

Background: The impact of mental health on the effectiveness of biological therapies, such as tumor necrosis factor inhibitors (anti-TNF), has received little attention in spondyloarthritis. This study explores how psychological well-being, assessed through standardized tools such as the SF-12 and ASQoL, influences inflammatory activity in patients treated with anti-TNF therapy.
Objectives: To assess the impact of mental well-being on the effectiveness of anti-TNF medications in patients with spondyloarthritis with rheumatological conditions.
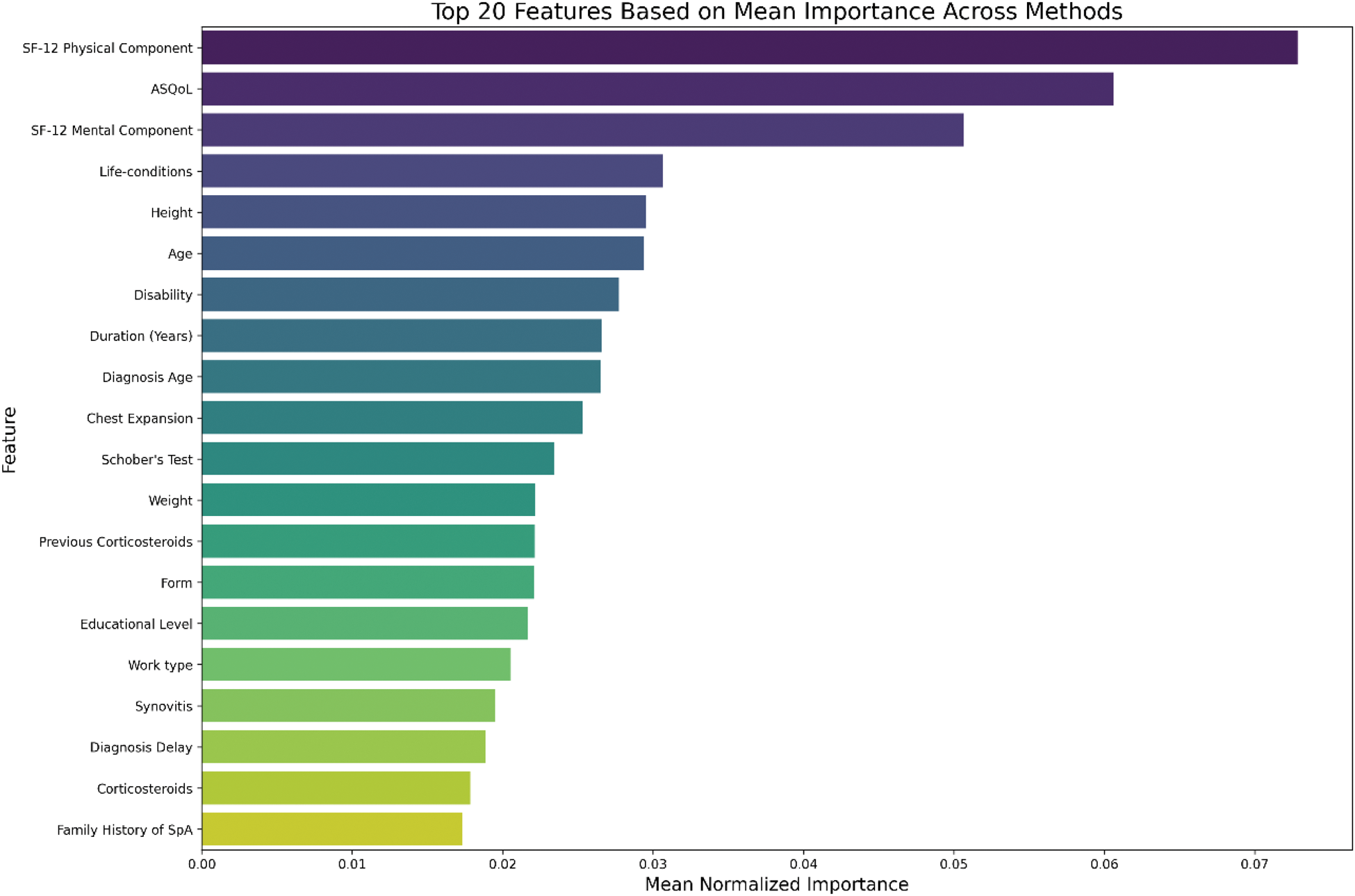
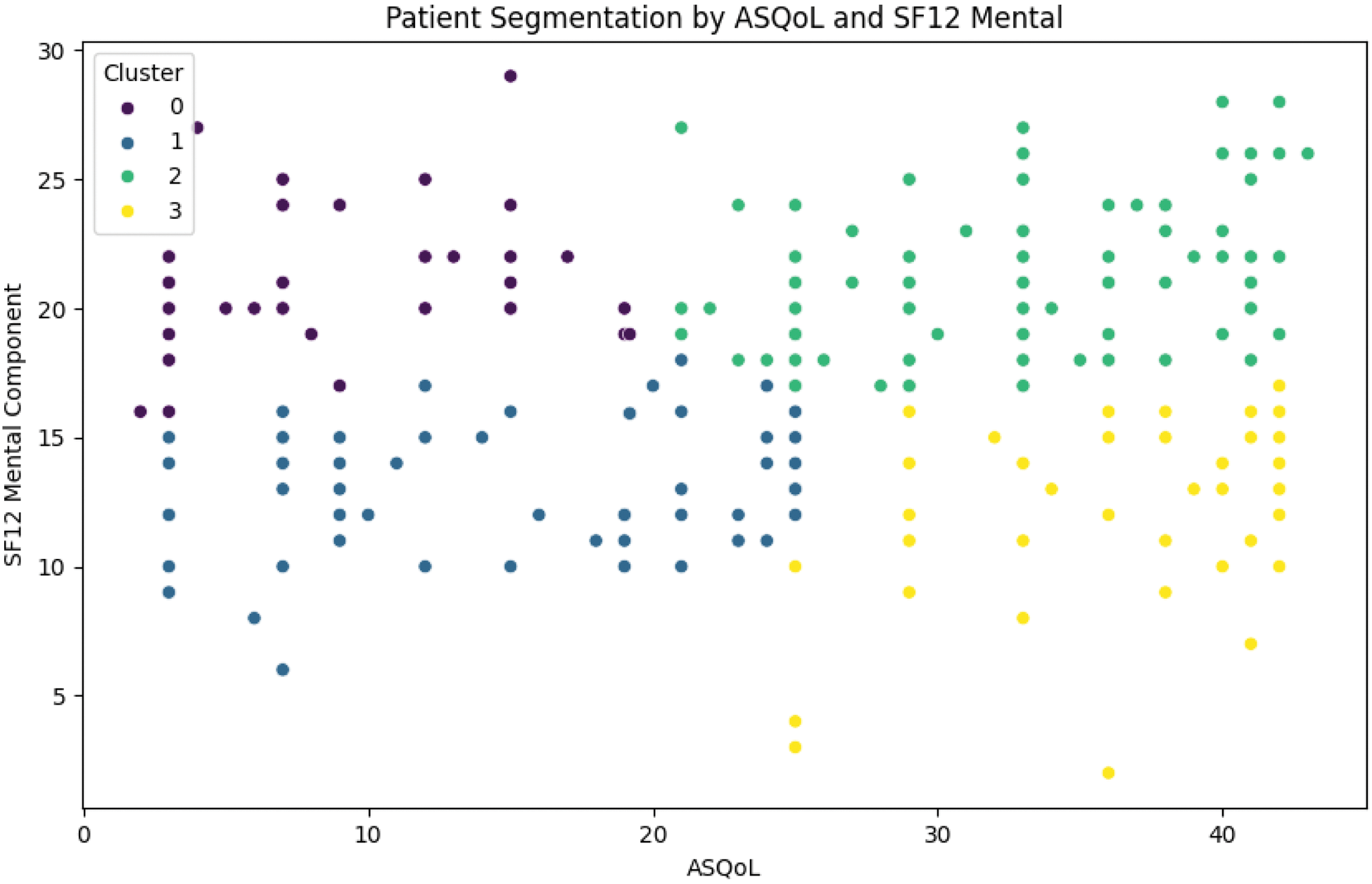
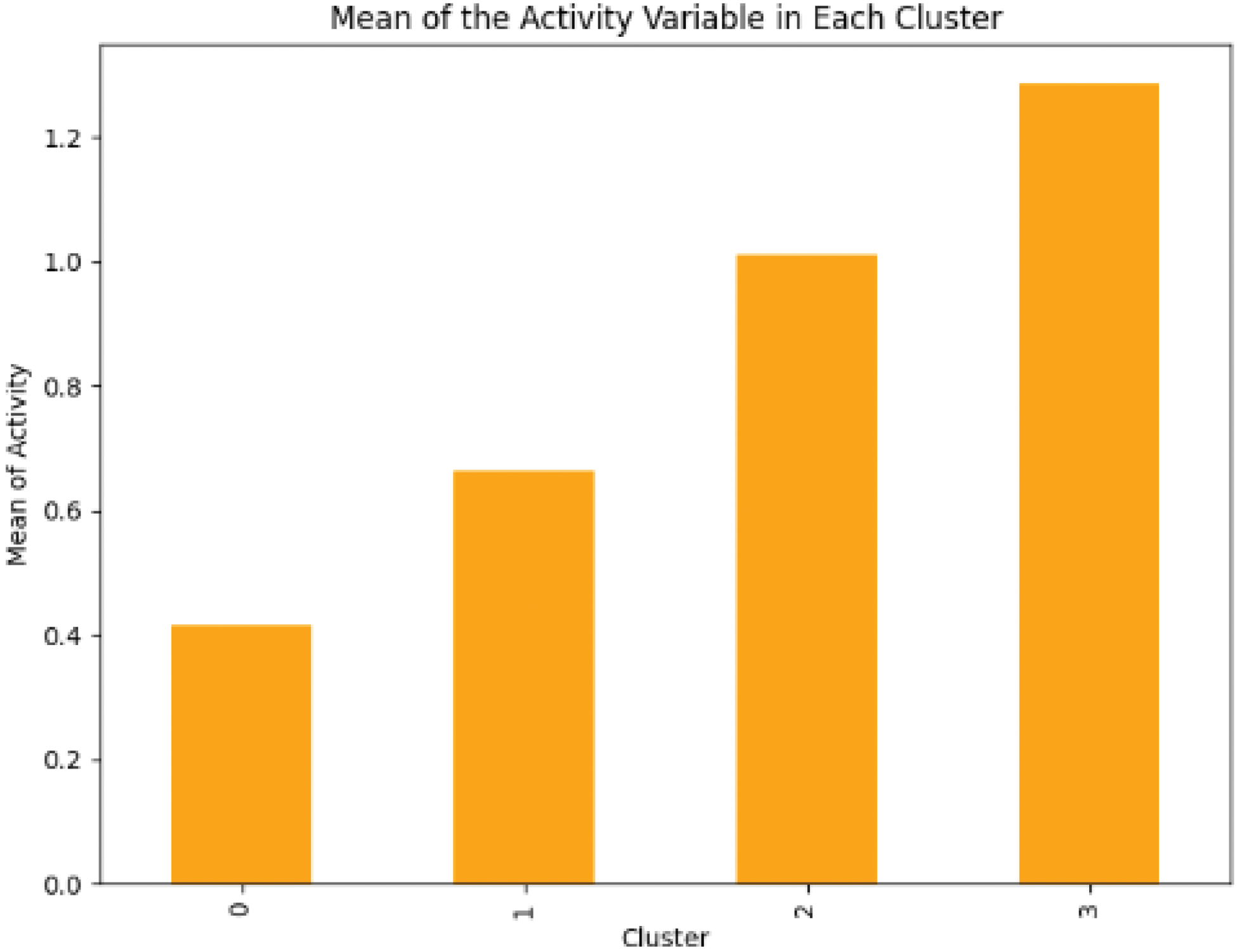
Methods: We combined data from two registries, REGISPONSER and RESPONDIA, resulting in a comprehensive dataset of 387 patients receiving anti-TNF therapy. During preprocessing, missing values were handled by imputing column means, and outliers were removed to ensure data integrity. To identify the most influential factors affecting disease activity, we applied five different feature selection methods: Mutual Information, Random Forest Importance, XGBoost Importance, Linear SVC, and Logistic Regression Coefficients. Each method provides a unique perspective; for example, Mutual Information captures non-linear relationships, while Random Forest and XGBoost highlight the variables that most effectively reduce model error. After normalizing the results, we summarized the findings in Figure 1, which ranks the most important predictors of inflammatory activity. For clustering, we standardized ASQoL (Ankylosing Spondylitis Quality of Life) and SF-12 Mental Component scores. We then employed the Elbow Method to determine the optimal number of clusters and selected k=4. K-means clustering was performed to categorize each patient into one of the four groups. We subsequently calculated the average inflammatory activity within each cluster, revealing distinct activity patterns that offer deeper insights into the heterogeneity of patient subgroups.
Results: While some prior research may have placed less emphasis on the mental health dimension (SF-12) when assessing anti-TNF therapy outcomes, our findings highlight the significance of this component. Figure 1 clearly indicates that mental well-being is among the most significant factors associated with inflammatory activity in spondyloarthritis patients. Whereas traditional analyses often center on demographic or lifestyle factors—age, physical labor, sex, or body mass index (BMI)—our study highlights the critical importance of mental health in understanding disease activity. To investigate this connection further, we conducted a two-dimensional clustering analysis using SF-12 and ASQoL scores. ASQoL specifically measures the impact of ankylosing spondylitis on a patient’s quality of life, and its integration with SF-12 Mental Component scores allowed us to classify patients into distinct subgroups, as illustrated in Figure 2. Our analysis revealed that Cluster 0, characterized by robust mental health and minimal disease burden, showed the lowest levels of inflammatory activity. In contrast, Cluster 3, featuring the worst combination of mental health and quality of life, experienced the highest levels of inflammation. These findings underscore a profound link between mental health and inflammatory states in rheumatologic conditions, offering valuable insight for optimizing patient care. One plausible explanation lies in the influence of psychological well-being on both the hypothalamic-pituitary-adrenal (HPA) axis and the autonomic nervous system—key mediators of immune responses. Poor mental health, marked by anxiety, stress, and depression, can stimulate the release of stress hormones (e.g., cortisol) and promote pro-inflammatory cytokine production. By comparison, positive mental health may mitigate stress effects, reducing both stress hormone release and inflammatory processes.
Conclusion: The interplay between mental well-being and quality of life substantially impacts inflammatory activity in patients with spondyloarthritis receiving anti-TNF therapy. These findings highlight the need for a holistic approach to treatment, one that transcends traditional physical and demographic considerations to include mental health support. Implementing interventions aimed at reducing stress, anxiety, and depression—conditions closely tied to heightened inflammation—could enhance disease management and improve patient outcomes. This more comprehensive view of rheumatologic care underscores the importance of addressing both the physical and psychological dimensions of health.
REFERENCES: NIL.
The most important features explaining inflammatory activity in patients treated with anti-TNF.
Cluster analysis of patients distributed by ASQoL vs mental component (Cluster 1) and physical component vs mental component (Cluster 2).
Activity level in cluster 1 and cluster 2.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (