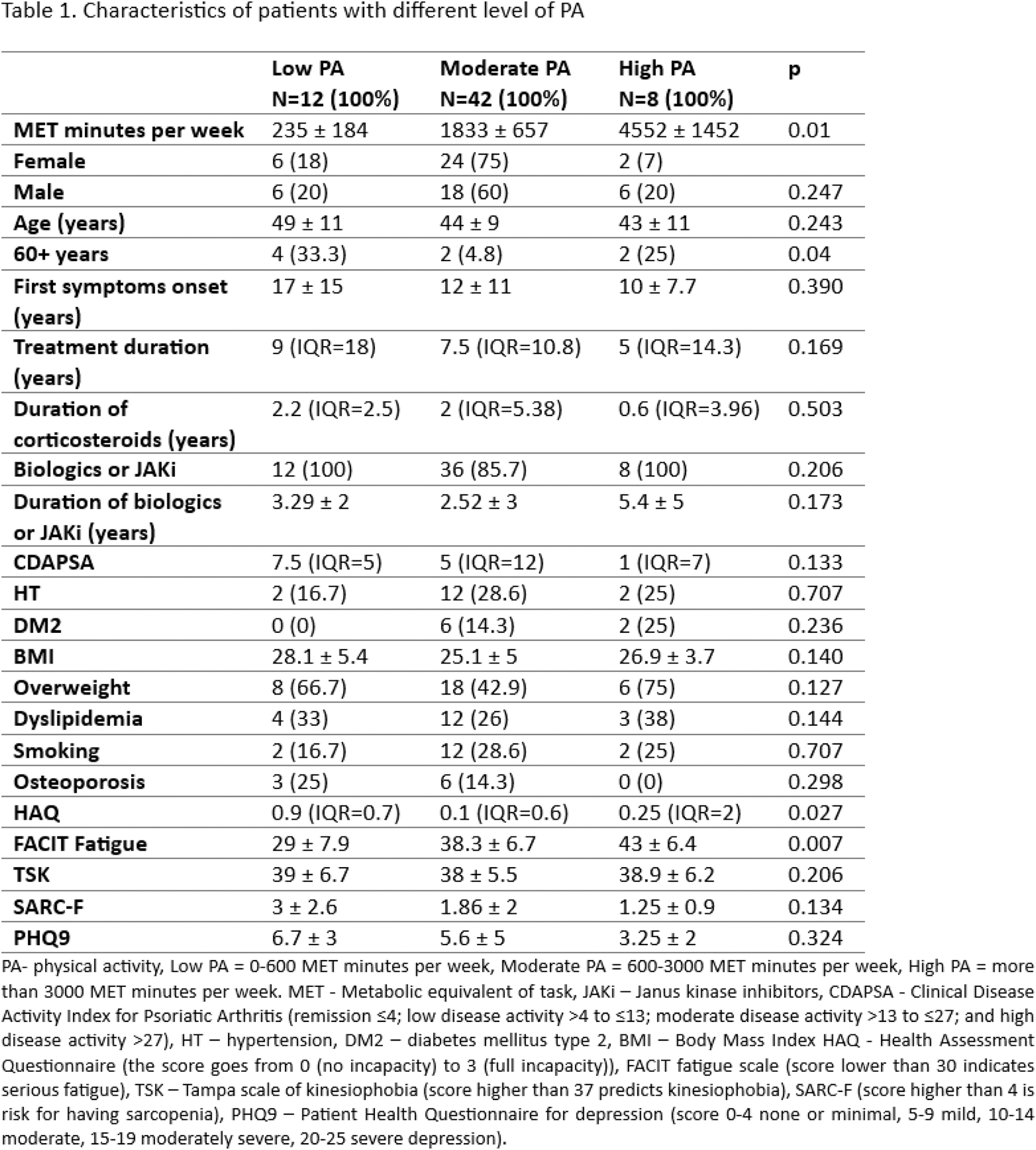
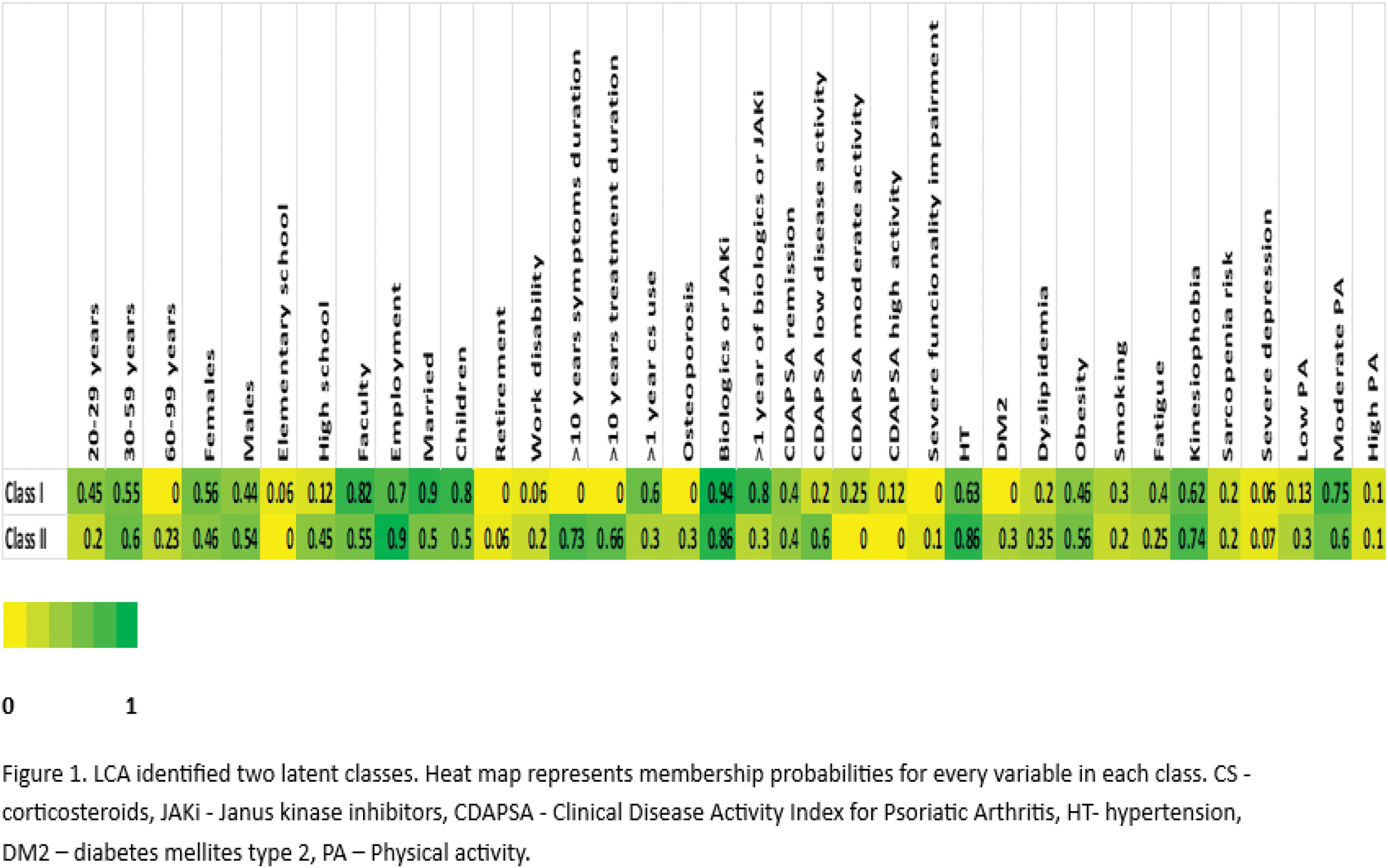
Methods: Sixty-two patients with PsA were included in this cross-sectional study. All patients completed the International Physical Activity Questionnaire (IPAQ), the Functional Assessment of Chronic Illness Therapy-Fatigue Scale (FACIT-F), the Tampa Scale for Kinesiophobia (TSK), the Strength, Ambulation, Rising from a Chair, Stair Climbing, and History of Falling questionnaire (SARC-F) for sarcopenia assessment, and the Patient Health Questionnaire-9 (PHQ-9) for depression. Basic socio-epidemiological data, the Clinical Disease Activity Index for Psoriatic Arthritis (CDAPSA), disease duration, therapy, and comorbidity data were retrieved from electronic patient records. Latent class analysis (LCA) was used to identify subpopulations of patients (latent classes).
Results: The cohort was nearly balanced between male and female patients (30/62 vs 32/62), with average ages of 47 and 42 years (p>0.05), respectively. Regarding disease activity, 80% were in remission or low disease activity. PA levels were classified as low (19.4%), moderate (67.7%), and high (12.9%). Patients with low PA experienced more fatigue (p=0.007), higher functional impairment (p=0.027), and were more likely to be over 60 years old (p=0.04). In the cohort the prevalence of CV factors was: HT (26%), DM2 (13%), depression (13%), obesity (52.6%), dyslipidemia (30%), and smoking (26%). LCA revealed two latent classes. Class I consisted mainly of younger adults (20–59 years) with a slight female predominance (56%). Most were highly educated (82%) and employed (69%), with moderate PA levels (75%). CV risks included obesity (46%) and smoking (30%), though HT, DM2 and dyslipidemia were less common. In this class, 12% had high disease activity (CDAPSA), correlating with increased fatigue (40%). Class II included a broader age range (23% aged 60–99 years) and a slight male predominance (54%). Education was more varied (55% university degrees), and employment was high (93%). PA levels were lower, with 30% reporting low PA and 60% moderate PA. This class showed higher HT (86%), DM2 (30%), obesity (56%) and dyslipidemia (35%), while smoking (20%) was less common. Serious depression was more common (7%), possibly due to functional impairment (10%) and aging. Other outcomes include kinesiophobia (74%) and sarcopenia risk (19%), indicating barriers to PA.
Conclusion: This study showed that higher levels of PA in PsA patients are linked to reduced levels of fatigue and functional impairment, while lower PA levels were associated with age over 60 years. LCA revealed important differences in PA levels and CV risk factors. Patients with low PA, especially those over 60 years old and those with high disease activity exhibited higher rates of HT, DM2, dyslipidemia and obesity. Notably, older patients also faced greater barriers to PA, including higher levels of kinesiophobia and sarcopenia risk. These findings highlighted the need for tailored interventions to promote and educate about adequate PA in older individuals and those with higher disease activity. In conclusion, the management of inflammation in PsA patients, through both pharmaceutical treatment and physical activity, does indeed “kill two birds with one stone”, improving both disease activity and CV risk factors.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (